| Contents | Previous | Next |

Guideline: Depressive disorders should not be confused with the depressed or sad mood that normally accompanies specific life experiences—particularly losses or disappointments. Mood disorders involve disturbances in emotional, cognitive, behavioral, and somatic regulation. A clinical depression or a mood disorder is a syndrome (a constellation of signs and symptoms) that is not a normal reaction to life’s difficulties. A sad or depressed mood is only one of many signs and symptoms of a clinical depression. In fact, the mood disturbance may include apathy, anxiety, or irritability in addition to or instead of sadness; also, the patient’s interest or capacity for pleasure or enjoyment may be markedly reduced. Not all clinically depressed patients are sad, and many sad patients are not clinically depressed. (Strength of Evidence = A.)
Primary mood disorders include both depressive (unipolar) and manicdepressive (bipolar) conditions. Most mood disorders seen in primary care settings are thought by some to be at an early, poorly organized stage of the illness. These disorders are often mixed with anxiety symptoms and accompanied by vague somatic complaints. Furthermore, they may be less profoundly severe, but more chronic, than those mood disorders encountered primarily by mental health care providers. Patients initially seeking care from primary care providers may be less inclined toward a psychological explanation or conceptualization of their depression.
Guideline: Major depressive disorder (sometimes called unipolar depression) is characterized by one or more episodes of major depression without episodes of mania or hypomania (low-level mania). By definition, major depressive episodes last at least 2 weeks (and typically much longer). (Strength of Evidence = A.)
A sad mood or a significant loss of interest is required, along with several associated signs and symptoms (Table 1), to diagnose a major depressive episode.
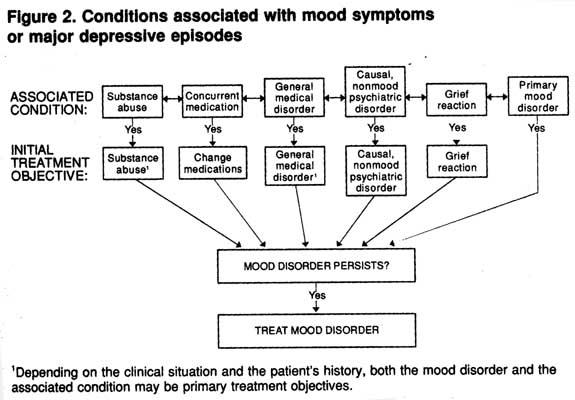
Guideline: A major depressive episode can occur as part of a primary mood disorder (e.g., major depressive or bipolar disorder), as part of other nonmood psychiatric conditions (e.g., eating, panic, or obsessivecompulsive disorders), in cases of drug or alcohol intoxication or withdrawal, as biologic or psychological consequences of various nonpsychiatric general medical conditions or as consequences of the use of selected prescription medications. Finally, a grief reaction (bereavement) may initially (within the first 2 months) meet the criteria for a major depressive episode. (Strength of Evidence = A.)
Table 1. DSM-III-R criteria for major depressive disorder
| At least five of the following symptoms are present during the same period. At least (1 ) depressed mood or (2) loss of interest or pleasure must be present. Symptoms are present most of the day, nearly daily for at least 2 weeks.
|
Whether general medical conditions or medications simply precipitate mood episodes in vulnerable individuals or whether they cause episodes de novo is unclear (Figure 2).
Unipolar forms of primary mood disorders are divided into three groups:
Figure 2. Conditions associated with mood symptoms of major depressive episodes
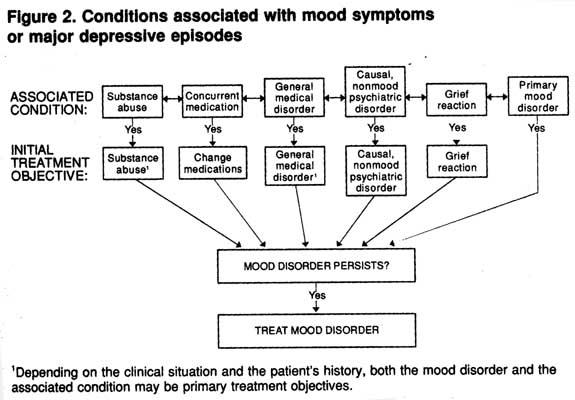
1Depending on the clinical situation and the patient’s history, both the mood disorder and the associated condition may be primary treatment objectives.
Guideline: Bipolar disorders are recurrent, episodic conditions characterized by a history of at least one manic or hypomanic episode. Nineb-five percent of persons with bipolar disorder also have recurrent episodes of major depression. (Strength of Evidence = A.)
Bipolar disorders have been grouped into three types:
Figure 3 summarizes the differential diagnosis of primary mood disorders. The clinically depressed patient must suffer either a sustained sad mood or a significant loss of interest/pleasure, plus associated criterion symptoms. If at least five total symptoms are present for at least 2 weeks, the patient has either a grief reaction or a major depressive episode. The typical bereaved person and nearly all patients with adjustment reactions suffer only two or three associated symptoms. Such patients are rarely suicidal and do not have any significant functional impairment. By definition, these reactions are time-limited (classically lasting less than 6 months) and are not associated with hallucinations or delusions. Some bereaved persons evidence sufficient symptoms to meet the criteria for a major depressive episode within the first month or two following the loss. If these symptoms persist beyond 2 months, the diagnosis should be changed to major depression.
Figure 3. Differential diagnosis of primary mood disorders
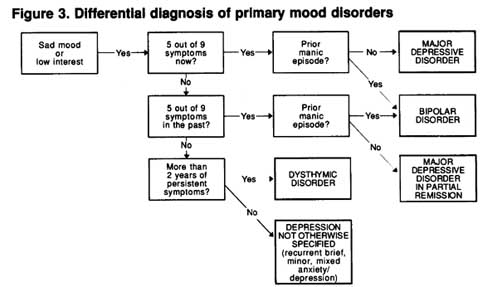
Nearly all patients with major depressive disorder report significant life stresses. The simple presence of a life stress is not a basis for diagnosing either a grief or a situational adjustment reaction, nor is it a basis for excluding the diagnosis of major depressive disorder. Rather, if the patient has only two to three associated symptoms that are mild and present for a short time and if there is no history of major depressive, manic, or hypomanic episodes, an adjustment disorder with depressed mood may be diagnosed. Treatment for this condition and for a classic grief reaction is usually support and reassurance. For some cases of adjustment disorder with depressed mood, a change in lifestyle or relationship patterns may be needed.
