| Contents | Previous | Next |
The structural health system relates to an individual's protective, physiological defense mechanisms (skin. bone. muscles, immune system). Alterations in structural integrity can give rise to potential alterations in other health parameters such as the cardiovascular and respiratory systems. Usual assessments in this area include skin breaks, joint and bone pain. strains, and fractures. Structural integrity also includes the immune system with potential for poor patient outcome when breakdown in the immune system occurs. Allergic reactions are one example of patient conditions addressed in this health system. The patient with acquired immune deficiency syndrome (AIDS) also has an alteration in the immune system that may be the etiology for the patient's primary presenting complaint. Patients with AIDS are evaluated according to their presenting complaint and triaged according to the significance of the problem in that health system. For example the patient with pneumocystis who presents with acute shortness of breath (SOB) would be triaged and managed according to the degree of dyspnea and compromise in the respiratory health system.
Case studies for this section were selected to address the wide range of presentations seen in the ED including alterations in skin and tissue integrity. breakdown of thermoregulation, and response of the immune system to an antigen.
| IMMUNE | MUSCULOSKELETAL | SKIN AND TISSUE |
| antigen-antibody | bones | entry-exit site |
| body temperature | exercise | incision |
| immunosuppression | gait | injury |
| infection | mobility | tumor |
| inflammation | muscles | wound |
| leukocytes | hygiene |
potential for infection
potential for altered body temperature
hypothermia
hyperthermia
ineffective thermoregulation
potential for trauma
disuse syndrome
potential for poisoning
impaired tissue integrity
impaired skin integrity
potential impaired skin integrity
impaired physical mobility
potential activity intolerance
bathing and hygiene self-care deficit
dressing and grooming self-care deficit
| Structural Health System | |||
| Level I | Level II | Level III | Level IV |
| Distal extremity injury, no gross deformity; circulation (C), sensation (S), mobility (M) intact; pain with motion, weight-bearing; client does not appear ill | Distal extremity injury, no gross deformity; C,S,M intact; with or without edema or ecchymosis; pain, but client does not appear ill |
Distal extremity injury, grossly deformed, moderate pain; C, S, M intact; client appears ill |
Distal extremity injury, gross deformity; pain is severe; C, S, M deficit; client appears shocky |
|
Laceration, superficial; C, S, M intact distal to injury; hemostasis has been or can be achieved by direct pressure; no other symptoms (sx); minor puncture wounds |
Laceration; C, S, M intact distal to injury; hemostasis has been or can be achieved by direct pressure | Laceration, deep or extensive,
arterial or uncontrollable venous bleeding; C, S, M deficit distal to
injury; wound grossly contaminated; significant crush or avulsion injuries;
trunk lacerations associated with evisceration; partial or complete amputation; open fracture; any laceration which is self-inflicted; puncture with foreign body |
|
| Minor bites, small punctures or scratches; localized insect bites |
Bite, minor tear or lacerations of face; insect bites, localized allergic response; hx snake or spider bite; no distress but wound obvious |
Bite, multiple lacerations, severe injury; insect bites-systemic allergic response or respiratory distress; history (hx) snake or spider bite; client appears ill: complains of pain | |
| Localized wound infection; localized cellulitis; patient appears well | Cellulitis or wound infection; client febrile; appears ill | Cellulitis or infection of face or periorbital area | |
| Thermal injury; mild discomfort; first-degree burns or sunburn comprising less than 10% of BSA | Thermal injury; moderate discomfort; first-degree burns greater than 10% but less than 25% of BSA | Any second- and third-degree burns; first-degree burns comprising greater than 25% of BSA; electrical burns; chemical burns | |
| Complains of feeling overheated after activity; temperature less than 102°F; VSS; no hx of metabolic disease; age less than 50 years of age; cramping of most-worked muscles after exercising; weakness, headache, nausea, oriented x3 | Heat exhaustion; core temperature greater than 102°F; recent history of exercise; oriented x 3; headache; anorexia; thirst; vomiting; may have orthostatic changes | Heat stroke; core temperature greater than 104°F; altered mental status; no perspiration present; hot, dry skin; tachypnea, tachycardia, hypotension | |
| Mild hypothermia; temperature 32-35 °C (90-95 °F) | Severe hypothermia; temperature 30° C (<90°F) | ||
| Allergic reaction—mild itching, diffuse reaction, mild distress | Same Sx as II with hx of previous reaction to similar substance noted | Respiratory distress, ingestion of known allergen | |
| Bee sting; mild local reaction; no hx of previous allergic reactions | Severe local reaction; bee sting greater than 24 hr old; no other associated symptoms | Severe local reaction with sting less than 24 hr old or with history of previous systemic allergic reaction | Respiratory distress after sting; generalized hives; gross swell¬ing of face |
| Fever less than 102°F | Fever more than 102° F, but less than 104°F; hx of flulike symptoms | Fever more than or equal to 105° F | |
| Partial laceration of tongue or cheek bite; minimal bleeding or injury | Puncture wound of soft palate; amputated tongue or tip of tongue; large laceration to cheek; hoarseness with hx of trauma to larynx | ||
| Multiple minor mouth sores; no history of immunosuppression | Multiple minor mouth sores; unable to take fluid for 12 hr with no orthostasis | Same Sx as II with clinical signs of dehydration | |
| Sore throat, swollen glands, laryngitis; temperature < 102°F; can swallow liquids | Sore throat, swollen glands, laryngitis; temperature > 102°F; can swallow liquids | Same Sx as II with inability to swallow liquids and orthostasis | Sore throat with stridor and drooling; difficulty breathing; bleeding post T and A |
| Mild toothache | Toothache, fever, swelling; moderate pain | Tooth knocked out; facial or jaw pain, bleeding | Multiple teeth knocked out; mouth injury with bleeding |
| Bleeding gums; not on anticoagulants | Moderate bleeding gums; not orthostatic; not on anticoagulants | Significantly bleeding gums; on anticoagulants | |
| Requests HIV testing; asymptomatic | |||
Susan C. Roberson, RN, MSN, CRNP
Tanya is a 23-year-old black female who presents alone to the ED with a chief complaint of a "boil" in her right arm/or 2 days. She complains of severe pain. feeling hoi and cold, sweating at night, and malaise. Whispering, she admits to daily intravenoususe of cocaine and heroin over the past 6 months. Tanya steals drugs from her husband. who is a dealer, but is not himself a user. She states her husband is unaware other addiction and that she is very afraid for him to find out since she believes he would then end their relationship. Tanya reports that she is not close to her family, has few friend'. and no one else she can turn to for support. She waited 2 days before coming to the ED fearing that her husband would find out about her drug-related illness. She stales she injected her last cocaine dose 4 days ago in the area where the boil now is. She drinks a quart of beer about 4 times a week and smokes half a pack of cigarettes a day. She has no regular medical provider. She has no known drug allergies and no other medical illnesses. She does not remember her last tetanus toxoid immunization. This is the first negative medical sequela of her drug use.
On physical exam Tanya appears uncomfortable and anxious. She is intermittently tearful. Her vital signs are temperature 100.1°F, respirations 20, pulse 100. and BP 136/88. She reluctantly rolls up the left sleeve of her blouse to reveal her boil. At her left antecubital space is a 3-cm-diameter fluctuant abscess surrounded by 3 cm of induration, erythema, and heat. Her epitrochlear lymph node is enlarged and tender. Auxiliary nodes are not palpable or tender. There is pain with flexion other elbow. She retains normal sensation and motor function of her hand and has normal radial and ulnar pulses.
Triage Assessment, Acuity Level III: Cellulitis and/or wound infection, patient febrile, appears ill.
Tanya was taken to the ED treatment area, and an evaluation was performed by a nurse practitioner. After her medical and social history were obtained, a physical exam was performed. Initial laboratory studies were completed, a problem Us! was compiled, and interventions were planned and implemented.
With the current epidemic of parenteral narcotic abuse, the urban ED nurse is frequently confronted with the overwhelming health care needs of the addicted patient. This patient is most likely to present for care of an infection, accounting for 27.5% of drug-related hospital admissions. The most common infections include cellulitis and the subsequent formation of an abscess at the site of injection (1).
An abscess is a localized collection of necrotic tissue, bacteria, and white blood cells, usually caused by the seeding of bacteria into a tissue (2). It begins as a focal accumulation of white blood cells in a space created by the breakdown of cellular materials or by the liquefication of necrotic tissue. Later, the abscess may become walled off by highly vascularized connective tissue that serves as a barrier to further spread (2). Enzymatic processes occurring in the abscess result in increased osmotic pressure, drawing water into the area and producing a large amount of pressure outward that increases the risk of bacterial spread along tissue planes or by way of the blood or lymphatic vessels (3).
The abscess can heal only after the pus has been released, since the presence of the pus perpetuates the inflammation. Without surgical intervention, the abscess may heal by proteolytic digestion of the cellular debris which is then resorbed into the blood. Alternately, the fluid may stay loculated in its fibrous capsule to create a cyst or may accumulate calcium salts to become a calcified mass. Most often, the abscess will burrow to the surface of the skin and rupture, thereby releasing the purulent material and causing extensive tissue damage (2). Surgical incision and drainage interrupts this process and is the mainstay of abscess care. Open drainage relieves the pressure inside the cavity: reduces the bacterial number; and, thus, toxin production; and allows the white blood cells to operate efficiently (3).
