| Contents | Previous | Next |

Guideline: Patients with depressive symptoms or in a major depressive episode may also be suffering from another nonmood psychiatric disorder. Treating one of the two disorders often clarifies the diagnostic picture. If the nonmood disorder is causing the mood symptoms, the nonmood disorder should usually be treated first. When formal major depressive syndrome is associated with another psychiatric condition, the decision of which to treat first rests on the nature of the nonmood disorder:
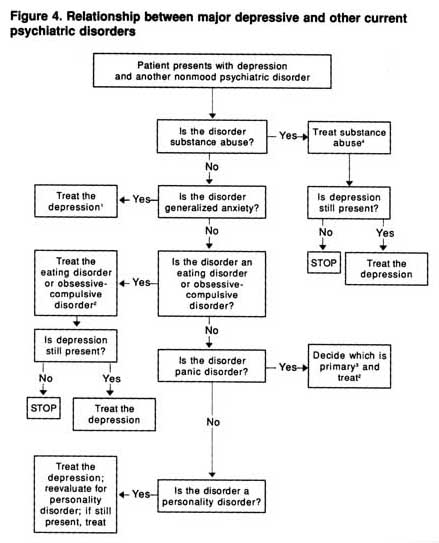
Figure 4 provides an algorithm for deciding when to treat depression in the presence of a concurrent nonmood psychiatric condition.
Guideline: Alcoholism and major depressive disorder are distinct clinical entities. They are not different expressions of the same underlying condition. While alcoholism is rarely a consequence of depression, many alcoholics do develop depressive symptoms or the full syndrome of major depression. (Strength of Evidence = B.)
The following conclusions are tentatively applicable to primary care settings since no data were found on depression in alcoholic patients seen in primary care settings or in alcoholics self-referred to self-help groups such as Alcoholics Anonymous. Most studies are of patients seen in psychiatric settings, who may be more likely to have other psychiatric problems in addition to alcoholism. Furthermore, the diagnostic criteria for alcoholism have become more inclusive over the last 15 years. Figure 4. Relationship between major depressive and other current psychiatric disorders
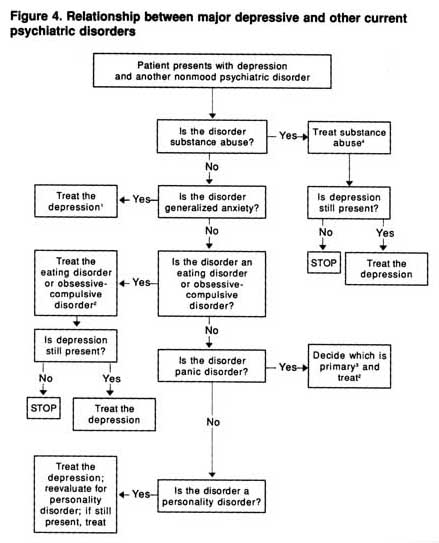
1When the depression is treated, the anxiety disorder should rsolve as well.
2Choose medications known to be effective for both the depression and other psychiatric disorder.
3Primary is the most severe, the longest standing by history, or the one that runs in the patient's family.
4In certain cases (based on history), both major depression and substance abuse may require simultaneous treatment.
Nine studies have examined the extent to which patients with primary depression develop alcoholism (Deykin, Levy, and Wells, 1987; Hasin, Grant, and Endicott, 1988; Lewis, Helzer, Cloninger, et al., 1982; Powell, Read, Penick, et al., 1987; Robins, Gentry, Mutton, et al., 1977; Schuckit, 1983, 1985; Winokur, Reich, Rimmer, et al., 1970; Woodruff, Guze, Clayton, et al., 1973). Most revealed that alcoholism is rarely a consequence of depression; it occurs in less than 5 percent of patients. Overall, the prevalence of alcoholism in patients with primary depression is probably no higher than in the general population.
On the other hand, most studies have found that alcoholics do become depressed over time. Of the 24 studies reviewed, most found that between 10 and 30 percent of patients with alcoholism also suffered from depression at the time of evaluation (see Petty, 1992, and Depression Guideline Panel, forthcoming).
The ECA Study found the prevalence of alcoholism to be approximately 5 percent (Helzer and Pryzbeck, 1988). This study also found the odds ratio for the coexistence of depression and alcoholism to be 1.7. That is, persons in the community who met the diagnostic criteria for alcoholism were nearly twice as likely as those without alcoholism to meet the criteria for major depressive disorder.
