| Contents | Previous | Next |
|
There are several professional associations that promote ethical standards of practice for counselors and psychotherapists. Some of these include the American Association for Marriage and Family Therapy, American Association of Pastoral Counselors, American Counseling Association, American Psychological Association and the National Association of Social Work. (Contact information may be found in the appendix).
This chapter will present some general guidelines for standards of practicing clinical supervision. Members of professional associations are responsible for knowing and practicing within the standards promulgated by their respective organizations.
The first recommended standard is documentation. Clinical supervisors should document these five key supervisory relationship elements:
The existence of the supervisor/supervisee relationship is documented with an Informed Consent & Clinical Supervision Agreement. A sample agreement follows this discussion. At a minimum, this agreement should contain:
The supervisor should briefly describe his or her clinical supervision model. Minimally this should include the model's assumptions, the perceived roles of the supervisor and the supervisee and the model's limitations. Next, any known risks presented by the model should be described.
The methodology for evaluating the supervisee's competence to practice counseling or psychotherapy should be described. This section should minimally include what standards will be used, how competence will be measured, how feedback will be given and how coaching will be provided to continuously improve the supervisee's skills and competence in delivering counseling or psychotherapy services.
Confidentiality must be addressed relating to the information arising from this relationship. Any limitations or exceptions to confidentiality should also be clearly described.
Finally, a statement of agreement that the supervisee is voluntarily engaging the clinical supervisor for supervision should be included. This statement should summarize that the supervisee understands the supervisor's personal clinical supervision model and its inherent risks, competency appraisal process to be used and an expressed interest in initiating clinical supervision with this supervisor on a voluntary basis.
Informed Consent & Clinical Supervision AgreementMy Personal Clinical Supervision Model In this section, the clinical supervisor describes his or her personal model for supervision. Minimally this should include the model's assumptions, the perceived roles of the supervisor and the supervisee and the model's limitations. Risks of Model In this section, any known risks presented by this model should be described. Competency Appraisal Process & Coaching I will draft quarterly, formal competency appraisals and discuss them with you documenting your skills competency based upon mutually agreed upon skills competency standards. I will utilize a three-fold competency coaching process. Competency coaching begins with my collective observations of your on the job competence. Next, I will compare observed behaviors and competence to our mutually predetermined goals and share this information with you. Together, we will formulate strategies for incremental learning and incremental improvement toward achieving your competency goals. Third, I will give feedback to you addressing both what appeared to be effective effort and what could be demonstrated differently. By observing behaviors, formulating strategies and providing feedback, I can provide you with assistance and motivation as you strive to implement these competency improvement strategies and hit your targeted goals. This three-fold process is ongoing. If unethical behavior occurs, I will be required to notify the appropriate professional bodies. We will address the circumstances as necessary in supervision. As an integral part of your clinical supervision, you may be requested to complete additional reading assignments, attend and participate in certain courses, workshops or seminars, or participate in additional supervision hours if