The bacteria may be seeded into the tissue by several routes: a contaminated needle or syringe (especially if "works" are shared among intravenous drug users), injection through contaminated skin. contamination of the drug with bacteria or fungi, mixing powdered drugs with an unsterile diluent (e.g., tap water or saliva), or by introducing oral flora when the user blows a blood clot out of a used needle (4).
Only a few studies have been conducted to identify the bacteria commonly involved in abscess formation related to intravenous drug use. These have produced varying results. Bacteria recovered from these abscesses are usually a mix of anaerobes and aerobes. with Staphylococcus aureus, p-hemolytic streptococcus, and oral flora predominating (5-7). Results of these studies vary with the geographic area studied. It is important for the practitioner to be aware of the specific bacteria that are frequently recovered from patients in the geographic area in which he or she is working, since antibiotic therapy should be initiated before culture results are known in order to control local cellulitis and bacteremia (6).
A quick and reliable method for determining the types of organisms involved in a specific abscess is the Gram stain. In general, the Gram stain shows one of three patterns: (1) white blood cells without bacteria, indicating a sterile abscess, (2) a mixed pattern of Gram-positive and Gram-negative rods and cocci, indicating a mixed aerobic and anaerobic infection, and (3) Gram-positive cocci in grapelike clusters, diagnostic of S. aureus. Additionally, anerobic organisms may produce a characteristic feculent odor, or air may be noted on the x-ray in the tissues surrounding the wound.
The history obtained by the nurse practitioner should include (1) the mechanism of injury if it is known, such as intravenous drug use. or a puncture wound to the foot by a nail; (2) in the case of a puncture wound, the material causing the wound, whether wood. metal, or glass, and the possibility of a foreign body in the wound if the material was rusty or was not removed intact; (3) the location of the abscess; (4) the duration and progression of the patient's symptoms: (5) any systemic signs possibly indicative of bacteremia, such as malaise, fever, chills, tachycardia; (6) the possibility of immunocompromise due to HIV infection, renal failure, diabetes or blood dyscrasia; (7) tetanus immunization status; (8) present medications: (9) drug allergies: (10) substance-abuse behaviors; and (11) in the case of substance abuse, readiness for treatment referral.
The physical examination of the patient should include vital signs: the location and size of the wound in centimeters; the presence of redness, swelling, induration, purulent material, or fluctuance; range of motion of the extremity involved; any vascular or neurological involvement: and the presence of lymphadenopathy or lymphangitis. Diagnostic testing of the patient may include a CBC with differential if the infection is extensive and/or associated with signs of systemic involvement, a needle aspiration at the site of cellulitis if the presence of an abscess is unclear, a wound culture, a radiograph for the presence of subcutaneous air or foreign body if indicated by the mechanism of injury, a Gram stain to aid the initial decision regarding antibiotic therapy, and/or blood cultures if the infection is extensive or associated with signs of systemic involvement.
Since the great majority of abscesses do not resolve spontaneously. but go on to burrow through the tissues to the surface causing extensive tissue damage, surgical incision and drainage (I and D) is most important in interrupting this process. Surgical I and D will allow the wound to heal by secondary intention. After I and D. the goal of wound care is to prevent the skin edges from closing prematurely over an unhealed cavity and to cleanse the wound of pus and debris allowing healing to progress. An abscess that extends into the subcutaneous tissues and that is associated with edema or induration will have a cavity after I and D and should be managed by copious irrigation, packed with a dampened gauze wick, and covered with a dry layer of gauze, creating a wet-to-dry dressing which separates the edges of the wound and prevents premature wound closing. This type of wound packing also serves to draw the purulent discharge from the wound by osmotic pressure (8-10). Burney (8) recommends irrigation 2 to 3 times daily and replacement of the wet-to-dry dressing until the wound begins to fill in and no longer produces purulent drainage.
In addition to surgical I and D the use of antibiotics may be required. Usually, in patients with normal host defenses, antibiotics are not needed. However, in the population of intravenous drug users. host defenses are often compromised and antibiotics are necessary. Antibiotics are further indicated in the presence of surrounding erythema and induration, lymphadenopathy or lymphadenitis. And / or systemic symptoms such as malaise, fever, chills, and tachycardia. The antibiotic of choice is determined by knowledge of the organisms commonly isolated from abscesses in the immediate geographic area. the Gram stain, the presence of a feculent odor or of air in the soft tissues as indicated on the x-ray, and by culture and sensitivity testing (9, 10). In the studies previously mentioned, culture and sensitivity tests revealed that penicillin alone covered most of the organisms involved and that a first-generation cephalosporin covered all the organisms involved (5-7). Once antibiotic therapy has been initiated. cellulitis should resolve within 36 to 48 hrs. Tetanus prophylaxis should be updated with a tetanus/diphtheria booster since Tanya did receive the three initial doses as required for school attendance but does not remember receiving a booster within the past 5 years (11).
Effective treatment of these abscesses also involves immobilization, elevation, and heat. If the wound is in a mobile body area such as near a joint, immobilization will help prevent muscle movement from forcing bacteria into the lymphatic or venous systems. Elevation above the level of the heart helps to prevent dependent edema promoting host resistance by maintaining a normal blood supply. Heat increases the blood supply and also helps to localize the infection.
Follow-up is required within 24 hr of initial therapy to monitor resolution of any systemic symptoms or cellulitis and to perform the initial dressing change. Based on this follow-up assessment the provider will determine how the individual patient should be followed. If appropriate, the patient or a family member is taught to provide wound care at home.
Diagnosis: Anxiety related to the treatment of her illness and the possibility of pain
Desired patient outcome: The patient will describe a basic understanding of her illness and the treatment involved, and the measures which will be employed to help reduce her pain. The patient will demonstrate a reduction in anxiety; for example, she may cease crying or clenching her fists and assume a more relaxed posture.
Diagnosis: Pain related to the I and D procedure and subsequent wound care procedures
Desired patient outcome: The patient will state that her pain is minimized or controlled; the patient will not exhibit nonverbal cues of discomfort.
Diagnosis: Altered family process related to the patient's poor relationship with her husband
Desired patient outcome: The patient will begin to formulate a plan to address her dysfunctional relationship in regard to her illness.
Diagnosis: Impaired skin and tissue integrity related to local infectious process
Desired patient outcome: The patient's cellulitis will resolve and the abscess will heal without sequela.
Diagnosis: Disturbance in self-esteem related to the patient's sense of moral failure in abusing drugs
Desired patient outcome: The patient will verbalize a realistic view other illness without moral condemnation of self. She will identify strengths and other positive aspects of herself. She will describe ways in which she will assume responsibility for her own health and rehabilitation.
Diagnosis: Knowledge deficit related to self-care of her wound
Desired patient outcome: The patient will verbalize an understanding of discharge instructions and give a return demonstration of abscess care.
Tanya's fear and anxiety regarding her treatment can be greatly reduced by the nurse's therapeutic use of self. The nurse should spend time with the patient to develop trust and rapport. Procedures should be explained carefully so that the patient is prepared and her fear of the unknown is reduced (12). The cause of the abscess and its treatment and prognosis are described. If possible, the nurse should be at the bedside during the I and D procedure to offer encouragement and support.
The patient's pain should be addressed by the nurse, first assessing the patient's response to pain and then providing an ongoing assessment throughout the ED visit. The patient should be positioned as comfortably as possible, in an area with a comfortable temperature. Analgesics should be administered as ordered by the medical provider prior to the I and D procedure. The nurse should be sensitive to the possible dependency needs of the patient and may determine on an individual basis that therapeutic touch is helpful (12). Tanya should be informed that she can expect her pain to be greatly reduced after the I and D procedure. For pain reduction on return visits during dressing changes, Tanya should be instructed to take an oral analgesic prior to the visit. She should maintain elevation of her arm above the level other heart and keep her splint on to help control the pain.
The nurse's therapeutic use of self can again be employed to address Tanya's lack of self-esteem. Tanya's self-esteem is enhanced when the nurse is able to communicate esteem and concern for the patient through conversation and behavior. A nonjudgmental approach should be maintained throughout the ED visit. The problem of drug addiction as opposed to moral failure should be distinguished by the nurse for this patient since it seems to be of major concern to her. The nurse can help the patient identify strengths she possesses which will aid her to pursue her recovery. Tanya would benefit from referral to a mental health provider or a drug rehabilitation program that can address her lack of self-esteem.
As with Tanya's lack of self-esteem, her dysfunctional family relationships cannot be adequately addressed during her brief visit to the ED. During this visit it is desirable to help Tanya begin to formulate a plan to deal with the immediate crisis of the effect other illness on her family relationships. Referral to another source for ongoing care is necessary.
The disruption of Tanya's skin and tissue integrity by the abscess and the I and D procedure itself is best managed through education regarding wound healing and wound care procedures. Tanya and a friend or family member must be taught to continue her wound care at home, and observe the wound for signs and symptoms of worsening infection. A return demonstration by the patient is recommended. If a family member or friend is not available, a visiting nurse referral is made to provide dressing changes. Tanya should be given information regarding analgesics and antibiotics as prescribed. She should also understand the importance of follow-up wound checks and have a written return appointment schedule.
Suzanne P. Hangasky, RN, BS, CRNP
Lisa is a 15-year-old black female who comes to the ED accompanied by her aunt. She is seeking care for a wound on her left hand and a "bruise" on her right shoulder sustained during an altercation with another teenager 8 hr earlier today. Further questioning reveals that both injuries are human bites. She has done no home wound care. Lisa is a young woman of average stature and build with normal vital signs. There is a puncture wound over the proximal interphalangeal joint of her left middle finger with a small amount of edema and tenderness but no erythema or heat. Lisa has adequate sensation in her finger and hand. There is a 3- by 4-cm ecchymotic region on her right shoulder with tooth imprints at the border but the skin is not punctured. Lisa is unable to remember her tetanus immunization status. She denies pas! medical problems and any history of allergies or intravenous drug abuse.