Based on the ECA data reanalysis commissioned by the panel, 10 percent of those with major depressive disorder and a concurrent psychiatric condition (n = 31) had alcohol abuse as the second condition. For those with dysthymic disorder complicated by another psychiatric condition (n = 46), 30 percent abused alcohol. For those with DNOS and another psychiatric condition (n = 167), 67 percent abused alcohol. Thus, practitioners should always inquire about co-morbid alcohol and drug abuse or withdrawal in those with mood syndromes and symptoms.
The idea that depressed patients self-medicate with alcohol and, therefore, become alcoholic seems untrue for men, but may be true for some women. The few studies (Depression Guideline Panel, forthcoming) that focused specifically on women suggest that women alcoholics (perhaps as many as one in four) may be more likely to have had a preexisting mood disorder. They may also be more likely to develop depression as a consequence of prolonged heavy drinking, perhaps twice as often as their male alcoholic counterparts. Women reared by alcoholic fathers appear to be at greater risk for depression (Goodwin, Schulsinger, Knopf, et al., 1977).
Although family studies have provided strong evidence that alcoholism and major depressive disorder are independently transmitted, a family history of depression and alcoholism may be associated with a poorer prognosis for the alcoholism. However, there is no evidence for familial aggregation between alcoholism and depression. Adoption studies confirm the independent transmission of depression and alcoholism. Goodwin and colleagues (Goodwin, Schulsinger, Hermansen, et al., 1973; Goodwin, Schulsinger, Knopf, et al., 1977) found an increased incidence of alcoholism in both the adopted sons and daughters of alcohol abusers, but no increase in the incidence of depression. They also found that daughters of alcoholics reared by their biologic parents were more likely to experience depression as adults. This suggests that the environment can contribute to the development of depression, particularly in women. Two studies suggest an important additive interaction between alcoholism and depression (van Knorring, Bohman, van Knorring, et al., 1985; Zisook and Schuckit, 1987). It may be that the familial contribution of mood disorder to alcoholism indicates a poorer prognosis for the alcoholism.
The clinical course of depression with alcoholism has not been extensively studied. Available data from four studies suggest that most patients admitted to alcoholism treatment programs who also have clinical depression experience spontaneous remission of their depressive symptoms during the first 2 to 4 weeks of sobriety (Brown and Schuckit, 1988; Dorus, Kennedy, Gibbons, et al., 1987; Schuckit, 1983, in press; Willenbring, 1986). Depressive symptoms and syndromes seen in very recently detoxified alcoholics likely reflect the toxic effects of alcohol consumption.
The longer term course of illness for depression with alcoholism is more difficult to assess. Two studies that followed patients for more than a year determined that the existence of depression and alcoholism at initial assessment predicted a poorer outcome for the alcoholism, at least in men, 1 year later (Loosen, Dew, and Prange, 1990; Rounsaville, Dolinsky, Babor, et al., 1987). One 2-year follownp study found no difference in alcoholic symptoms in patients with major depressive disorder plus alcoholism versus those with alcoholism alone at initial assessment (O’Sullivan, Rynne, Miller, et al., 1988). No lengthier followup studies are available.
For logistical reasons, the panel did not formally review the area of depression with drug abuse or dependency. However, depressive symptoms or major depressive episodes can occur concurrently with drug abuse. Intoxication with brain depressants is known to cause dysphoric mood and even suicidal ideation. Withdrawal from stimulants, such as cocaine or amphetamines, produces sadness, insomnia, apathy, and other depressive symptoms. The course and response to treatment of depressive disorders in patients who abuse drugs may differ from those of depressive disorders in patients who do not have substance dependency. In the ECA data reanalysis, drug abuse was the second condition in 19 percent of the 31 individuals with major depressive disorder and another psychiatric condition, in 30 percent of the 46 with dysthymic disorder and another condition, and in 26 percent of the 167 with DNOS and another psychiatric condition. Substance abuse is common in those with depressive syndromes and symptoms.
Guideline: It is recommended that depressed patients with concurrent substance abuse discontinue the abused substance and their condition be reevaluated 4 to 8 weeks later when they are in a drug-free state. If major depressive disorder is still present, it is treated as a primary mood disorder. In certain clinical situations, however, earlier treatment of the depression may be needed. (Strength of Evidence = B.)