If someone has only two or three (but not five or more) symptoms associated with a major depressive episode, it is essential that the practitioner ask about prior major depressive episodes to see if the patient has only partially recovered from a prior major depressive episode. If so, treatment proceeds as for major depressive disorder.
If prior or current major depressive episodes are diagnosed, a history of manic (or hypomanic) episodes should be sought to evaluate the possibility of the presence of a bipolar disorder. If no such episodes have occurred, a history of prior episodes of major depression is sought to determine whether the major depressive disorder is single episode or recurrent. The number of episodes, including the present one, determines whether maintenance treatment should be a consideration.
Even if the patient has only two or three symptoms of major depression and no prior major depressive episodes, it is still important to elicit a history of manic episodes. The patient may have a full bipolar disorder without yet having sustained a full major depressive episode.
Major depressive disorder may begin at any age, although it usually begins in the mid-20s and 30s. Symptoms develop over days to weeks. Some people have only a single episode, with a full return to premorbid functioning. However, more than 50 percent of those who initially suffer a single major depressive episode eventually develop another. In these cases, the diagnosis is revised to recurrent major depressive disorder. Individuals with recurrent major depressive disorder are at greater risk of developing bipolar disorder than are those with single episodes, and they are more likely to have first-degree biologic relatives with major depressive disorder. Some patients who meet the criteria for major depressive disorder, especially of the recurrent type, have a genotype that groups them more clearly with patients with bipolar disorder, as evidenced by a family history of bipolar disorder, early onset of their major depressive disorder, a higher frequency of depressive episodes, and a greater tendency to show psychomotor retardation and hypersomnia during the episode of major depression (Akiskal, 1983). These patients may have a greater tendency to develop hypomania with standard tricyclic antidepressants (TCAs), and their recurrent depressive episodes may be more responsive to lithium alone (Akiskal, 1983).
The course of recurrent major depressive disorder is variable. In some patients, the episodes are separated by many symptom-free years of normal functioning. For others, the episodes become increasingly frequent with greater age. Major depressive episodes nearly always reduce social, occupational, and interpersonal functioning to some degree, but functioning usually returns to the premorbid level between episodes if the episodes remit completely.
Studies of patients with major depressive disorder have found that most untreated episodes last 6 to 24 months. (For a review of these studies, see Goodwin and Jamison, 1990, and Rush, Cain, Raese, et al., 1991.) For two-thirds of cases, symptoms remit completely and functioning returns to the premorbid level. In the remaining cases, the full episode may persist for more than 2 years (about 5 to 10 percent), or recovery between episodes may be partial (about 20 to 25 percent). Approximately onefourth of patients develop major depression superimposed on a low-grade chronic depression (dysthymic disorder), which accounts for the majority of those with poor interepisode recovery.
Major depressive episodes may end completely or only partially. If the latter occurs, clinical experience and some research data suggest that:
According to data from community samples, women are more likely to remain depressed at 1-year follownp than are men (Weissman and Myers, 1978). For women, older age, less than a high school education, and an unstable marital history are risk factors. In addition, women with major depressive disorder whose disease was more severe, more recurrent, or associated with greater prior or current co-morbidity for panic or somatization disorder (but not drug or alcohol abuse) at initial evaluation are more likely to have major depressive disorder 1 year later. Men, but not women, with both dysthymic and major depressive disorders initially are more likely to have major depressive disorder 1 year later. For men, age, education, and marital history are unrelated to outcome. For both sexes, longer lasting episodes of major depressive disorder at initial evaluation are related to the presence of major depressive disorder 1 year later.
The panel commissioned a reanalysis of the data from the large, multisite Epidemiologic Catchment Area (ECA) Study, which involved more than 18,000 interviews in several communities (Eaton, Holzer, von Korff, et al., 1984; Eaton, Regier, Locke, et al., 1981; Regier, Boyd, Burke, et al., 1988; Regier, Myers, Kramer, et al., 1984; Weissman and Klerman, 1978; Weissman, Leaf, Tischler, et al., 1988; Weissman and Myers, 1978) and revealed that at 1-year followup 40.3 percent of those with major depressive disorder still had the same diagnosis, 2.6 percent had developed dysthymic disorder, 16.7 percent had improved somewhat but had not completely recovered, and 40.5 percent had no mood disorder (Johnson and Weissman, unpublished manuscript). Studies also indicate that treatment for major depressive disorder is more effective earlier in the episode, before it becomes chronic (Bielski and Friedel, 1976; Kupfer, Frank, and Perel, 1989; Rush, Hollon, Beck, et al., 1978). Taken together, these findings suggest that early treatment is essential to reduce subsequent morbidity and mortality.
To put these findings into context, it is necessary to recognize that data from epidemiologic community samples include many mood-disordered persons who are neither seeking nor receiving treatment for their psychiatric disorders. Assuming that these people are “less ill” than are those in treatment with mental health care specialists, outcomes based on community samples are likely to provide a more optimistic view than are outcomes in primary care or psychiatric outpatient samples.
Guideline: The point prevalence for major depressive disorder in the Western industrialized nations is 2.3 to 3.2 percent for men and 4.5 to 9.3 percent for women. The lifetime risk for major depressive disorder is 7 to 12 percent for men and 20 to 25 percent for women. Risk factors for major depressive disorder include female gender (especially during the postpartum period), a history of depressive illness in firstdegree relatives, and prior episodes of major depression. (Strength of Evidence = A.)
The above gender difference is found in community samples and, thus, is not due to increased female help-seeking behavior. Prevalence rates for major depressive disorder are unrelated to race, education, income, or civil status. Recent epidemiologic data clearly indicate that the age at onset of major depressive disorder has decreased for the more recently born (the “birth cohort” effect) in many westernized cultures.
A recent review of available studies strongly suggests that psychosocial events or stresses may play a significant role in precipitating the first or second episodes of major depressive disorder, but they may play little or no role in the onset of subsequent episodes (Post, 1992). That is, for the recurrent forms of major depressive disorder, new episodes are less likely to involve a specific precipitant as the disorder becomes more firmly established.