Triage Assessment. Acuity Level III: Human bite to the hand over 6 hr old no distress, wound obvious.
An x-ray of her left finger is obtained and a CBC with differential is sent.
The number of human bites occurring annually is estimated at greater than 60 bites per 100,000 persons (1). Many of these injuries are not evaluated because people are embarrassed about the circumstances surrounding the injury (2). For this same reason, the patient may report the bite as a wound occurring from another type of injury. Those persons who seek early treatment do so because they are concerned about their immunization status or because the wound is serious enough to have developed complications (3).
Most human bites occur as a result of fighting, although self-inflicted bites from thumb sucking, seizures, or falls are reported (1). Forty to seventy-five per cent of human bite injuries involve the hand; other frequent sites are the arms and breasts (1.4. 5). The incidence of complications is 25 to 50% (1,5) with the greatest number occurring in bites to the hand. It is interesting to note that the peak incidence of human bite injuries occurs in warm weather and on weekends (1,6).
The human jaw delivers a crushing force, and teeth can cause puncture wounds when a bite occurs. These cause devitalization of tissue and an inoculation of the area h microorganisms from the mouth and skin. When the bite occurs over a clenched fist, the joint is not covered by the dorsal expansion hood and the joint space is easily accessible to puncture. When the finger is extended again, the entrance to the joint may be covered and sealed off. The resulting hypoxic area allows for the proliferation of anerobic organisms. The crushing force delivered may also cause a fracture of the underlying bone. Complications which can develop as a result of the injury include septic arthritis, tendon injury, cellulitis and osteomyelitis. Signs of infection begin in 6 to 12 hrs and spread proximally. The length of time elapsing between injury and treatment is the most important factor in preventing complications (4, 5).
The microbiology of the wound is important in the determination of antibiotic therapy for the patient. The bite forces bacteria from the skin and oral cavity into the resulting wound. Normal oral flora, more than skin flora, are found on wound cultures (7). The bacteria grown in cultures from human bite injuries are both aerobic and anaerobic. Frequently found aerobic microorganisms are Staphylococcus aureus, Eikenella corrodens, and group A streptococci (3, 7. 8). B-Lactamase activity is noted in 41% of cultures (8). Eikenella corrodens. which is present in 20 to 38% of clenched-fist injuries, acts synergistically with a-hemolytic streptococci (6, 8). This polymicrobial combination causes a severe infection which is hard to eradicate.
It is possible to inject viruses and spirochetes with the human bite. Infectious diseases such as hepatitis, scarlet fever, tuberculosis, syphilis, and herpes may be transmitted (3,6). Since HIV has been found in saliva, in theory, it could be transmitted with a human bite although no cases have been reported (3, 9).
Nursing diagnoses for this patient involve both the injury and the behavior that led to the injury.
Diagnosis: Impaired tissue integrity related to bite injury
Desired patient outcome: The patient will not develop complications of infection, arthritis, osteomyelitis, or cellulitis as evidenced by healing tissue, and absence of drainage, pain. and fever.
Diagnosis: Pain related to tissue ischemia and infection at site of bite injury
Desired patient outcome: The patient will state that there is relief or reduction in pain to the point that it is tolerable. The patient will not exhibit nonverbal cues of pain.
Diagnosis: Impaired social interactions related to emotional response to conflict leading to verbal and physical assault
Desired patient outcome: The patient will describe strategies to avoid or minimize conflict, such as the use of self-control to de-escalate a potentially violent exchange.
Diagnosis: Knowledge deficit related to wound care and importance of follow-up management
Desired patient outcome: The patient will verbalize an understanding of the discharge instructions; the patient will give a return demonstration of correct wound care technique: the patient will state date and time of follow-up appointment and describe how she will arrange to keep the appointment.
As with any injured person, the ABCs of assessment should be the first priority. The wounds sustained may be impressive, but the patient must be physiologically stable.
The patient's pertinent history should include how and when the injury occurred, the number of bites sustained, past medical history. and any risk factors that would further increase the potential for wound infection such as diabetes mellitus or immunosuppression. The patient's current immunization status is also needed.
Patient assessment (after the ABCs) should include inspection of each wound. The neurovascular and motor status of all tissue distal to the bite(s) is assessed by looking for the 5 p's: pallor, pain. pulselessness, paresthesia, and paralysis. It may be helpful to diagram multiple wounds on a flowchart noting the location and description of each bite: abrasion, laceration, puncture, size, any ecchymosis. edema. erythema. or heat.
A CBC with differential is ordered by the physician and sent to assess any rise in the WBC count that would indicate infection. The x-ray of wounds over bones are ordered to determine if there is any damage to the underlying bone or the presence of any tooth fragment (1.8. 10).
The need for pain management varies with each patient and is related to the extent and location of the injury and the presence of edema and inflammation. Elevation and functional positioning may reduce the amount of discomfort in an extremity wound. Some patients may require analgesics. If the patient is anxious about her injury, potential procedures, or admission, this may heighten the pain. Reassurance, education, and emotional support throughout the ED visit will help to reduce the level of anxiety.
Wound cleansing is essential. Aggressive management is necessary to prevent infection and to provide good cosmetic and functional results (8). All wounds need to be topically cleansed. Normal saline scrubbing removes most bacteria and does not injure tissue. Other cleansing agents such as 1% povidone-iodine may irritate already damaged tissues. Superficial wounds, such as Lisa's shoulder wound. require no further cleansing (10), but puncture wounds and lacerations (especially those on the hand) require debridement (1. 3. 8). A regional block or other local anesthetic may need to be administered for the procedure. Infected wounds should be cultured. Extremity injuries require immobilization and elevation (1.3). Opinions vary on the need for hospitalization as opposed to outpatient management (2. 5, 9, 10). Considerations include the severity, age, and site of the wound and predicted patient compliance with follow-up care.
Antibiotic therapy is initiated if the wound exhibits any signs of infection or is on the hand, or if the patient has other health problems that put her at risk for complications (9). Prophylactic antibiotic therapy may be used because a human bite is considered to be a contaminated wound. If the patient is to be discharged, the first dose of antibiotic may be given intravenously to obtain a therapeutic level more expediently. Penicillin's are the most active agent against oral inoculates although some bacteria are resistant to the drug (8). Penicillinase-resistant antibiotics or a cephalosporin can be given concurrently to cover those bacteria (1, 8). For the penicillin-allergic adult patient, tetracycline or erythromycin are alternatives (1. 3. 9). A combination of amoxicillin and clavulanate potassium is effective for all human bite pathogens (3).
Tetanus diphtheria or toxoid is recommended if the patient has not had a booster in the past 10 years (2, 6). Other immunizations or medications may be ordered by the physician if the biter is known to have a communicable disease.
Patient education is of the utmost importance to assure compliance and an optimal outcome. The patient needs to be instructed in proper administration and side effects of the antibiotics and pain medications prescribed. Signs and symptoms of infection must be taught, immobilization and elevation clearly defined, and any wound care instructions reviewed and demonstrated. Return demonstration is a necessity if there is potential for serious knowledge deficit or non-compliance. The need for follow-up care must be stressed: when. where, and with whom, as well as the complications that may ensue if the wound becomes infected or progresses. All instructions should be specific, in writing, and verbally reviewed.
Lisa was seen by a plastic surgeon in the ED because her hand and finger were involved. He administered a regional block for debridement and exploration of the finger wound. A wound culture was obtained. Lisa's hand was splinted and elevated in a Curtis bag. The shoulder wound was scrubbed with gauze and normal saline. A tetanus diphtheria immunization was administered and an intravenous line initiated for administration of pencillin and a cephalosporin. Because the wound was overlying the joint and showed early signs of infection, Lisa was admitted to the hospital for further antibiotic therapy and observation.
Patient education in the ED was aimed at Lisa's understanding of the potential for complications (i.e., the reason for her admission) and to introduce the concept of problem resolution without physical assault. The discharge teaching plan from the hospital should include the information reviewed above and should also assist Lisa in developing strategies for alternative means of conflict resolution.
Sharon A. Childs, RN, BSN, CEN
James, a 44-year-old, mildly retarded, Caucasian male, with a history of hypertension and diabetes mellitus, was brought to the ED by ground ambulance. He had been standing on the street corner waiting to cross when he was struck by a car.
James was designated as a priority 2 case by the paramedics. His Glascow coma score was rated at 15/15. Peripheral intravenous access with 1000 ml D5/Ringer's lactate was established. Oxygen was provided by non-rebreather mask, and spinal immobilization was initiated. Gross deformity was evident in James' lower extremities. He was unable to move either limb. Pedal pulses were not palpable. James was splinted with two metal, long leg, posterior splints by the paramedics and was immediately brought to the treatment area of the ED for further assessment and treatment.
Triage Assessment, Acuity Level IV: Distal extremity injury, gross injury with cardiovascular and motor deficit.