Guideline: Depressive symptoms or syndromes often accompany anxiety, panic, or phobic disorders. Furthermore, anxiety symptoms are frequent in major depressive episodes. The depression may precede the panic or anxiety disorder, or the anxiety disorder may be the forerunner of and part of the longitudinal course of a mood disorder. The presence of both anxiety/panic and a major depressive disorder results in a more severe disorder with greater impairment than does either disorder alone. When the patient complains of anxiety symptoms, major depressive symptoms should be elicited. (Strength of Evidence = A.)
Concurrent panic disorder is present in 10 to 20 percent of patients with major depressive disorder seen in ambulatory treatment settings. In possibly half of these, the panic disorder preceded the major depressive disorder. About 30 percent of outpatients with major depressive disorder may also have met the criteria for generalized anxiety disorder sometime during the course of their illness. In about half of these, the generalized anxiety disorder preceded the major depressive disorder.
Four community studies (Angst and Dobler-Mikola, 1985; Boyd, Burke, Gruenberg, et al., 1984; Hecht, van Zerssen, and Wittchen, 1990; Vollrath, Koch, and Angst, 1990) and one conducted in a primary care setting (Katon, Vitaliano, Russo, et al., 1986) have reported current comorbidity of anxiety and mood disorders using DSM-III or DSM-III-R. Ink the ECA data reanalysis (Johnson and Weissman, unpublished manuscript), panic disorder was found in 19 percent of the 31 people with major depressive disorder and another psychiatric condition, in 7 percent of the 46 people with dysthymic disorder and another condition, and in 21 percent of the 167 people with DNOS and another psychiatric condition.
Most longitudinal studies of patients with anxiety disorders have found an increased incidence of depressive disorders over time. In one study, 91 percent of patients with agoraphobia developed a mood disorder over the 3-year followup (Munjack and Moss, 1981). Eighty-four percent of these patients had a family history of probable mood disorder. One study found that two-thirds of a group with agoraphobia or panic disorder developed major depressive disorder, 85 percent of which was of the melancholic type (Breier, Charney, and Heninger, 1985). Approximately half of those who developed major depressive disorder had experienced at least one prior major depressive episode that was separate from the onset of panic attacks. In a comparative family study of individuals with panic disorder with agoraphobia, limited phobic avoidance, or social phobia, a significantly higher percentage of agoraphobic patients had family histories of mood disorders compared to those with limited and social phobias (Munjack and Moss, 1981).
Available data are consistent with the idea that many persons with concurrent major depressive disorder and panic, social phobic, or generalized anxiety disorders may actually have only a single disorder that presents with both anxiety and depressive symptoms. The decision about which disorder to treat may in some cases be determined by one of the following:
Given that followup studies of those with panic or other anxiety disorders reveal that many will subsequently develop major depressive disorder and that they often have had a prior major depressive disorder or have a family history of major depressive disorder, the depression is the appropriate main target of treatment in many cases. Sometimes, however, only a treatment trial and observation will answer this complex diagnostic question.
Whichever disorder is primary, the data are clear that the combination of panic and major depressive disorders results in a more severe disorder with greater impairment than does either disorder alone. For example, depressed patients with associated panic attacks have a more severe depressive illness and are less likely to recover during a 2-year followup than are those without panic attacks (Coryell, Endicott, Andreasen, et al., 1988). The lifetime suicide attempt rate for persons with both panic and major depressive disorders is more than twice that of those with panic disorder, but without major depressive disorder (19.5 versus 7.0 per 100) (Johnson, Weissman, and Klerman, 1990). In two separate studies, panic disorder and primary major depressive disorder were each associated with high suicide rates (Coryell, Noyes, and Clancy, 1982, 1983). These data strongly suggest the importance of inquiring about, and even expecting to fmd, a concurrent mood disorder (especially major depressive disorder) in patients with anxiety complaints. If an individual presents with both conditions and if they are equally impairing, the practitioner should consider treatment with medications for which efficacy has been demonstrated for both conditions. These include MAOIs, SSRIs, TCAs, or in selected cases alprazolam.
Guideline: The practitioner is advised to ask about anorexia nervosa and bulimia nervosa in young women who present with any mood disorder, especially those with amenorrhea. If present, the eating disorder is the principal target of treatment. (Strength of Evidence = B.)