additional education, training or coaching is necessary for your development and ability to practice as a therapist. Should personal issues appear to be negatively affecting your ability to deliver therapeutic services to your clients, you may be required to seek personal therapy if you desire to continue to practice as a supervisee under my supervision. My supervision may focus on your personal functioning as it impacts your therapeutic skills and interventions but it is not therapy nor should it serve as a substitute for personal therapy. The primary focus of supervision is to improve your competence as a therapist in improving the functioning of your clients, while the primary focus of personal therapy is to improve the functioning of the client. Confidentiality As your clinical supervisor, I will maintain confidentiality with all information that arises within the context of our supervision relationship, including information about the supervision process notwithstanding the mandated exceptions (information regarding immediate danger and/or harm; court-ordered releases). Formal competency appraisals are also treated confidentially. I understand that if I should breach the Confidentiality Agreement - Supervisee it may result in the termination of my supervision with the undersigned individual and/or group supervisors and the automatic termination of my Informed Consent & Clinical Supervision Agreement. Voluntary Choice of Supervision I understand the supervisor's personal clinical supervision model, the inherent risks and the competency appraisal process described in this Informed Consent: Clinical Supervision Agreement and I am interested in initiating clinical supervision with my supervisor as described within this document. ________________________________/____/_____
________________________________/____/_____
________________________________/____/_____
|
The clinical supervisor can document the occurrences of supervision sessions by utilizing a series of forms. These include:
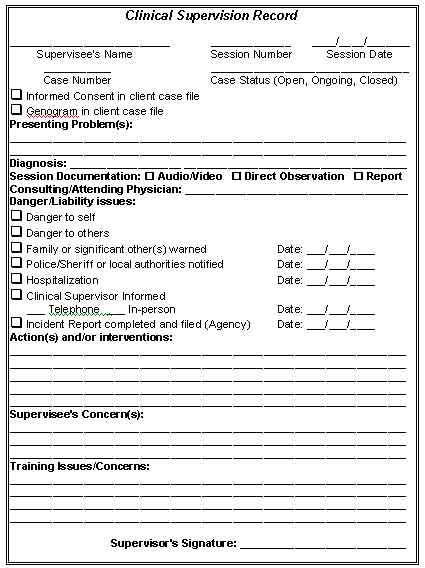
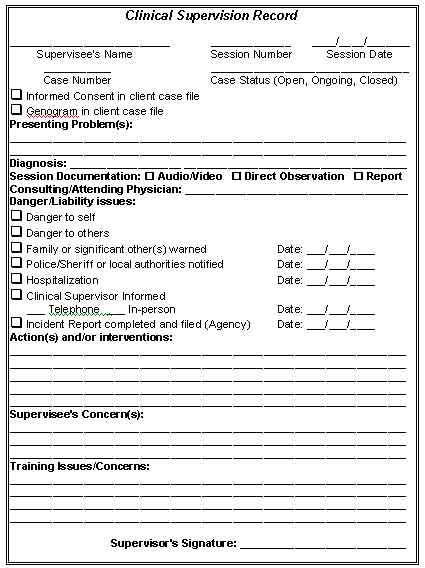
The Clinical Supervision Record documents the important elements and activities of the clinical supervision session. One form should be completed for each client case presented in each clinical supervision session.
The supervisee's name is recorded at the top of the form. Next the supervision session number and session date are recorded. Each client should be assigned a case number to preserve client anonymity in these records. The client's case status should also be noted, e.g., Open, Ongoing, Closed.
An indication should be made that the Informed Consent & Release for clinical case presentation is in the client record. The presence of a Genogram for family therapy cases should also be recorded.
Next, the client's presenting problems should be outlined. This is followed by a diagnosis. The method for documenting the counseling or therapy should be indicated as "audio/video," "direct observation" or "report" format.
If a consulting or attending physician is on the case, the name should be recorded. An indication of any danger or liability issues should also be noted.
Actions and or interventions used in the counseling should be described. Any concerns on the part of supervisee should be addressed and documented.
Finally, any training issues or concerned should be documented and added to the competency appraisal and coaching documentation process for follow-up.
A sample "Clinical Supervision Record" form follows:
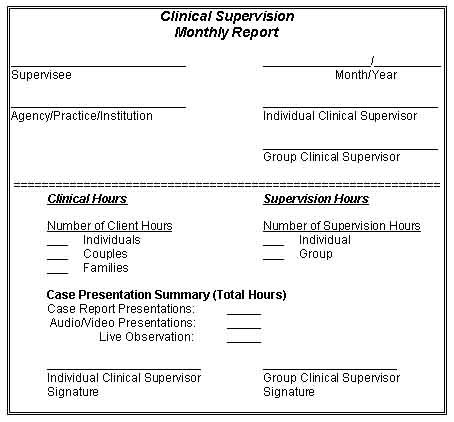
The Clinical Supervision Monthly Report documents a summary of the clinical hours delivered by the supervisee and the supervision hours provided by the supervisor during a monthly period. The clinical hours are broken down into three categories: Individuals, Couples and Families. The supervision hours are broken down into two categories: Individual and Group. A Case Presentation Summary is broken down into three categories: Case Report Presentations, Audio/Video Presentations and Live Observations. The total hours for each category are recorded for the month period.