While in the treatment area of the ED, James' vital signs were BP 180/100. pulse 104. and respirations 24. His lab values were within normal limits. His cardiopulmonary and neurological findings were unremarkable. X-rays revealed positive deformity to both lower extremities. Ecchymosis was present over the proximal tibia His left foot was warm. with a positive dorsalis pedis pulse by Doppler: his right leg was deformed and tense with an extensive hematoma to the anterior and lateral portions of the leg. Right posterior tibial and dorsalis pedis pulses were obtained by Doppler, but found to be diminished. Right popliteal pulse was absent. James was unable to evert his right ankle. However, sensation was intact to the right peroneal nerve distribution. Left peroneal nerve sensibility was intact.
James was diagnosed as having bilateral proximal tibia and fibula fractures, a right tibial plateau fracture, and a posterior fracture and dislocation of the right knee. The fractured and dislocated right knee was causing occlusion to the right popliteal artery at the level of the knee.
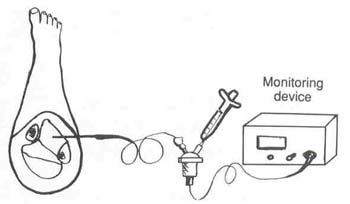
During the assessment, evaluation, and treatment phase in the ED. James was complaining of increasing right lower leg pain. Narcotic analgesia had afforded lii-tie relief of his pain. It was becoming evident that the mechanism and extent of injury was precipitating one of the most serious orthopedic complications— compartment syndrome. Compartment pressures were obtained by Wick catheter (1) (Fig. 5.3.1). Anterior compartment pressure was recorded to he 60 mm Hg: superficial posterior compartment pressure was 48 mm Hg. James was immediately prepared and taken to surgery for compartmental decompression fasciotomy. open reduction and internal fixation of fractures, and exploration of the popliteal artery and possible vascular bypass.
Figure 5.3.1.
Insertion of the Wick catheter. (From Pradka L: Use of the Wick catheter for diagnosing and monitoring compartment syndrome. Orthop Nurs 4(4):17-18. 1985. Reproduced with permission of the publisher, Orthopaedic Nursing, official publication of the National Association of Orthopaedic Nurses.)
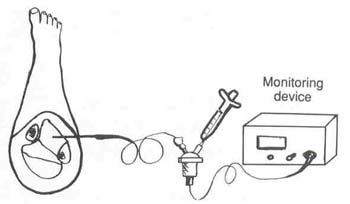
When tissue injury occurs from phenomena such as trauma and burns (thermal or chemical), biochemical changes activate an inflammatory response. At the cellular level, macrophages and neutrophils are stimulated into action. There is also liberation of many tissue products which enhance the inflammatory response. Some of these products include histamine, bradykinin, serotonin, and prostaglandin and reaction by-products from the complement and blood-clotting systems. Damaged vessels in the ischemic muscle dilate from the effects of histamine and these other tissue products. This dilation affects the mean capillary pressure. Hydrostatic filtration pressure becomes greater than the oncotic pressure of the plasma colloids causing plasma proteins and fluid to shift to the interstitium. With the accumulation of fluid in the interstitium, an increase in the hydrostatic pressure inhibits adequate drainage from the venous end of the capillary. The disequilibrium of the pressure gradients within the muscle hinders microvascular perfusion to the tissues. The cycle of edema. increased tissue pressures, and decreased perfusion leads to ischemia with a repetitive sequence until signs and symptoms of compartment syndrome are evident (2-8). Compartment syndrome can be defined as a local condition in which edematous and ischemic muscle is confined within an osteofascial compartment (Fig. 5.3.2).
TIP: Fracture of the lateral condyle or plateau of the tibia is a result of blunt trauma to the lateral aspect of the knee. While the feet remain in a planted and fixed position. severe abductive valgus strain is placed upon the knee resulting in subluxation or complete dislocation of the joint (9). This type of injury is commonly referred to as a "bumper fracture" and frequently results in compartment syndrome.
Systemic evidence of muscle necrosis can include myglobinuria, renal failure, acidosis, and hyperkalemia with resultant cardiac involvement (12, 13). Unless intervention to release the pressure is promptly instituted, tamponade of perfusion to the tissues will result in muscle and nerve ischemia which will cause permanent and irreparable damage.
The patient who has sustained significant soft tissue injury is a candidate for developing neurovascular compromise. The following are the pertinent nursing diagnoses for this patient.
Diagnosis: Pain related to muscle ischemia, fracture, and neurovascular compromise
Desired patient outcome: The patient will describe relief of or experience significant reduction in the sensation of pain.
Diagnosis: Alteration in peripheral tissue perfusion related to localized tissue edema; obstruction of microvascular circulation causing compromised neurovascular status
Desired patient outcome: The patient will maintain normal compartment pressures as evidenced by compartmental readings of 20 mm Hg or less; the patient will regain distal pulses, have reduction in lower extremity pain, and report decreased numbness and tingling.
Diagnosis: Impaired mobility related to multiple fractures
Desired patient outcome: The patient will be free of preventable complications of immobility (e.g., pneumonia, decubiti, and renal calculi); the patient will perform mobilization activities with assistance.
Diagnosis: Impaired tissue integrity related to fractures, fasciotomies, and surgical wounds
Desired patient outcome: The patient will have normal progress of tissue healing evidenced by clean wound and pink, healthy tissue.
Diagnosis: Potential for infection related to impaired tissue integrity
Desired patient outcome: The patient will not experience signs or symptoms of infection as evidenced by temperature < 100.4°F; wound drainage will not be odoriferous.
Diagnosis: Knowledge deficit related to limited understanding of treatment modalities, and mild mental retardation
Desired patient outcome: The patient will describe a basic understanding of treatments; the patient will demonstrate the ability to follow instructions related to the treatment plan.
Figure 5.3.2.
Extremity osteofacial compartments.
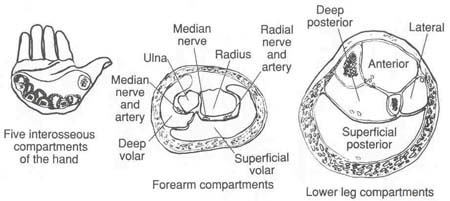
Table 5.3.1 Associated Signs and Symptoms Seen in Compartment Syndrome
| Compartment | Areas of Sensibility Deprivation | Muscular Motor Weakness | Pain on Passive Flexion or Extension | Region of Muscle Tenseness | |
| Forearm | |||||
| Dorsal | None | Extension of wrist and fingers | Flexion of wrist | Dorsal forearm | |
| Volar | Ulnar and median nerve distribution on palm side of fingers | Flexion of wrist and fingers | Extension of wrist and fingers | Volar forearm | |
| Hand | |||||
| Interosseous | None | Interosseous muscles | Abduction and adduction of the metacarpal joints | Dorsum of hand between metacarpal joints | |
| Lower leg | |||||
| Anterior | Web space of great toe |
Toe extensors and tibialis anterior |
Toe flexion | Anterior aspect of tibia | |
| Lateral | Dorsum of foot | Peroneal muscles | Inversion of foot | Lateral aspect of lower leg | |
| Superficial posterior | None |
Soleus and gastrocnemius |
Dorsiflexion of foot | Calf of leg | |
| Deep posterior | Sole of foot |
Toe flexors and tibialis posterior |
Toe extension |
Distal midportion of leg between Achilles tendon and area of tibia |
|
| From Matsen FA Compartment syndrome: A unified concept Clin Orthop Relal Res 113.8-14. 1975; Copyright JB Lippincott (Harper & Row) | |||||
Nursing interventions in James' case as well as for all patients who are suspect for developing musculo-neurovascular compromise (compartment syndrome) focus primarily on astute neurovascular assessment.
TIP: Pain that is unrelieved by narcotic analgesia and expressed as being continual and unrelenting or pain that is elicited by passive stretch of the muscles in the involved compartment is pathognomonic for compartment syndrome.
Assessments of the neurological status of the upper and lower extremities are performed by the nurse. Table 5.3.2 illustrates the assessment criteria.
Vascular assessment is performed by using the Doppler for pulse assessment, checking nail beds for capillary refill time (brisk, diminished, absent), and evaluating temperature (warm. cool. cold) and appearance (pink, cyanotic, pallor, mottled) of the skin (5. 7).
The medical intervention that is commonly used to detect increased pressure in the affected compartment is intracompartmental pressure monitoring. The procedure is useful in detecting subtle pressure changes even in those persons who because of communication problems (aphasia, comatose, intoxication) or paralysis are not cognizant of the impending situation (4).
Several techniques are available to measure and monitor compartment pressures. Techniques include needle manometer, the Slit catheter, Wick catheter, and the solid state transducer intracompartmental (STIC) pressure monitor system (1,4, 15-17). The basic concept for all these methods is the detection of increased pressure within the tissue compartment.
Nursing responsibilities include assisting with insertion of the monitoring device, maintenance of the system while it is inserted. and monitoring of the readings if continuous pressure monitoring is ordered (1). Pain will be relieved by pharmacological and nonpharmacological interventions. Providing physical support and patient comfort by means of chemical analgesia (giving medication and observing the effects), patient positioning, and the nurse's therapeutic use of self (touch and verbal communication) are all important (1.4. 17-19).
Continued neurovascular assessment in conjunction with the measurement of compartment pressures with accurate documentation of findings is crucial in the care of the patient who is being monitored for compartment syndrome. Untoward changes should be reported to the physician immediately.
Compartment pressures of O to 20 mm Hg are normal: pressures of 21 to 30 mm Hg are indicative of insidious compartment syndrome (decreased microvascular perfusion), and pressures greater than 40 mm Hg indicate compartment syndrome (ischemic necrosis).