The eating disorders include anorexia nervosa and bulimia nervosa (American Psychiatric Association, 1987). Anorexia is a refusal to maintain body weight over a minimal normal weight, accompanied by intense fear of becoming fat, disturbance in body image, and amenorrhea. Anorexia occurs in 0.2 to 0.8 percent of adolescent girls in school cohort studies and in 0.05 to 0.1 percent of adults in community samples (Robins, Helzer, Weissman, et al., 1984).
Bulimia is characterized by recurrent episodes of rapid consumption of large amounts of food, accompanied by a feeling of loss of control; regular use of vomiting, laxatives, or other means to attempt to control weight; and overconcern with body shape and weight. The prevalence of bulimia is approximately 1 percent among adolescent and young adult women. Prevalence rates of 1.8 to 1.9 percent have been found in populations at family planning clinics, and rates ranging from 1 to 22 percent have been found in primary care settings.
No large studies of the prevalence of eating disorders among patients with major depressive disorder have been conducted. On the other hand, it is well established that one-third to one-half of patients with eating disorders (either anorexia or bulimia) suffer concurrently from a major depressive syndrome. Approximately 50 to 75 percent of eating disorder patients have a lifetime history of major depressive disorder. Dysthymic disorder and DNOS occur less frequently among patients with eating disorders by most reports.
Assuming a 1 percent prevalence of eating disorders and an 8 percent prevalence of major depressive disorder, and assuming that one-half of eating disorder patients also suffer from concurrent major depressive disorder, the likelihood of an eating disorder may be as high as 1/16 (6 percent) in women between the ages of 15 and 35 who suffer from a major depressive disorder.
Patients with undernutrition from various etiologies often exhibit depressive symptoms, including depressed mood, irritability, poor concentration, indecisiveness, loss of sexual interest, and sleep disturbance, all of which usually improve with weight gain. Thus, when significant depressive symptoms are found with anorexia nervosa, treatment is first aimed at the eating disorder. If mood symptoms persist after the malnourished state has been reversed, treatment is as for a primary mood disorder. A number of studies indicate that some antidepressant medications (e.g., imipramine, desipramine, fluoxetine, MAOIs) and formal cognitive behavioral psychotherapies may help treat the bulimia with or without associated depressive symptoms. (For examples, see Hughes, Wells, Cunningham, et al., 1986; Mitchell and Groat, 1984; Pope, Hudson, Jonas, et al., 1983; Walsh, Stewart, Wright, et al., 1982.) Such treatments, if successful, usually result in remission of the depressive symptoms.
Guideline: For those depressed patients whose disorder has some obsessive features, the mood disorder is the initial focus of treatment. If full-blown OCD is present with depressive symptoms or manicdepressive disorder, the OCD is usually the initial objective of treatment. Evidence from OCD medication treatment trials suggests that, if the OCD is treated successfully, the depressive symptoms usually abate. (Strength of Evidence = A.)
The ECA survey revealed some overlap between OCD, major depressive disorder, and schizophrenic disorder. Most studies agree that the lifetime occurrence of depressive symptoms is high (80 to 100 percent) among OCD patients, even though only about 10 to 30 percent of them meet the criteria for major depressive disorder at the time of admission to study. The major depressive disorder usually follows the onset of OCD, while schizophreniform symptoms are equally likely to precede or to follow OCD onset. A review of 13 followup studies found that OCD patients were at increased risk for major depressive disorder, but not for schizophrenia (Goodwin and Jamison, 1990). Whether currently or ever depressed, OCD patients are likely to have a family history of depression.
The ECA data reanalysis showed that OCD is relatively common among those with a mood disorder complicated by the presence of another psychiatric condition (Johnson and Weissman, unpublished manuscript). Specifically, OCD was found in 35 percent of the 31 subjects with major depressive disorder, in 15 percent of the 46 with dysthymic disorder, and in 40 percent of the 167 with DNOS, when the mood disorder was associated with another psychiatric condition.
The practitioner must differentiate severe depression, which may present with obsessive features, from true OCD. Severely depressed patients have recurrent ruminations, but rarely have compulsions. The content of the* ruminations is usually consistent with a negative sad mood (e.g., guilty preoccupations). These patients often do not meet the formal criteria for OCD and often have had prior episodes of severe depression. The onset of these obsessive symptoms in the severely depressed occurs at the same time as the onset of the major depressive episode.