Individuals with major depressive disorder, as well as those with dysthymic disorder and DNOS, are high users of medical services and are as functionally impaired as are patients with severe chronic medical disorders (Katon, von Korff, Lin, et al., 1990; van Korff, Ormel, Katon, et al., 1992; Weissman, Leaf, Tischler, et al., 1988; Weissman and Myers, 1978).
The lifetime psychiatric co-morbidity rate for major depressive disorder can be as high as 43 percent (Sergeant, Bruce, Florio, et al., 1990). That is, up to 43 percent of patients with major depressive disorder have histories of one or more nonmood psychiatric disorders. The 1-month point prevalence for concurrent in contrast to lifetime psychiatric comorbidity is 8 percent.
Depressive conditions are highly prevalent in primary care settings (Johnson and Weissman, unpublished manuscript). Prevalence rates of depression based on chart notations by primary care physicians vary from 1.5 to 4.5 percent. Structured psychiatric interviews based on standard diagnostic systems (DSM-III-R or ICD-9) provide the best prevalence data because they identify all who have the conditions and differentiate them from those with depressive symptoms from other causes. (However, even many of the studies in which the investigators used structured interviews may not fully exclude patients whose depression was caused by concurrent nonpsychiatric medical disorders, medications, or substances of abuse.) Eleven studies have used structured psychiatric interviews and specific diagnostic criteria to determine the prevalence of major depressive disorder. in primary care settings (Table 2). The point prevalence of major depressive disorder in primary care outpatient settings ranged from 4.8 to 8.6 percent; 14.6 percent of adult medical inpatients studied met ICD-9 criteria for major depressive disorder (Feldman, Mayou, Hawton, et al., 1987).
Guideline: Patients with major depressive disorder have substantial amounts of physical and psychological disability, as well as occupational difficulties. (Strength of Evidence = A.)
Untreated major depressive disorder has a substantial effect on health and functioning. Patients in a major depressive episode report substantially poorer intimate relationships and less satisfying social interactions than do members of the general population who have previously suffered from depression or who currently have other psychiatric disorders (Fredman, Weissman, Leaf, et al., 1988).
Physical complaints are also common during a major depressive episode. Twenty-three percent of patients in one study reported some days in which their health kept them in bed all or most of the day in the previous 2 weeks, compared to 5 percent for the general population (Wells, Golding, and Burnam, 1988a). This finding is supported by reports of the health status of community respondents with major depressive disorder, 48 percent of whom described their health as either fair or poor, compared to only 19 percent of the general population (Wells, Golding, and Burnam, 1988a). Other general population data indicate that patients with major depressive disorder reported 11 disability days per 90-day interval versus 2.2 disability days for the general population (Broadhead, Blazer, George, et al., 1990). Data from community respondents indicate that 38 percent of patients with major depressive disorder have some chronic activity restriction, and 30 percent of those with depression reported decreased activity days in the previous 2 weeks (Wells, Golding, and Burnam, 1988a).
Clinical samples of patients with major depressive disorder also provide evidence of severe impairment in interpersonal and occupationalfunctioning, including loss of work time (Wells, Stewart, Hays, et al., 1989). Patients with major depressive disorder have more physical illnesses than do other patients seen in primary care settings (Coulehan, Schulberg, Block, et al., 1990). Health care utilization is increased in persons in the community with major depressive disorder compared to other patients in the general medical setting (Regier, Hirschfeld, Goodwin, et al., 1988).
Table 2. Prevalence of major depressive and other mood disorders in primary care settings
| Study | Number of Subjects | Interview | Major Depression | Other Mood Disorders |
| Barrett, Barrett, Oxman, et al., 1988 | 1,055 screened with SCL depression subscale; 260 interviewed | SADS-RDC | 2.2% (6.4% masked major depression) |
3.6% episodic minor depression; 2.1% chronic depression |
| Blacker and Clare, 1988 | 2,308 screened with GHQ; 1,019 interviewed | SADS & PSE RDC | 4.8% | 5.0% intermittent depression; 3.4% minor depression |
| Burnam, Wells, Rogers, et al., 1989 | RAND Medical Outcome Study; Los Angeles, Chicago | DIS & DSM-III | 4.1-5.4% | Not reported |
| Coulehan, Schulberg, Block, et al., 1990 | University general internal medicine clinic; 618 patients |
DIS & DSM-III | 6.6% | Not reported |
| Hoeper, Nycz, Cleary, et al., 1979 | 1,072 screened with GHQ; 247 completed SADS-L | SADS-L & RDC | 5.6% | 5.0% intermittent depression; 3.4% minor depression |
| Hoppe, Leon, and Realini, 1989 | Family health center, San Antonio; 165 patients | DIS & DSM-III | F = 9.8% MDD or dysthymia; M = 11.1% MDD or dysthymia |
Not reported seperately |
| Kessler, Cleary, and Burke, 1985 | ECA users of health care | DIS & DSM-III | F = 6.9-9.3% M = 3.3-6.5% |
Not reported |
| Ormel, Van Den Brink, Koeter, et al., 1990 | 2,237 screened with GHQ | PSE & PSE-10 Bedford College criteria | 5.6% | 4.7% borderline depression (similar to minor depression) |
| Schulberg, Saul, McClelland, et al., 1985 | 1,554 screened with CES-D; 294 completed DIS | DIS & DSM-III | 6.2% | 3.0% dysthymic and adjustment disorder |
| von Korff, Shapiro, Burke, et al., 1987 | 1,242 screened with GHQ; 730 patients interviewed | DIS & DSM-III | 5% | 3.7% dysthymic disorder |
| Zich, Attkisson, and Greenfield, 1990 | University general internal medicine; 65 patients | DIS & DSM-III | 7.7% | Not reported |
Note: SCL = Symptom Checklist. SADS-RDC = Schedule for Affective Disorders and Schizophrenia-Research Diagnostic Criteria. GHQ = General Health Questionnaire. PSE = Present State Examination. DIS = Diagnostic Interview Schedule. SADS-L = Schedule for Affective Disorders and Schizophrenia-Lifetime Version. MDD = major depressive disorder. ECA = Epidemiologic Catchment Area. CES-D = Center for Epidemiological Studies Depression Scale.