Table 5.3.2 Assessment Criteria for Neurological Status
| Nerves | Sensorya | Motorb |
| Upper Extremity | ||
| Radial | Test for sensation at the dorsal web space of the thumb. Rationale: Radial nerve discrimination is assessed by this area of sensibility in the hand. | Have patient hyperextend wrist and / or hyperextend thumb. Rationale: Inability to perform strong movement is indicative of potential radial nerve injury. When the radial nerve is significantly damaged ½ to ¾ of the hand’s power is lost. |
| Ulnar | Test for sensation on the volar (palmar) surface of the tip of fifth (small) finger. Rationale: Ulnar nerve discriminately assessed for in this area of the hand. | Have patient adduct fingers: Motor capability necessary for normal hand functioning; pinching. |
| Median | Test for sensation in the volar (palmar) surface at the tip of the index (second finger). Rationale: Integrity for main sense of touch to hand is elicited here. | Have patient consecutively oppose each finger of hand to the thumb. Rationale: Median nerve is the main nerve of precise functioning (pronation of the hand). |
|
Lower Extremity |
||
| Peroneal | Test sensation at dorsal web space of first (great) and second toes. Rationale: Nerve innervation can be precisely assessed in this area. | Ask patient to dorsiflex ankle/foot. Rationale: Motor functioning is assessed in this one maneuver. |
| Tibal | Test sensation to the sole of the foot. Rationale: Sensibility is discriminately assessed in this area. | Ask patient to plantarflex foot. Tibial nerve integrity gauged by ability to plantarflex. |
| Femoral | Test for sensation on the anterior thigh. Rationale: Nerve innervation best assessed on anterior thigh. | Have patient do straight leg raise. Rationale.: Motor functioning interrupted if unable to straight leg raise because of decreased power. |
| a Sensibility is graded as normal, numbness, tinging, diminished, or absent sensation. | ||
| b Motor ability is classified as normal, decreased, or absent. | ||
TIP: Do not elevate extremity. Elevation above the level of the heart is contraindicated because venous drainage is already impeded because of edema. Elevation would further decrease arterial perfusion and increase ischemia.
After the fasciotomy, the nurse's dynamic role in continued neurovascular assessment is necessary. Postfasciotomy complications are prevented by continued assessment of the wound, observing for local and systemic signs and symptoms of developing infection, and following the medical regimen, including dressings, antibiotics, and pressure monitoring as indicated.
Cathy Robey-Williams, RN, MS, CCRN
Jason and his friends were walking home from basketball practice when they noticed a bonfire on the frozen river. A few of their friends were out in the middle ice-skating. When walking with his friends toward the bonfire to socialize, Jason fell through the ice The rest of the group stood frozen with fear. When Jason did not return to the surface. one of his friends ran to shore and called 911 from the closest house.
The first emergency unit to arrive on the scene was an engine crew who placed a ladder on the ice out to the hole near the bonfire. The fire was extinguished and the other teens instructed to return to shore following the ladder. Ten minutes later rescue divers arrived and began their search pattern. After 12 min, Jason was brought to the surface. Basic life support was begun as Jason was slid back to shore. He was immediately placed into the awaiting helicopter and orally intubated with a no. S endotracheal tube. The flight to the closest trauma center took 3 min. During that time Jason's wet clothing was removed and he was wrapped in a blanket.
The ED was alerted that a 16-year-old male weighing an estimated 80 kg had fallen through the ice. The patient would be arriving in full cardiac arrest, intubated with basic cardiac life support initiated. The ED'S resuscitation team was alerted and began to prepare for the child's arrival. The OR staff were also notified.
Triage Assessment, Acuity Level IV: Cardiopulmonary arrest and profound hypothermia.
Upon arrival to the ED, basic life support is continued. Healed humidified oxygen is initiated via ambu bag. Two large bore intravenous lines are started, and warmed NS is infused at a temperature of 40°C via a rapid warmer-infuser device. Jason initial rectal temperature was 26.6° C. During the first 15 min of the resuscitation effort Jason has an additional 2° C drop in temperature. A nasogastric tube is passed and warm NS lavages begun. Urethra! and recta! Foley catheters are introduced and warm NS enemas initiated. Several doses of epinephrine are administered, without response from the heart. Jason is therefore taken to the OR and placed on heart-iung bypass. After his blood is warmed to 32.2°C, an idioventricular rhythm is noted via ECG. Epinephrine increases the rate to 40 beats per minute. Jason is maintained on bypass until his temperature reaches 35.5° C. At that time Jason's HR is 62. BP 100/60, and he is mechanically ventilated. He is then transferred to the intensive care unit for continued monitoring.
Central blood temperature receptors located in the anterior hypo-thalamus compare core body temperature to messages received regarding peripheral or shell body temperature. As blood circulating to the brain cools, the hypothalamus sends messages to the adrenal medulla to release catecholamines and directs neural pathways to vasoconstrict. The hypothalamus can also stimulate the body to shiver which can produce the same amount of heat as maximum exercise for limited periods of time (1). These compensatory mechanisms are usually effective during normal cycles of temperature change such as going outdoors during the winter months. When these compensatory mechanisms are ineffective, such as during intense or prolonged exposure to cold, the brain cools and cerebral 0; consumption decreases. Cerebral blood flow then decreases and sludging and a decreased level of consciousness occur. At a core body temperature below 30°C consciousness is lost, reflexes decrease, pupils dilate, and the body lies in a near dormant state.
The respiratory system also attempts to compensate during cooling. Bronchodilation occurs and the oxygen-hemoglobin dissociation curve shifts to the left. Cessation of breathing occurs at temperatures around 24°C. The GI tract becomes silent at a temperature of 35s C. The genitourinary tract is affected by an increase in serum glucose as the sympathetic nervous system is stimulated, thus causing the adrenal glands to secrete catecholamines. Elevated serum glucose combined with inadequate levels of insulin produces glucose excretion in the urine and a concomitant diuresis of fluid (1).
The cardiovascular system is the primary organ system affected by hypothermia. Cooling of Purkinje fibers below 25°C decreases resting transmembrane potential, depresses action potential height. slows conduction velocity, prolongs absolute and relative refractory periods, and slows the rate of spontaneous depolarization. In humans cooled for cardiac surgery, ventricular fibrillation occurs at 23'C and asystole occurs at 20°C (2).
Metabolic changes that occur during hypothermia include depletion of body stores of fat, carbohydrates, and protein: stimulation of catecholamines and glucocorticoids; reduction in insulin activity: and reduction in liver function secondary to inhibition of the enzyme hexokinase. Initially hypothermia causes a shift of fluid to the extracellular compartment and induces diuresis creating relative hypovolemia. At temperatures below 25°C water moves into the cells and fluid is sequestered in the capillaries which results in hemoconcentration and increased blood viscosity (3, 4). Prolonged clotting times are evident at 20°C. Leukopenia and thrombocytopenia also occur and are a result of sequestration of cells in the liver and spleen (4). Table 5.4.1 correlates temperature and clinical manifestations of hypothermia.
Until the central body organs are rewarmed, pharmacological and electrical therapy are ineffective. In fact, giving cardiac arrest drugs to a hypothermic patient can be deleterious. As the body rewarms. the drugs that have been dormant because of the cold state are then activated and begin affecting the body concurrently. At 28 °C the heart rate slows to 50% of normal. Between 20 and 28 °C the heart rate drops down to 20% of normal until asystole occurs, usually at 20°C. The risk of dysrhythmias increases after temperatures drop below 28°C. This is due to decreased flow to the myocardium secondary to vasoconstriction and viscosity of blood. Ventricular fibrillation is a common complication during this time precipitated by hypocapnia. alkalosis, rewarming (especially surface rewarming). and physical manipulation of the heart. Sometimes movement of the victim's body or endotracheal intubation will stimulate ventricular fibrillation (2, 4). Ventricular fibrillation is resistant to defibrillation and antiarrythmic drugs below a core temperature of 28°C (5).
Table 5.4.1 Correlation between Temperature and Clinical Symptoms
| Temperature, °C | Clinical Manifestations |
| 35-37 | Cold sensation Moderate shivering Loss of coordination |
| 32-35 | Violent shivering Slurred speech Confusion Amnesia Tachycardia Vasoconstriction |
| 28-32 | Decreased shivering Muscle rigidity Bradycardia Atrial fibrillation Cyanosis Hypoventilation Systemic lactic acidosis |
| 25-28 | Hypotension Stupor Coma Irregular pulse Ventricular fibrillation if heart stimulated Cold diuresis |
| 21-25 | Spontaneous ventricular fibrillation Areflexia Pupils fixed, dilated No spontaneous movement Apnea Asystole |
| From Jonston JB:Hypothermia: assessment and intervention. Emerg Nurs Rep 3(8):5, 1988. Reprinted with permission of Aspen Publishers, Inc., @ November 1988. | |
The definition of hypothermia is a core temperature that is less than 35 °C. Heat loss occurs through four physical mechanisms. Conduction is heat lost through direct contact. An example is heat lost through contact with water. The thermal conductivity of water is 30 times greater than that of air, which is why cold water immersion is so devastating to the body. Convection is heat transfer by movement. An example is heat lost by wind blowing against the body and disrupting the warmed air surrounding the body. Radiation is heat lost through the skin, for example, the unprotected head. Evaporation is heat lost through warm fluid loss. Examples are heat lost from a burn patient due to plasma excretion through the skin or heat losses from the respiratory tract during ventilation.