Guideline: Somatization is defined as the presentation of somatic symptoms by patients with psychiatric illness or psychosocial distress. These somatic symptoms have no, or insufficient, underlying organic cause. While most depressed patients have medically unexplained somatic complaints, they are rarely of sufficient intensity or frequency to meet the threshold for somatization disorder. (Strength of Evidence = A.)
Somatization may well be the main reason for the misdiagnosis of mental illness by primary care physicians (Bridges and Goldberg, 1985). In primary care settings, many depressed and nondepressed patients present with medically unexplained symptoms. Most patients with such complaints do not meet the formal criteria for Somatization disorder, which in DSM-111-R require the presence of 13 or more medically unexplained symptoms. Most patients with diffuse unexplained somatic symptoms in primary care and community samples either have a treatable psychiatric illness (e.g., anxiety or depressive disorders) or are responding to stressful life events. Accurate differential diagnosis and treatment of the acute psychiatric illness often decrease the tendency toward Somatization
Twelve studies of a total of 976 primary care and medical specialty (e.g., gynecology) patients with clinically significant depressive symptoms revealed that 30 to 87 percent also had clinically significant pain complaints (Fishbain, Goldberg, Meagher, et al., 1986; Haley, Turner, and Romano, 1985; Katon, 1988; Katon, Ries, and Kleinman, 1984; Kramlinger, Swanson, and Maruta, 1983; Large, 1986; Lindsay and Wyckoff, 1981; Maruta, Vatterott, and McHardy, 1989; Schaffer, Donlon, and Bittle, 1980; Turner and Romano, 1984; Walker and Greene, 1989; Walker, Katon, Harrop-Griffiths, et al., 1988). A highly significant 30 to 50 percent met the formal criteria for major depressive disorder. Two additional studies found that 50 to 70 percent of primary care patients with psychiatric illness (mainly mood disorders) presented with somatic complaints (Katon, 1987; Katon, Kleinman, and Rosen, 1982).
Conversely, pain symptoms occurred in approximately 60 percent of patients with major depressive disorder in three studies with 403 primary care and medical specialty patients, in which pain was documented by selfreport (Lindsay and Wyckoff, 1981; Magni, Schifano, and de Leo, 1985; van Knorring, Perris, Eisemann, et al., 1983). Major depressive disorder patients had significantly more symptoms on a medical review of symptoms, even when the investigators controlled for chronic medical illness. In a study using a 1,000-patient sample from a health maintenance organization, patients with one pain complaint were no more depressed than were controls (Dworkin, van Korff, and LeResche, 1990). However, patients with two pain complaints were six times more likely, and patients with three pain complaints were eight times more likely, to have a clinical depression. The Medical Outcomes Study also showed that patients with major depressive disorder perceived their general health as poorer; had more limitations in physical, social, and vocational functioning; and had more pain complaints than did persons with chronic medical illnesses (Wells, Stewart, Hays, et al., 1989).
Guideline: The practitioner is advised to have a high index of suspicion for major depressive or other mood disorders if patients present with two or more unexplained pain complaints. A formal diagnostic evaluation for mood disorders is recommended. (Strength of Evidence = B.)
The majority of patients with major depressive disorder, DNOS, or dysthymic disorder have some pain symptoms. The most common complaints in such patients are joint pain, headaches, backaches, and abdominal pain. Treatment of major depressive disorder with somatic complaints usually results in complete relief of the pain complaints.
Guideline: Personality disorders are not uncommon among mooddisordered patients. The presence of a personality disorder does not exclude diagnosis of a mood disorder, if present. When both a major depressive and a personality disorder are present, more frequent and longer major depressive episodes, as well as poorer interepisode recovery (if untreated), may be anticipated. For some with major depression, symptoms that initially appear to be maladaptive personality traits remit once the depressive disorder improves. (Strength of Evidence = B.)
Studies of depressed patients using structured interviews indicate prevalences of personality disorders ranging from 35 percent in psychiatric outpatients to 72 percent in psychiatric inpatients. Most studies report rates of 45 to 65 percent. However, most of these studies were conducted in specialized research centers, which may attract a greater proportion of mood-disordered patients who also have personality disorders.