Major depressive disorder is associated with increased mortality, which is generally considered to be secondary to suicide and accidents (Wells, 1985). A recent report indicated that patients with major depressive disorder admitted to nursing homes had a 59 percent greater likelihood of death in the first year following admission compared to those without major depressive disorder (Rovuer, German, Brant, et al., 1991). Patients with major depressive disorder in the ECA Study aged 55 and over had a mortality rate over the next 15 months that was four times higher than that of nondepressed age-matched controls. Up to 15 percent of patients with major depressive disorder severe enough to require hospitalization eventually die by suicide (Coryell, Noyes, and Clancy, 1982).
Studies of major depressive disorder reveal heterogeneity with regard to the biology, family history, pharmacologic response, genetics, and course of illness. Several schemes have been proposed to subdivide major depressive conditions. The common subgroups and possible clinical relevance of each are shown in Table 3. These subtypes are not allinclusive. For example, a large number of patients who have major depressive disorder without melancholic, psychotic, or atypical features have episodes that are not seasonally related and do not have a postpartum onset.
Three subgroups based on cross-sectional symptom features— psychotic, melancholic, and atypical—may have implications for treatment selection. Two based on course features—seasonal pattern and postpartum onset—have prognostic utility; the seasonal type may also suggest the specific therapeutic option of light therapy. However, these subgroups may not be etiologically distinct. Rather, they may represent varying clinical expressions of the same condition over time, in different age groups, or in the context of particular provoking stimuli.
Guideline: Psychotic features refer to the presence of delusions or hallucinations. They occur in 15 percent of patients with major depressive disorders. (Strength of Evidence = A.)
In psychotic depressions, psychotic features are never present without concurrent mood symptoms. Psychotic depressions must be distinguished from schizoaffective disorder. In the latter only, there are periods of atleast 2 weeks during wchich delusions or hallucination are present without mood disturbances.
Table 3. Major depressive disorder subgroups
| Subgroup | Essential Features | Diagnostic Implications | Treatment Implications | Prognostic Implications |
| Psychotic | Hallucinations Delusions | More likely to become bipolar than nonpsychotic types. May be misdiagnosed as schizophrenia. |
Antidepressant medication plus a neuroleptic is more effective than are antidepressants alone. ECT is very effective |
Usually a recurrent illness. Subsequent episodes are usually psychotic. Psychotic subtypes run in families. Mood-incongruent features have a poorer prognosis. |
| Melancholic | Anhedonia Unreactive mood Severe vegitative symptoms |
May be misdiagnosed as dementia. More likey in older patients |
Antidepressant medication is essential. ECT is 90% effective. |
if recurrent, consider maintenance medication. |
| Atypical | Reactive mood Overeacting/ weight gain Oversleeping Rejection sensitivity Heavy limb sensation Fewer episodes |
Common in younger patients. May be misdiagnosed as personality disorder. |
TCAs may be less effective. MAOIs are preffered. ?SSRIs preffered. | Unclear |
| Seasonal | Onset, fall Offset, spring Recurrent |
More frequent in non equatorial latitudes. Pattern occurs in major depressive and bipolar disorders. |
Medications have ? efficacy. Psychotherapy has ? efficacy Phototherapy is an option |
Recurs |
| Postpartum psychosis/ depression | Acute onset (<30 days) in postpartum period. Severe, labile mood symptoms. 1/1,000 is a psychotic form |
Often heralds a bipolar disorder. | Hospitalize. Treat medically. |
50% chance of recurring in next postpartum period. |
Note: ECT = electroconvulsive therapy. TCA = tricyclic antidepressant. MAOIs = monoamine oxidase inhibitors. SSRIs = selective serotonin reuptake inhibitors.
The content of the hallucinations or delusions in psychotic depressions is usually logically consistent with the predominant sad mood (mood congruent). For example, there may be a delusion that the patient has sinned in an unforgivable way. Less commonly, the hallucinations or delusions have no obvious relationship to sadness (mood-incongruent); for example, there may be persecutory delusions, for which the person has no explanation. Studies to date suggest that mood-incongruent symptoms are associated with a worse prognosis; evolve *nto schizophreniform or schizoaffective disorders; involve a less episodic, more chronic course; and require more assiduous, longer maintenance treatment(s). (See LaliveAubert and Rush, 1992; Lalive-Aubert and Rush, in press, for reviews.)
The psychotic features of psychotic major depressive disorder usually recur in subsequent episodes, should such episodes occur. Some studies suggest that psychotic depressive episodes are familial (Schatzberg and Rothschild, in press; Weissman and Johnson, 1990).
For psychotic depressions, TCAs plus a neuroleptic or electroconvulsive therapy (ECT) are each superior to TCAs alone in treating the illness (Depression Guideline Panel, forthcoming). Given the markedly disabling nature of psychotic depression, maintenance treatments are strongly *ndicated when the disorder is recurrent. However, the relative efficacy of maintenance treatment compared to placebo; the value of *ncluding both a neuroleptic and an antidepressant in maintenance treatment; and the acute and maintenance phase efficacy of non-TCA medications, lithium, or selected anticonvulsants have not been studied in randomized controlled trials (Schatzberg and Rothschild, 1992).
Guideline: The key melancholic features of major depressive disorder are:
(Strength of Evidence = A.)
Melancholic symptom features appear to repeat from episode to episode in individuals with recurrent, severe major depressive disorder. They are more commonly present *n older depressed patients (see Rush and Weissenburger, *n press, for a review). Melancholic features are not uniquely associated with a family history of depression. They are associated with reduced rapid eye movement latency and/or dexamethasone nonsuppression (Rush, Cain, Raese, et al., 1991).
Severely symptomatic patients whose depression has melancholic features are likely to respond to treatment with TCAs or to ECT. Melancholic features do not predict which antidepressants will be effective, though the* presence indicates that anxiolytics will not be effective (Depression Guideline Panel, forthcoming). The presence of melancholic symptom features, especially in the severely ill, should sharply increase the practitioner’s tendency to treat with antidepressants and should provoke a thorough questioning for the presence of psychotic symptom features. If medications fail, ECT should be strongly considered for these patients.