The physical mechanisms of heat loss are easily understood in situations of exposure to harsh weather or immersion hypothermia as in Jason's case. These type of situations are encountered more frequently in rural areas as a result of accidents during outdoor activities. A more complex problem is that of urban hypothermia. characterized by chronic generalized cooling of highly susceptible individuals (6).
Individuals with impaired thermoregulatory systems are prone to hypothermia and do not require exposure to severe cold to experience heat loss. The most significant high-risk population is the elderly 0. An epidemiological study of deaths as a result of hypothermia found the highest risk group to be those 85 years of age and over. Comparing demographic data for the entire population over 65 years of age. more nonwhites died of hypothermia regardless of sex, and more men died of hypothermia regardless of color. The same study evaluated Washington D.C. statistics and found that out of all the people who died from hypothermia in 1982, 50% had elevated blood alcohol levels. 50% had inadequate housing, and 30% were malnourished (8).
Rationales for the high risk of the elderly population are consistently reported throughout the literature. These risks include decreased peripheral sensation to cold, functional disability, poverty. and social isolation (6-10). Other populations at risk for hypothermia are those with underlying diseases that impair normal thermoregulation. Examples are patients experiencing shock (hypovolemic. cardiogenic, neurogenic), Gram-negative sepsis, staphylococcal pneumonia, hypoendocrine states (thyroid, adrenal, pituitary), profound anemia, pulmonary edema, acute renal failure, epidural hematoma, seizures, hypoglycemia, hypothalamic and CNS dysfunction [Wernicke's encephalopathy, head trauma, tumor, cerebrovascular accident (CVA)], and dermal disease (burns, exfoliative dermititis).
Patients who arrive to the ED for primary illnesses as listed above may, upon further examination, be found to be hypothermic. Conversely, patients brought to the department because of hypothermia may have an underlying condition that prohibits normal response to warming treatment.
Chronic hypothermia occurs gradually with subtle heat losses over time. In most cases the individual does not realize the loss is occurring and therefore does not take action. Patients in social isolation are at greatest risk because no one is aware that cooling is taking place. The individual eventually becomes less active, and neurological function is impaired. Patients in this circumstance are often rescued by concerned neighbors, family, or friends that have not heard nor seen the individual for extended periods of time.
Intoxication with alcohol is the most common cause of urban hypothermia. However, with increasing drug use, hypothermia can also be anticipated in patients with overdoses from cocaine and heroin. Alcohol as a vasodilator increases heat loss to the environment as well as depresses normal CNS temperature control function. In addition to alcohol and illicit drugs there are also several groups of medications that directly interfere with normal thermoregulatory mechanisms predisposing some consumers to hypothermia (8). These medications include nicotine, neuroleptics (tubocurarine, pancuronium). phenothiazines, tricyclic antidepressants, benzodiazepines. narcotics, reserpine, barbiturates, and ß-blockers.
Another population of patients often overlooked that is predisposed to altered sensorium or inability to respond to the cold are patients with psychiatric disorders such as acute psychosis and profound depression (10). The pediatric patient population especially neonates are also at risk for hypothermia regardless of weather conditions. Air-conditioned treatment rooms can pose a major threat to a newborn if the infant is not properly dried, wrapped and placed in a warm environment. Premature infants with little or no subcutaneous fat, underdeveloped neurological systems with inability to shiver, and large body surface area lose heat quickly. In fact, infant core body temperatures drop immediately upon delivery and require immediate measures to replace heat loss. Hypothermia in neonates results in a cascade of events which can lead to hypoglycemia. seizures, and death.
Nursing diagnoses related to the management of Jason's hypothermia and cardiopulmonary arrest are essential. If Jason survives, he and his family will require instruction on identification and management of future potential medical problems related to complications of hypothermia and treatment as well as safety measures that will prevent this sort of accident from happening again.
Diagnosis: Hypothermia related to accidental cold water immersion for 30 min
Desired patient outcome: The patient's core body temperature will increase to normothermia in response to active core rewarming interventions.
Diagnosis: Ineffective breathing pattern related to absence of CNS function
Desired patient outcome: Artificial ventilation will provide the patient with symmetrical chest expansion; the patient will have breath sounds, heard in all lung fields.
Diagnosis: Impaired gas exchange related to decreased oxygen delivery from cardiopulmonary arrest and pulmonary edema secondary to fresh water drowning
Desired patient outcome: The patient will maintain a PaO2 > 90 to 100 mm Hg and maintain capillary oxygen saturation above 97%; the patient will have clear breath sounds, pink mucous membranes, and brisk capillary refill.
Diagnosis: Decreased cardiac output related to cardiac arrest secondary to hypothermia
Desired patient outcome: The patient will have normal cardiac function following rapid core rewarming of the heart evidenced by ECG showing sinus rhythm, systolic BP > 90 mm Hg. HR < 100 beats/min; urinary output > 30 ml/hr.
Diagnosis: Fluid volume deficit related to vasodilation and diuresis of intravascular volume
Desired patient outcome: The patient will maintain a systolic BP > 90 mm Hg, HR < 100 beats/min, and urinary output > 30 ml/hr.
Diagnosis: Altered cardiopulmonary tissue perfusion related to hypothermia
Desired patient outcome: The patient will respond to core re-warming by converting asystole to a perfusing rhythm and upon reaching normothermia will maintain a sinus rhythm. The patient's ECG will show no PVCs nor evidence of myocardial ischemia (absence of J waves, ST elevation. ST depression, or inverted T waves).
Diagnosis: Altered cerebral tissue perfusion related to hypothermia
Desired patient outcome: The patient will respond to core re-warming by return of neurological function as evidenced by pupils constricting briskly to light, return of reflexes, response to stimuli, and response to verbal commands.
Diagnosis: Knowledge deficit related to accidental cold water immersion via fall through ice
Desired patient outcome: The patient will be able to describe risks associated with walking on ice. The patient will describe proper actions to take if confronted with the same situation in the future. The patient will identify emergency measures that should be taken if he is witness to a similar incident.
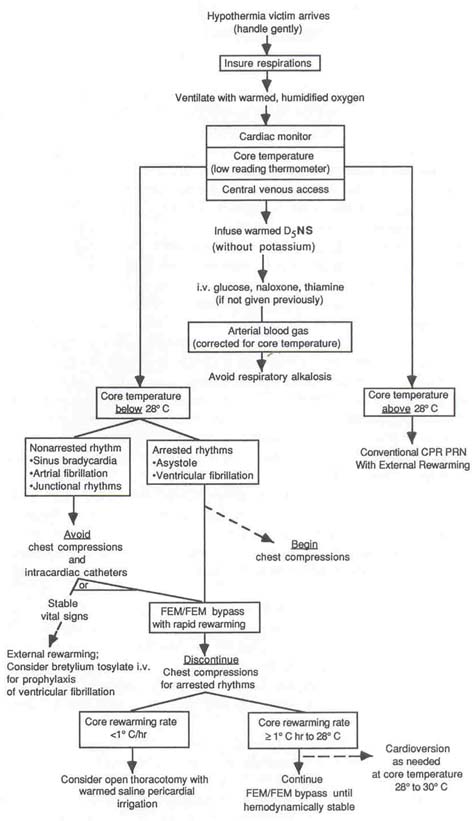
Figures 5.4.1 and 5.4.2 describe the standard algorithm for management of hypothermia. As the algorithm describes, field treatment and initial ED treatment for cases like Jason focus on airway, breathing, and circulation. The nurse caring for Jason must ensure airway patency by assessing the placement of the endotracheal tube. chest expansion, and breath sounds. A heating unit placed around an oxygen humidifier prior to patient arrival will provide for heated 100% oxygen delivery to the patient. Optimal gas exchange can be ensured by the nurse's vigilant suctioning of excess secretions and continuous monitoring and reporting of the patient's oxygenation status.
Nursing interventions related to cardiovascular function follow the primary goal of returning the patient's core body temperature to normal. Extracorporeal blood rewarming if available is considered the best treatment for patients like Jason in cardiopulmonary arrest with temperatures below 28 °C(1, 10-13). This is accomplished by gaining vascular access to the femoral artery and vein and circulating the patient's blood through the bypass machine until core temperature reaches 30 to 32°C. Disadvantages to this technique include the need for special equipment, the need for an OR team and a perfusionist, the heparinized state of the patient, potential damage to red blood cells, and potential damage to blood vessels.
Other methods of active core body rewarming include intragastric balloon inflation, colonic irrigation, mediastinal irrigation, hemodialysis, and peritoneal dialysis. Intragastric balloon inflation is accomplished by passing a cuffed tube down the esophagus until it reaches the stomach. Once placement in the stomach is verified, heated NS is instilled and the cuff is inflated to keep the solution in place. Colonic irrigation is accomplished by inserting a large Foley catheter into the rectum and irrigating the large bowel by means of warmed saline enemas.
Mediastinal irrigation is performed after thoracotomy with warmed saline irrigation fluid poured into the chest cavity. Hemodialysis and peritoneal dialysis are performed as usual with attention to maintaining the temperature of the dialysate at 40°C (1. 10. 13). Heated humidified oxygen administration is promoted in most of the literature reviewed: however, there is conflicting evidence as to its effectiveness as a true core rewarmer (11. 12. 14. 15). All these procedures require the emergency nurse to be knowledgeable about the equipment needed, to understand the steps of each technique in order to anticipate and assist the physician as necessary, and to be able to coordinate simultaneous activities while guarding patient safety.