The DSM-III-R personality disorders are grouped into three clusters:
The presence of these personality disorders may negatively affect the natural course and treatment response of mood disorders. Five studies have examined patients with concurrent major depressive disorder and a personality disorder (Black, Bell, Hulbert, et al., 1988; Charney, Nelson, and Quinlan, 1981; Ionescu and Popescu, 1989; Pfohl, Stangl, and Zimmerman, 1984; Shea, Glass, Pilkonis, et al., 1987). Those with personality diagnoses had an earlier age of onset for their first depressive episode, more severe depressive symptoms, more frequent episodes, longer depressive episodes, poorer short-term recovery with both antidepressant medications and psychotherapy, and more residual symptomatology at later followup. A concurrent personality disorder diagnosis is associated with a more complicated, disturbed social history, especially in patients with Cluster A or B personality disorders. When depression is complicated by personality disorder, most studies find increased rates of suicide attempts and self-harm.
The generally negative effect of personality disorders on the outcome of depression seems largely accounted for by Cluster B. or borderline personality disorder specifically. Depressed patients with co-morbid borderline personality disorder had poorer social outcomes and higher levels of residual symptomatology at both 4- and 7-year follownps (Pope, Jonas, Hudson, et al., 1983). Borderline personality disorder seems highly prevalent among depressed psychiatric patients; a sample drawn from a general psychiatric population yielded an estimate of 6 percent. The estimated community prevalence of borderline personality disorder is 0.2 percent (Weissman and Myers, 1980). One study of people who were not psychiatric patients found a 1.6 percent prevalence of borderline personality disorder, but this population included a large sample of firstdegree relatives of psychiatric inpatients (Zimmerman and Coryell, 1989). There are insufficient studies of the incidence of personality disorders in primary care settings to make prevalence estimates.
Guideline: DSM-111-R indicates that, if depressive symptoms begin within 2 to 3 weeks of a loved one’s death, the diagnosis is uncomplicated bereavement, which is not viewed as a disorder but as a normal, relatively benign state that resolves spontaneously without treatment. While uncomplicated bereavement and major depressive episodes share many symptoms, active suicidal thoughts, psychotic symptoms, and profound guilt are rare in bereavement. However, if a major depressive episode is still present 2 months following the loss, the episode is likely to be prolonged and associated with substantial morbidity. Clinically, the diagnosis of major depressive disorder may be made during the period of “grief” in those who meet the criteria for a major depressive episode 2 months following the loss. (Strength of Evidence = A.)
Grief reactions are equally common in women and men. Over the course of the first year of bereavement, Clayton (1974) found that 35 percent of 109 widows and widowers met the criteria for a major depressive episode at 1 month, 25 percent at 7 months, 17 percent at 13 months, and 46 percent were depressed some time during the first year following the loss of a spouse.
Zisook and Shuchter (1991) studied 350 widows and widowers 2 and 13 months after their spouses’ deaths. Twenty-four percent met the DSM-III-R criteria for a major depressive episode at 2 months. Since the deaths had occurred only recently, the condition of these subjects was diagnosed as uncomplicated bereavement rather than major depressive disorder. Those meeting the criteria for major depressive disorder early in the period of grief were more likely to have personal or family histories of major depressive episodes (not in response to the death of a loved one), culTent treatment with antidepressant medications, suicidal ideation, poor health, and poor current job satisfaction. Most important, they were likely to be in a major depressive episode 1 year following the loss. Given the anticipated prolonged suffering and disability, it is logical to consider treating these patients for the major depressive disorder, though randomized controlled trials of any treatment are lacking in this population.
A distinct, but poorly studied, segment of primary care patients present serious mood symptoms thought to require clinical management, though they do not fulfill the criteria for major depressive or dysthymic disorders. DSM-III-R classifies such “subthreshold” pathology as either DNOS or an adjustment disorder with depressed mood. Little is known of the presenting symptoms, clinical course, or outcome of an adjustment disorder with depressed mood. However, the clinical utility of the diagnosis is that it allows practitioners to identify mildly distressed patients, some of whom may need followup to determine whether the symptoms remit or whether they evolve into a formal mood syndrome. If such patients develop a major depressive or dysthymic disorder, treatment should be as for the primary mood disorder. There are no randomized controlled trials of treatment for adjustment disorder with depressed mood, but it is logical to consider treatment with psychotherapy or medication for those with substantial pain, suffering, incapacity, or chronicity.
| Contents | Previous | Next |