The groups studying atypical features deDme the features differently. Two types, vegetative and anxious, have been proposed in the literature. Vegetative features include:
Atypical features of either type are associated with a younger age at onset of illness. Whether these symptoms run in families, repeat across episodes, or are associated with an identifiable or unique biology is not known. However, rapid eye movement latency is not characteristically reduced in this type of mood disorder. The relationship between atypical and melancholic symptom features remains to be clarified. Some data suggest that atypical symptoms may be more likely earlier in the course of major depressive disorder, while melancholic features are more likely to appear later.
Several randomized controlled trials indicate that, when atypical features (those in the vegetative group above) are present, monoamine oxidase inhibitors (MAOIs) are more effective than TCAs, although the laker are still more effective than placebo. Case reports and clinical experience suggest that those depressions with atypical features may respond beKer to selective serotonin reuptake inhibitors (SSRIs) than to TCAs.
Guideline: DSM-III-R indicates that a seasonal pattern for major depressive disorder can be diagnosed only if:
Most often, depressive symptoms remit fully between seasonal episodes. (Strength of Evidence = A.)
The first systematic evidence of the prevalence of seasonal affective disorder was an estimate of 6 percent from a study in the New York area. Subsequently extended to various east coast latitudes, this study showed less than 2 percent prevalence in Florida and nearly 10 percent prevalence in New Hampshire (Rosenthal, Levendosky, Skwerer, et al., 1990; Terman, 1988). There are two to three times as many people personally troubled by the winter recurrence of seasonal mood symptoms than there are those with manifestations severe enough to warrant clinical diagnosis (Kasper, Wehr, Bartko, et al., 1989; Rosen, Targum, Terman, et al., 1990; Terman, Botticelli, Link, et al., 1989).
Preliminary evidence suggests that light therapy is effective in the short-term treatment of outpatients with mild to moderate seasonal major depressive disorder. Further research is required before such a claim can be made for subsyndromal seasonal affective disorder. To date, no hazard has been encountered with short-term light therapy using standard fluorescent lighting apparatus (designed to produce 2,500- to 10,000 lux stimulation and low levels of ultraviolet emission). Exposure extending beyond 2 weeks has not been fully evaluated. Clinical reports suggest that medications may also be effective for some seasonal mood disorders.
Postpartum mood symptoms are divided into three categories, based on severity: blues, psychosis, and depression (Kendell, 1985; for a review, see Purdy and Frank, in press). Postpartum blues are brief episodes (1 to 4 days) of labile mood/tearfulness that normally occur in 50 to 80 percent of women within 1 to 5 days of delivery. Treatment consists of reassurance and time to resolve this normal response.
Postpartum psychoses can be divided into depressed and manic types. Patients with the depressed type show more psychotic, disoriented, agitated, and emotionally labile features, as well as more psychomotor retardation, than do nonpostpartum matched depressed controls (Dean and Kendell, 1981). Most of these cases are associated with signs of organic impairment. Features of the manic type are similar to features of a classic mania. The incidence of postpartum psychosis is low (0.5 to 2.0 per 1,000 deliveries), as shown in eight studies (Grundy and Roberts, 1975; Hemphill, 1952; Kendell, Rennie, Clarke, et al., 1981; Meltzer and Kumar, 1985; Nott, 1982; Paffenbarger, 1964; Paffenbarger and McCabe, 1966;Paffenbarger, 1964; Paffenbarger and McCabe, 1966;Paffenbarger, Steinmetz, Pooler, et al., 1961). Many early cases were mistaken for toxic/infectious states.
The symptoms of postpartum psychosis develop rapidly (over 24 to 72 hours), typically beginning 2 to 3 days after delivery. The period of risk for developing postpartum. psychosis is within the first month following delivery. For acute postpartum psychosis, the prognosis is generally good. However, many patients have previously had or subsequently develop a bipolar disorder. The risk of postpartum psychosis is higher for those with episodes at prior deliveries. The recurrence rate is from 33 to 51 percent.
Nonpsychotic postpartum depressions (major or minor depressive disorders) have also been identified (O’Hare, Neunaber, and Zekoski, 1984). These conditions may occur from 2 weeks to 12 months postpartum, but typically occur within 6 months. The prevalence of nonpsychotic depressions is 10 to 15 percent within the first 3 to 6 months after childbirth, which is somewhat higher than are the rates (5 to 7 percent) in nonchildbearing matched controls. However, the risk for nonpsychotic postpartum depression is higher for persons with a psychiatric history.
No randomized controlled treatment trials for any of the postpartum mood conditions are available. Logic and clinical experience suggest that prophylactic lithium be given as soon as possible after delivery to prevent a postpartum precipitation in patients with a history of bipolar disorder. Likewise, given the high likelihood of recurrence, other previously effective psychotropic medications should be considered in those with a history of psychotic postpartum mood episodes immediately after giving birth.
Guideline: The essential feature of dysthymic disorder is a chronic mood disturbance (sadness in adults; sadness and, possibly, irritability in children and adolescents) present most of the time for at least 2 consecutive years (1 year for children and adolescents). (Strength of Evidence = A.)
Patients with dysthymic disorder exhibit at least two of the associated symptoms noted in Table 4. The associated features of dysthymic disorder are similar to those of major depressive disorder, except that, by definition, delusions or hallucinations are absent. Dysthymic disorder usually begins in childhood or adolescence without a clear onset and with a chroniccourse.
Differentiation between dysthymic disorder and major depressive disorder can be difficult. Their symptoms are similar, differing only in duration and severity. Individuals who initially present with dysthymic disorder frequently go on to develop concurrent major depressive disorder.
Table 4. DSM-III-R criteria for dysthymic disorder
|
Some develop hypomanic episodes, a situation requiring a revised diagnosis of either bipolar disorder not otherwise specified or bipolar II disorder. If the onset of an apparent dysthymic disorder directly follows a major depressive episode, the correct diagnosis is major depressive disorder in partial remission. By definition, dysthymic disorder cannot follow an episode of major depressive disorder unless the major depressive episode has been in full remission for at least 6 months before the onset of the dysthymic condition. When a major depressive episode immediately follows a preexisting dysthymic disorder that has been present for at least 2 years, the diagnosis is concurrent major depressive disorder and dysthymic disorder.