In situations where invasive measures are being used for rewarming. basic measures to increase body temperature should not be overlooked. The nurse, by ensuring that the patient is dry and on a warm surface, will prevent further heat loss. Ensuring that all fluids in contact with the patient have been warmed is essential, including blood products and crystalloids. The nurse must closely monitor and document amounts of fluid used for resuscitation as well as urinary output to ensure that adequate volume is delivered.
As discussed earlier, cardiac arrest drugs are not indicated for temperatures below 28 to 30°C. Several authors (1. 5. 10). however, suggest administering 25 g D5()W. 100 mg thiamine. and 2 mg Narcan as soon as intravenous access is available. Baseline neurological function as well as response to these medications are important parameters for the nurse to be monitoring. Anticipating for these drugs and having them prepared prior to patient arrival eliminates delay in administration.
Bretylium is one antiarrythmic drug that has been helpful in some hypothermic patients. In one case study (16). 10 mg of Bretylium per kg of body weight converted ventricular fibrillation at a core temperature of29.5°C after 6 min. When the epinephrine was ineffective, the emergency nurse caring for Jason could have suggested to the physician team leader that a dose of 400 to 800 mg bretylium intravenous push might be effective.
When there is a perfusing cardiac rhythm in the presence of hypothermia. the management of the patient can be much less aggressive. The goal of therapy would be to maintain normal cardiac function while gently rewarming the patient, taking care not to stimulate ventricular fibrillation. At temperatures above 30°C rapid rewarming is rarely necessary. Passive methods such as heated humidified oxygen, warm intravenous fluids, and use of an external heat source are usually sufficient (10).
If Jason's case had been less serious and he had been easily warmed in the ED, the nurse would then have to talk with him and his parents to prevent this kind of accident from happening again. Topics for discussion should include making correct choices, how to handle peer pressure, proper actions to take when around ice. methods to protect one's self against heat loss, and how to contact emergency medical services when needed.
Figure 5.4.1. Prehospital algorithm. (From Zell SC, Kurtz KJ: Severe exposure hypothermia: a resuscitation protocol. Ann Emerg Med 14(4): 340, 1985.)
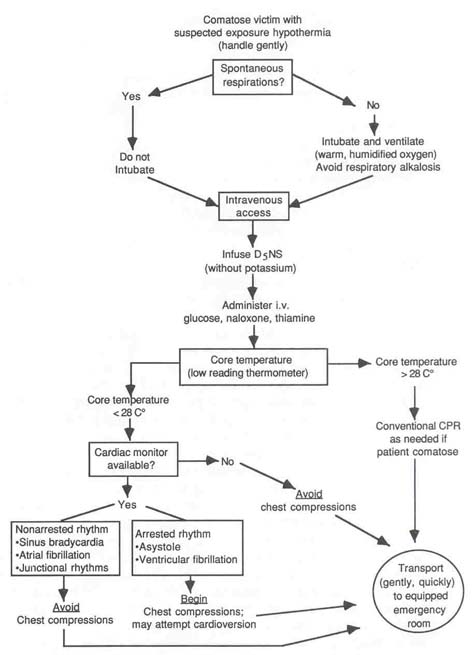
Figure 5.4.2. Emergency department algorithm. (From Zell SC, Kurtz KJ: Severe exposure hypothermia protocol. Ann Emerg Med 14(4): 342,1985.)
There are three major groups of complications resulting from active rewarming of a patient: (1) after drop, (2) rewarming shock and associated complications from external rewarming, and (3) direct pathology to organ systems from the hypothermic event. There are also complications associated with the various treatment measures as already discussed in question 5.
After drop is defined as a continued fall in body temperature after rewarming maneuvers have been initiated (17). Usually body temperatures will continue to fall during the first 10 to 30 min of resuscitation. This phenomenon occurs primarily with rapid immersion cooling, and rarely with gradual cooling as experienced by the elderly (17). After drop can be minimized by core rewarming, but must be closely monitored during initial resuscitation.
External rewarming of the skin and extremities can have serious negative effects. As the peripheral tissues are warmed, vascular beds dilate, releasing cold acidotic blood to the heart. Rewarming acidosis occurs from circulation of peripheral blood that had become stagnate without flow. resulting in anaerobic metabolism and lactic acid production. Acidosis also occurs as a result of increased metabolic demands of the newly heated peripheral tissues not being met by the cold core body organs (10). This influx of acidotic blood could stimulate the heart into ventricular fibrillation. Dilation of the blood vessels also reduces systemic vascular resistance decreasing blood pressure and further depressing cardiac function (4). Ventricular fibrillation is a common complication during rewarming efforts with patients in initial reperfusion rhythms. This is due to the heart's decreased fibrillatory threshold that is easily triggered by resuscitation procedures. Ventricular fibrillation has been stimulated in patients with temperatures less than 28°C by movement of their body during transit, endotracheal intubations, central line insertion, and introduction of gastric tubes (4, 10,11).
Even when quick central core rewarming techniques are used. hypothermia continues to have associated complications. Hypoglycemia occurs as a result of depletion of body stores of glucose and is complicated by impaired insulin function (4). Hypovolemia occurs as a result of the shift of body fluids to the extra cellular compartment and induced diuresis (3).
Intravascular thrombus formation with MI and CVA is a result of the increase viscosity of the blood that results from massive diuresis. Pneumonia and pulmonary edema are pulmonary insults associated with hypothermia. Other effects of hypothermia include pancreatitis. acute tubular necrosis, alkalosis as a result of K+ excretion, hemolysis. depressed bone marrow activity, disseminated intravascular coagulation. hypophosphatemia, seizures, hematuria, myoglobinuria. temporary adrenal insufficiency, and gastric erosion and hemorrhage (1).
In this case, Jason suffered the worst type of hypothermic insult. In addition, he sustained complications from near drowning in fresh water. According to the National Institutes of Health (7), the chances for a complete recovery are good when core body temperatures do not drop below 32.2 °C and there are no other complications. If body temperatures fall between 26.6 and 32.2°C, most victims will recover but may sustain permanent damage. Victims of severe hypothermia with core body temperatures less than 26.6°C have poor chances of survival. Improved systems of patient evacuation and transportation to facilities with advanced technology, coupled with improvements in medical and nursing management of the hypothermic patient, will increase the probability for survival of patients like Jason in the future.
Cathy Robey-Williams, RN, MS, CCRN
Valerie is a 20-year-old white female who was stung on her right hand by a bee. probably a yellow jacket, 30 min ago. She noticed immediate swelling other hand and arm similar to a reaction which she had with a previous sling. This time. however, she felt different, and she describes the sensation as "edgy all over. " When Valerie began feeling a "lump" in her throat and started having difficulty breathing. she called 9II.
The paramedic unit found Valerie sitting upright, leaning forward, in obvious respiratory distress. She was edematous, and her color was acrocyanotic, When answering questions. Valerie could only respond in single-word answers. The paramedic applied oxygen at 10 liters/win via a non-rebreather mask. There was. very little air movement when her breath sounds were auscultated. Vital signs were BP 80/40. HR 120. and respirations 40. The ECG monitor revealed sinus tachycardia without ectopy. An intravenous line was attempted but was unsuccessful. The ED was consulted, and the paramedic requested the following: epinephrinc 0.3 mg: 1:1000 subcutaneous; military antishock trousers (MAST). The physician agreed with the paramedic's request for treatment. The estimated time of arrival was 15 min. Following treatment by the paramedic, Valerie's respiratory status improved Her BP was 100/50 with the legs of the MAST inflated. During transport a second intravenous access attempt was successful, and Ringer's lactate solution was infused wide open.
On arrival to the ED, Valerie is talking in sentences and states her breathing; is much better. She can still feel "that lump" in her throat. Her color is flushed and her skin warm. Valeria's right hand and arm, face. and periorbital area are very edematous. Wheezes are heard in all her lung fields.
Triage Assessment. Acuity Level IV: Severe respiratory distress, respiratory rate 40. acute wheezing, BP < 90 mm Hg.
Valerie is taken immediately to the treatment area where she is kept on oxygen via a non-rebreather mask, and a second liter of Ringer's lactate is hung. Repeat vital signs are BP 100/50, HR 134. and respirations 32. During the interview, Valerie tells the emergency nurse that she has no medical history, is not aware of any allergies, and is only taking oral contraceptives. She states she weighs approximately 130 pounds.
Valerie is given a nebulizer treatment with 0.6 mg Alupent in 3 ml NS. The physician orders include 295 mg intravenous aminophylline over 30 min followed by an infusion of 30 mg/hr: 200 mg intravenous Solu-Cortef: and 25 mg intravenous Benadryl. ABG and admission blood work and chest x-ray are also ordered. Following fluid replacement Valerie' s BP stabilizes at 110/60, and MAST trousers arc reduced. One hour after arrival Valerie appears to be resting comfortably with improvement in her vital signs and breath sounds. Plans have been made for Valerie to be admitted to the hospital for observation overnight.
Anaphylaxis is a Greek term meaning backward protection. The word originates from the early 1900s when Portier and Richet described the responses of dogs to sea anemone toxin. Instead of protecting dogs from the toxin as proposed, repeated exposures to toxin resulted in a hypersensitivity reaction producing massive circulatory collapse and death (1).
Prior exposure to an antigen is required for anaphylaxis to occur. The antigen is necessary to stimulate IgE antibody formation. The term anaphylaxis can be used broadly to describe any IgE-mediated reaction releasing histamine and affecting target organs which are blood vessels and smooth muscle (2). Most clinicians reserve the term anaphylaxis for severe systemic responses where there is circulatory collapse (2).