Dysthymic disorders may be primary (i.e., unrelated to other preexisting disorders), or they may accompany coexisting nonmood psychiatric disorders or other nonpsychiatric medical conditions. In the latter case, they are called secondary dysthymic disorders. The presence of dysthymic disorder with no prior episodes of major depressive disorder should cue the practitioner to search for other nonmood psychiatric disorders, such as substance or alcohol abuse. The reanalysis of the ECA Study data showed that, in patients with dysthymic disorder (with and without major depressive disorder) who were reexamined 1 year later, 7 to 26 percent still had dysthymic disorder, 4 to 10 percent had major depressive disorder, 5 to 20 percent had both, 11 to 23 percent had DNOS, and 41 to 52 percent were well (Johnson and Weissman, unpublished manuscript).
ECA Study data indicate a lifetime rate for dysthymic disorder (with and without major depressive disorder) of 4.1 percent for women and 2.2 percent for men. Women aged 25 to 64 had rates of almost 6 percent. Men 65 and over had the lowest rate (1.0 percent). The 1-month prevalence for dysthymic disorder without major depressive disorder was 0.8 percent. The 1-month prevalence for dysthymic disorder with major depressive disorder was 1.3 percent. ECA Study data indicate that 15 percent of those with dysthymic disorder also have a concurrent nonmood psychiatric disorder, usually alcohol or drug abuse. In adults, dysthymic disorder is more common in women than in men. In children, dysthymic disorder, like major depressive disorder, is equally frequent in both sexes. Dysthymic disorder is more common among first-degree biologic relatives of persons with major depressive disorder or with bipolar I and II disorders than among the general population. The point prevalence of dysthymic disorder in primary care outpatients is 2.1 to 3.7 percent.
The functional and financial costs of untreated dysthymic disorder are substantial. In the ECA Study, 29 percent of general medical patients with dysthymic disorder had some chronic restriction of their activity (Wells, Golding, and Burnam, 1988b). Similarly, 27 percent of patients with dysthymic disorder in that community survey showed decreased activities in the previous week. Sixteen percent reported bed days within the previous 2 weeks, compared to only 5 percent of the general population. Furthermore, 39 percent of those with dysthymic disorder said that they had poor or fair health, compared to 19 percent of the general population. Patients with dysthymic disorder reported an average of 3 disability days per 90-day interval, compared to 2 days for the general population.
Guideline: Depression not otherwise specified identifies mood conditions with depressive symptoms that do not meet either severity or duration criteria for dysthymic, major depressive, or bipolar disorders. It is a heterogeneous category. (Strength of Evidence = B.)
Examples of DNOS include minor depression (Merikangas, Ernst, Mater, et al., in press), recurrent brief depressive disorder (Merikangas, Hoyer, and Angst, in press), and mixed anxiety/depression (Zinbarg, Barlow, Liebowitz, et al., in press). Whether these three groupings are true disorders is under investigation. Currently, they are not formally recognized diagnoses. They are described here because less than major forms of depression are common in primary care settings. The treatment implications of these groupings are unclear.
Minor depressive disorder is symptomatically similar to major depressive disorder, but with fewer symptoms and less disability; symptoms come and go, but are present for at least 2 weeks at a time. Minor depressive disorder does not have the chronic/pervasive, multiyear pattern of dysthymic disorder.
Recurrent brief depressive disorder features brief (3 to 7 days) episodes that return 6 to 10 times per year and meet the symptomatic threshold and clinical features of a major depressive episode, but not the 2-week duration criterion (Angst, Merikangas, Scheidegger, et al., 1990). It occurs somewhat more often in women than in men, and the age of onset is late adolescence to the mid-20s. The likelihood of a positive history in firstdegree relatives of patients with recurrent brief depressive disorder is 12 to 20 percent for major depressive disorder and 1 to 3 percent for bipolar disorder.
Studies (Zinbarg, Barlow, Liebowitz, et al., in press) have begun to suggest the existence of a disorder involving symptoms of both anxiety and depression that was particularly prevalent among primary care patients, but they did not use DSM nomenclature. Barrett, Barrett, Oxman, et al. (1988) found that 4.1 percent of a sample of 1,055 primary care patients had mixed anxiety/depression, defined as concurrent anxious and depressive symptoms, neither of which was of sufficient frequency or duration to meet criteria for a formal anxiety or mood disorder.
An analysis of the ECA Study data showed that 11.0 percent of subjects met the criteria for DNOS. The point prevalence of DNOS in primary care outpatients is 8.4 to 9.7 percent (see Depression Guideline Panel, forthcoming).
A reanalysis of the ECA Study 1-year followup data on subjects who had a mood disturbance and two associated symptoms of major depression (an attempt to operationalize DNOS) was commissioned by the panel. The data indicated that for those with DNOS interviewed at 1-year follownp, 38 percent were not ill, 52 percent still had DNOS, 3 percent had developed dysthymic disorder, and 9 percent had developed major depressive disorder (Johnson and Weissman, unpublished manuscript). For some patients, substantial morbidity is thus associated with DNOS over 1 year.
Fifty percent of patients with DNOS in the ECA sample had one or more of the following co-morbid nonmood psychiatric conditions: alcohol or substance abuse/dependence, panic disorder, obsessive-compulsive disorder, or somatization disorder. Phobic and generalized anxiety disorders were not included. The point prevalence for the 167 subjects with co-morbid DNOS was 40 percent for alcohol dependence, 15 percent for drug dependence, 37 percent for panic or obsessive-compulsive disorder, and 1 percent for somatizationdisorder.
Preliminary evidence indicates that DNOS significantly affects patients’ functioning, health, and disability. Patients with DNOS have decreased physical, social, and role functioning (Wells, Stewart, Hays, et al., 1989) and increased disability days. Their current health has been found to be worse than that of those with no chronic condition or those with only chronic medical conditions. Patients with DNOS reported 4 to 6 disability days per 90-day period, compared to the community population rate of 2 days per 90-day period (Broadhead, Blazer, George, et al., 1990).
Guideline: Bipolar disorders classically feature episodes of major depression interspersed with episodes of mania and/or hypomania. (Strength of Evidence = A.)