Bee or Hymenoptera stings and penicillin are the two major causes of anaphylaxis in humans (3). The Hymenoptera family consists of honey bees, yellow jackets, wasps, hornets, and fire ants. Hymenoptera venom, a protein, is the antigen that stimulates the chain of events leading to anaphylaxis which accounts for a reported average of 40 deaths per year in the United States (4).
There are three separate events that produce anaphylaxis following exposure to a foreign substance: (1) antigen-antibody reaction or complement activation, (2) release of pharmacologically active mediators, and (3) the response of the individual. The initial exposure to an antigen, i.e.. the first bee sting, sensitizes a group of B lymphocytes. Plasma cells are then produced which secrete IgE antibodies. The IgE molecule then attaches to the surface of mast cells and basophils (5).
Subsequent exposures to the antigen produce the chain reaction seen in anaphylaxis. As the antigen enters the body. it attaches to the IgE molecules that are affixed to the mast cell surface. This added bond activates degranulation of the mast cells and basophils resulting in exocytosis of cell contents. Mast cell exocytosis releases a complex of histamine and heparin which dissociates and circulates into the blood stream. Heparin produces prolonged clotting time. Histamine produces arteriole, venule, and capillary dilatation (3, 5).
There are two types of histamine receptors throughout the body. Stimulation of HI receptors by circulating histamine results in non-vascular smooth muscle contraction. H2 receptors, when activated. increase gastric secretion which may produce vomiting as well as stimulate cardiac function, which on rare occasions results in isch-emic changes on ECG (6). Table 5.5.1 summarizes types of smooth muscle and symptoms that may result when the muscles are affected by histamine.
Several other chemical mediators are released from mast cells and basophils during anaphylaxis: serotonin, kinins, prostaglandins. and leukotrienes. The actions of these mediators combined, contributes to the major respiratory and cardiovascular changes seen with anaphylaxis.
The response of the individual or clinical presentation of anaphylaxis is extremely variable. Symptoms may be mild to irreversible, resulting in death. Reactions to antigens usually occur within 30 min. Factors contributing to an individual's variable response are dose of antigen, route of administration (injection of bee venom from stinger), and the degree of host responsiveness (3).
The body's normal response to a bee sting is first intense burning throbbing pain at the site of venom injection. A small area of inflammation and erythema then develops. This minimal amount of swelling should only pose a threat if the sting occurred in the pharynx affecting breathing or affects distal circulation such as in a ring-bearing finger (7).
Many individuals experience a hypersensitivity reaction to bee stings and other bites such as spiders, mosquitoes, and horseflies. Hypersensitivity reactions are limited to inflammation and erythema, but can affect a larger local area such as the entire arm if the hand is stung. As long as no systemic symptoms occur, the individual is not experiencing a life-threatening emergency. Systemic symptoms of anaphylaxis include itching, paresthesia distal to sting site. generalized erythema, urticaria, angioedema, dyspnea. wheezing, stridor, vocal changes, feeling of impending doom, abdominal pain. vomiting, diarrhea, urinary incontinence, vaginal bleeding, and tachycardia (7. 8).
Individuals experiencing hypersensitivity reactions should be warned that they may develop systemic reactions with future stings. These people should be taught the signs and symptoms and how to obtain proper medical attention.
Table 5.5.1 Histamine Action on Smooth Muscle with Clinical Symptomatology
| Smooth Muscle | Histamine Action | Clinicla Sympton |
| Bronchi | Bronchospasm | Wheezing, Stridor, dyspnea |
| Capillaries | Increased membrance permeability | Decreased vascular volume, pulmonary edema |
| Angioedema | Uvula and laryngeal edema, choking Sensation, dysphonia, barking, crowing complete airway obstruction | |
| Intestine | Constriction and stimulation of motility | Cramping abdominal pain, vomiting diarrhea |
| Bladder | Contraction | Urinary incontinence |
| Uterus | Contraction | Vaginal bleeding, premature labor |
| Adapted from Dickerson M: Anaphylaxis. Crit Care Nurs Q 11(1):72,1988, reprinted with permission of Aspen Publishers, Inc., © June 1988. | ||
A summary of the drugs used, including dosage, and their action is listed in Table 5.5.2.
TIP: The presence of ß-blockade medications may decrease the effectiveness of epinephrine. If a patient does not respond to an initial dose of epinephrine. 1 mg intravenous glucagon followed by an infusion of 1 mg/hr is recommended (1. 9).
Table 5.5.2 Common Medication Used in the Treatment of Anaphylaxis
| Medication | Dosage | Action |
| Epinephrine | 0.3-0.5 mg of 1:1000 solution s.c. or i.m.; or 1:10,000 solution i.v. Titrate to effect Used when there is evidence Of circulatory collapse | Increases contractility and Cardiac bronchodilation, constricts aterioles and increases peripheral vascular resistance |
| Metaproterenol Sulfate (Alupent) | 0.6 mg aerosol in 3ml NS | Bronchodilation |
| Aminophyline | Loading dose: (5 mg / kg body Weight) i.v. over 30 min; infusion: 0.5 mg /kg / hr | Bronchodilation |
| Hydrocortisone (Solu-Cortef) Diphenhydramine Hydrochloride (Benadryl) | 200-400 mg every 4-6 hr 25-50mg i.v. or i.m | Stabilizes capillary membrane Blocks histamine receptors; relieves itching, urticaria decreases angioedema |
Nursing diagnoses related to management of Valerie's airway. breathing, and circulatory collapse are crucial. She also requires instruction on management of future potential problems.
Diagnosis: Ineffective breathing pattern related to a decrease in effective airway size from bronchoconstriction resulting in hypoventilation
Desired patient outcome: The patient will experience Bronchodilation with decreased wheezing, and breath sounds heard clearly in all lung fields. The patient describes relief in the ability to breathe.
Diagnosis: Impaired gas exchange related to decreased oxygen delivery from alveolar hypoventilation and accumulation of pulmonary interstitial fluid
Desired patient outcome: The patient will maintain PaO2 of 90 to 100 mm Hg, and maintain capillary 02 saturation above 97%; the patient will have clear breath sounds, respiratory rate of 12 to 24. and pink mucous membranes
Diagnosis: Decreased cardiac output related to peripheral vasodilation
Desired patient outcome: The patient will maintain systolic BP > 90 mm Hg, HR < 100 beats/min, maintain a Glasgow Coma Score of 15, and urinary output > 30 ml/hr.
Diagnosis: Decreased cardiac output related to fluid shift from vascular compartment into interstitial space because of increased vascular permeability
Desired patient outcome: The patient will experience a decrease in circumferential size of extremities. The patient will have diminished angioedema as evidenced by return of voice, ability to speak clearly, ability to swallow, and decrease in dyspnea.
Diagnosis: Pain related to body changes and fluid shifts from the chemical action of kinins on body tissue
Desired patient outcome: The patient will state that there is relief of pain and itching: the patient will not exhibit behavior cues of discomfort.
Diagnosis: Anxiety related to sympathetic stimulation from the stress response and catecholamine administration
Desired patient outcome: The patient will verbalize understanding of feelings and sensations resulting from anaphylaxis and medications. Patient will maintain control over anxiety evidenced by calm tone of voice, lack of repetitive motor movement. appropriate discussion, and questions.
Diagnosis: Knowledge deficit related to anaphylaxis and risk of future antigen exposure; treatment techniques
Desired patient outcome: The patient will describe the sequence of events that will result from another bee sting. The patient will describe activities to avoid to decrease her risk. i.e.. walking barefoot outside, picnics in August. The patient will return demonstrate technique of subcutaneous injection describing correct dose of epinephrine to be administered using Ana-Kit prescribed to her at discharge. The patient will describe the appropriate steps she would take if she is again stung by a bee.
Valerie's triage assessment of level IV communicates to the staff that immediate intervention is required. Nursing interventions for Valerie focus on maintaining an adequate airway and treatment of shock. Because a preliminary report was received from the field. equipment for intubation, fluids for resuscitation. and medications were prepared ahead of Valerie's arrival.
The nurse should begin the assessment with airway patency and ventilation effectiveness. Oxygenation should be assessed via neurological status, ABGs, and oxygen saturation. A pulse oximeter is useful to monitor 0; saturation. Assessment of circulatory status should follow. including cardiac monitoring and obtaining vital signs. Peripheral circulation assessment should include color, temperature, pulse checks. and capillary refill. Urinary output, the most sensitive indicator of cardiac output, should be monitored as soon as Foley catheterization can be accomplished. In Valerie's case, she responded immediately to treatment, and therefore catheterization was not indicated.
As always. Valerie's nurse should introduce his- or herself and explain the planned procedures. The nurse should prepare the patient for the sensations the patient may feel with each medication and procedure. The nurse encouraged Valerie to verbalize her fears or questions. and repeatedly asked her if she was in pain. Medications are administered as ordered to assist with airway clearance. The nurse should be alert to and request medical orders for additional medications such as Benadryl and acetaminophen that will reduce inflammation and itching and provide better comfort for the patient.
After Valerie was comfortable, the emergency nurse taught her about the process of anaphylaxis. The nurse discussed the actions that should be taken following future bee stings, and that a medic alert bracelet was essential to wear. Valerie could easily describe ways to avoid contact with bees in the future and recited the key rules she should follow for safety.
TIP: The decision to admit Valerie for overnight observation was based on the risk of reoccurrence of symptoms that reportedly affects 20% of patients. Secondary reactions can occur up to 8 hrs following anaphylaxis (10).