The major depressive episodes of bipolar disorder meet the criteria outlined in Table 1. Manic episodes are distinct periods of persistently elevated, abnormally expansive, or irritable mood associated with at least three of the symptoms noted in Table 5. About 3 percent of all bipolar disorder patients experience only manic episodes (so-called unipolar mania). Table 5. DSM-111-R criteria for a manic episode
|
Delusions or hallucinations are sometimes present in manic episodes. Their content is usually consistent with the predominant mood (moodcongruent). For example, a patient may hear “God’s voice” explaining that the patient has a special mission or special powers. Delusions may be based on the idea that the person is being persecuted because of some special relationship or attribute. Less commonly, hallucinations or delusions have no apparent content relationship to the expansive/irritable mood (mood-incongruent). Disorders with mood-incongruent psychotic features in the manic episode appear to have a poorer prognosis.
Although they are similar to manic episodes, hypomanic episodes are milder. They are usually brief periods (4 days to several weeks) in which patients are often mildly dysfunctional. Sometimes, they actually feel very well and are creative, but others see them as different from their normal selves. By definition, psychotic symptoms are never present in hypomanic episodes. Patients often do not recall hypomanic periods as times of illness, though others recognize the disturbance. Persons with bipolar I disorder may have hypomanic episodes as well as manic episodes.
In the course of classic bipolar disorder (so-called bipolar I disorder) manic, depressive, and/or mixed manic episodes may occur. (Mixed manic episodes refer to the simultaneous presence of both depressive and manic symptoms in the same episode within the same 24- to 48-hour period.) In bipolar I disorder, manic and depressive episodes are equally frequent. Mixed manic episodes occur in one-third of patients with bipolar I disorder, but these episodes represent only 6 percent of all episodes.
The mean age at onset of bipolar disorder is in the early 20s, and the decade for highest risk of onset is 20 to 29 years of age. The sexes do not differ in age at onset. Men are more likely to have initial manic episodes, while women are more likely to experience initial depressive episodes.
The mean duration of untreated manic episodes is 6 months; the mean duration of untreated major depressive episodes is approximately 8 to 10 months. The depressive episodes immediately precede and/or follow manic episodes in more than half of cases. The total number of episodes of illness experienced by a patient with bipolar disorder during a lifetime is variable. On the average, the episode risk is 0.3 to 0.4 episodes each year.
The time between episodes decreases with subsequent episodes. For individuals, the temporal pattern of episodes tends to repeat itself. Therefore, the future course of illness is best predicted by the individual’s prior course. There is usually a full recovery between episodes, although roughly 25 percent have less than full recovery.
The morbidity and mortality associated with bipolar I disorder are high. Suicides, “accidental deaths,” and intercurrent illnesses contribute to an excessive mortality rate. Ten to 15 percent of untreated patients commit suicide, which is 15 to 20 times the suicide rate in the general population (1 percent over a lifetime of 70 years). Women with bipolar disorder are much more likely than are men to attempt suicide; men are more likely to complete suicide. A large study found that prior to the availability ofeffective treatment, 23 percent of 4,341 patients with a manic episode admitted between 1912 and 1932 died in the hospital, 60 percent from "exhaustion" (Derby, 1933)
Patients with bipolar disorder experience considerable impairment in social and occupational functioning. While manic, they often need to be protected from the consequences of their poor judgement and overactivity, which often result in involuntary hospitalization. Over time, even with periods remission the chronicity and unpredictability of the disorder lead to secondary problems, such as joblessness, legal difficulties, divorce and death by suicide, as well as medical morbidity.
Bipolar I disorder affects men and women equally. It has a lifetime prevalence of 0.4 to 1.2 percent. The 1-month prevalence of bipolar disorder is 0.1 to 0.6 percent. Bipolar I disorder occurs at much higher rates in first-degree biologic relatives of persons with bipolar I disorder than in general population. First-degree relatives of those with bipolar I disorder have a 12 percent chance of having the same disorder over their lifetimes. Another 12 percent have recurrent major depressive disorder, and roughly an additional 12 percent have disthymic or other mood disorders (Goodwin and Jamison, 1990; Rush, Cain, Raese, et al., 1991)
Guideline: Psychoactive substances, such as cocaine and amphetamines; head trauma; certain neurologic diseases; endocrinopathies; and some other disorders can produce secondary manic and hypomanic episodes similar to those seen in primary bipolar disorder. In addition, in some patients with a family history of bipolar disorder, antidepressant medications can precipitate a manic or hypomanic episode. (Stength of Evidence = A)
Case reports suggest that secondary bipolar disorders may be more effectivly treated with anticonvulsants than with lithium. (For a review, see Goodwin and Jamison, 1990)
A seasonal pattern has been found in a subset of patients who have bipolar II disorder (and in some, but fewer, cases of bipolar I disorder). The requisite feature is the occurence of major deprssive episodes in a seasonal pattern (typically, fall onset, spring offset). Perhaps 10 percent of patients with bipolar II disorder expirience such seasonal episodes. It is unclear whether lithium is differentially effective in these patients and, indeed, whether the disorder becomes nonseasonal over time.
Some patients with bipolar I or II disorder exhibit a "rapid cycling" pattern, experiencing four or more mood episodes each year. Mood episodes include manic (or mixed manic-depressive), hypomanic, and major depressive episodes. The mood episodes may follow one anohter with or without intervening asymptomatic periods. According to nearly all studies, from 80 to 90 percent of those with a rapid cycling pattern are women.
Bipolar disorder begins with a rapid cycling pattern in some patients, while rapid cycling develops during the course of the illness for others. Rapid cycling may occur spontaneously or, in some cases, may be caused or maintained by tricyclic and possibly other antidepressant medications. Concurrent thyroid axis disease may also cause rapid cycling.
For those with a rapid cycling pattern, the prognosis is poorer than is that for others with bipolar disorder, as is the response to lithium. Treatment with high-dose thyroid hormone may be effective, even if there is no thyroid disease (three studies). Carbamazepine or other anticonvulsants may be particularly effective for both acute and prophylactic treatment of bipolar disorders with a rapid cycling pattern, according to at least four studies. (For a review of these studies, see Bauer and Whybrow, in press.)
Under DSM-III-R, bipolar disorder not otherwise specified is a residual category for disorders with manic or hypomanic features that do not meet the criteria for bipolar I disorder. This category presently includes what some investigators have called bipolar II disorder. Bipolar II disorder usually consists of multiple episodes of major depression interspersed with episodes of hypomania. If a manic episode develops, the diagnosis is changed to bipolar I disorder.
Bipolar II disorder has an earlier age of onset than does major depressive disorder and displays a relatively stable lifetime course, although 5 to 17 percent of bipolar II patients develop mania and convert their diagnoses to bipolar I disorder over 5 to 40 years. Compared with patients with major depressive disorder, those with bipolar II disorder have more frequent episodes, increased frequency of suicide attempts, greater propensity to commit suicide following hospital discharge, and higher familial incidence of suicide.
In addition to bipolar II disorder, the category of bipolar disorder not otherwise specified includes various bipolar conditions thar are insufficiently clear-cut in their clinical presentation to be definitvely considered either bipolar I or bipoar II disorders. Examples include single or recurrrent hypomanic episodes withouth enterepisode subsyndromal deprressive symptoms (which if continuous, would be diagnoses as cyclothymic disorders) and without major depressive episodes *which if, present, would lead to a bipolar II diagnosis.) As a category, bipolar disorder not otherwise specified has not been subjected to randomized controlled treatment trials.
Guideline: Cyclothymic disorder features numerous, alternating hypomanic and mild derpessive periods, lasting days to week and nearly continuous. There are few truly symptom-free periods. The symptoms fluctuate, but never reach the severity/duration criteria of major depressive or manic episodes. The course is chronic, often lasting years. (Strength of Evidence = A.)
A variety of clinical, family history, biologic, and treatment response characteristics suggest that this “subsyndromal” condition falls within the domain of mood disorders. A subgroup of those with symptoms of cyclothymic disorder do not have a significant family history of mood disorder or do not respond to lithium. However, various personality traits, temperaments, and disorders are associated with cyclothymic disorder. Socially problematic behaviors, such as marital discord, promiscuity, poor work performance, and substance abuse, are recognized as psychosocial complications of such subsyndromal mood disorders.
Accurate clinical assessment of these patients is difficult, especially when they manifest mood instability among their symptoms. For example, patients with borderline personality disorder frequently manifest a variety of mood symptoms, making it difficult to distinguish their illness from a mood disorder. On the other hand, many patients with borderline personality disorder may have unrecognized, and hence untreated, mood disorders. Given the likely clinical heterogeneity of cyclothymic disorder and its similarities to selected personality disorders, the clinician should carefully and comprehensively evaluate the conditions of patients with subtle, often more chronic, mood symptoms.
The onset of cyclothymic disorder is generally before age 30. During a 1- to 2-year followup of patients with cyclothymic disorder, 6 percent were reclassified as having bipolar I and 30 percent as having bipolar II disorder (Akiskal, Khani, and Scott-Strauss, 1979). However, this followup period is likely to be too short to assess the ultimate outcome of cyclothymic disorder. On the other hand, these findings indicate that a significant number of patients with cyclothymic disorder do go on to develop a formal bipolar condition.
The lifetime prevalence of cyclothymic disorder is 0.4 to 1.0 percent (Weissman and Myers, 1978). Cyclothymic disorder was diagnosed in 3 to 10 percent of a mental health clinic population (Akiskal, Khani, and Scott-Strauss, 1979).
Guideline: The clinical features of major depressive episodes are more similar than different in children, adolescents, adults, and geriatric patients; in men and women; and in all ethnic groups. (Strength of Evidence = A.)
For children, it is important to differentiate between behavioral problems in those who are primarily depressed and depression in those who have a primary behavioral disorder. In the former, behavioral problems are less severe and follow the onset of depression. In the latter, the behavioral problems are more severe and chronic, and they precede the onset of depression.
In prepubertal children, boys and girls seem equally affected with major depressive disorder. After puberty, girls are two to three times more likely to be affected than are boys. The prevalence of clinical depression is reported to be 0.8 percent in preschool children, 2.0 percent in school-aged prepubertal children, and 4.5 percent in adolescents. In clinical samples, the prevalence of depression in children and adolescents is estimated to be 58 percent in educational clinics, 28 percent in outpatient psychiatric clinics, and 40 to 60 percent in psychiatric hospitals, compared to 7 percent in hospitalized pediatric patients (Weller and Weller, 1990). The offspring of one or more parents with a history of major depression are at markedly higher risk for major depression, including prepubertal onset illness (Weissman, Gershon, Kidd, et al., 1984).
The course of major depressive disorder in prepubertal children and adolescents has not yet been fully studied. On the other hand, one study found that up to 30 percent of adolescents hospitalized with severe major depressive disorder may go on to develop bipolar disorder over 3 to 8 years (Strober and Carlson, 1982). Early onset of major depression (first episode prior to age 20) is associated with a greater likelihood of a more recurrent pattern in adulthood (Giles, Jarrett, Biggs, et al., 1989, Grof, Angst, and Haines, 1974). To date, evidence suggests a problematic course for at least some patients with onset of major depressive disorder prior to age 20—particularly those with a positive family history.
Depression in the elderly is a significant matter for primary care practitioners because of its prevalence and the complexity of the differential diagnosis. The clinical presentation of depression in the elderly is similar to that in other adults. However, it can be difficult to distinguish depression from dementia in those over age 65, as some symptoms of depression (e.g., disorientation, memory loss, and distractibility) may suggest dementia. Coexisting major-depressive disorder and dementia are more common than is pseudodementia, and they tend to occur early in the course of Alzheimer’s disease. The most representative prevalence estimate for elderly hospitalized patients with major depressive disorder is 6.0 to 11.5 percent.
The course of major depressive disorder or DNOS in the elderly is poorly studied. It is known from studies of adults that the co-occurrence of medical disorders is a poor prognostic factor in the longer term course of illness. The practitioner must consider the confounding problems created by co-morbid medical conditions in older patients with mood symptoms’ as well as the concurrent use of selected prescription medications and occult alcohol or substance abuse (Table 6). Table 6. Confounds in the diagnosis and treatment of depression in the elderly
|
| Contents | Previous | Next |