A sample Clinical Monthly Supervision Report follows:
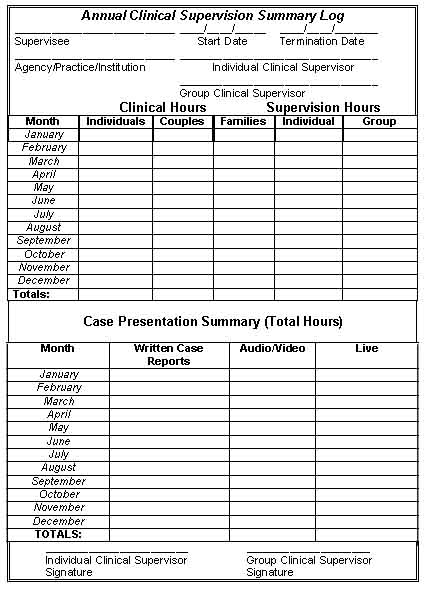
The third documentation form is the Annual Clinical Supervision Summary Log. This form is used to document and summarize a one-year period of clinical supervision.
The supervisee's name and the start date and termination date of the clinical supervision relationship are recorded at the top of the form. The agency, practice or institution is identified and the individual and group clinical supervisors are identified.
A monthly summary of both clinical and supervision hours are recorded and totaled. This is followed by a monthly summary of case presentations broken down into Written Case Reports, Audio/Video Presentations and Live Observations. The total hours are recorded monthly and totaled for each category. Both the individual and group clinical supervisors sign the form at the bottom.
A sample Annual Clinical Supervision Summary Log follows:
The fifth element of the clinical supervision relationship that should be documented is the existence of informed consent and confidentiality agreements. This should include both an agreement of confidentiality by the supervisee and an informed consent and release for documentation and case presentation for clinical supervision from each client.
The first recommended form is an Informed Consent & Release: Audio/Video Recording & Case Presentation Permission. A sample form follows:
Informed Consent & Release: Audio/Video Recording & Case Presentation PermissionI, _______________________________ grant permission to _______________________________, to record our sessions with either audio or video tape and present such recordings to his/her individual and/or group clinical supervisor and supervision group for the purpose of supervision of my case from this date: _____/____/_____ to _____/_____/_____. I understand that all group supervision participants and either individual or group supervisors will sign a Confidentiality Agreement form prior to hearing or viewing any of my case recordings or case progress/history notes. I understand that any breach of the confidentiality agreement may result in their immediate dismissal from individual supervision and/or group supervision and the notification of any applicable agencies or professional associations and their respective Ethics Committees to which they may belong. I have been made aware that the original copy of this informed consent and release shall remain in my confidential client file and my therapist will give a copy of this form to his/her supervisor(s) with my last name blotted out. I agree to the stipulations contained within this informed consent and release form. ________________________________/____/_____
I agree to the stipulations contained within this informed consent and release form with the following exceptions or conditions: ______________________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ________________________________/____/_____
________________________________/____/_____
________________________________/____/_____
________________________________/____/_____
|
The second recommended form is the Confidentiality Agreement - Supervisee. This documents the supervisee's agreement to maintain the confidentiality of his or her clients and the clients of peers (other supervisees in the practice, agency, institution or clinic). This includes a commitment to refrain from revealing any identifying information regarding clients during case presentations in either individual or group supervision. A commitment is also made to protect the confidentiality of client records by bringing minimal information for supervision sessions and only Genograms that lack all client identification data.
An acknowledgment that the supervisee will not present a case in supervision without first obtaining a prior signed Informed Consent & Release: Audio/Video Recording & Case Presentation Permission form for each client case to be presented in supervision should also be included.
It is also necessary to document the supervisee's agreement not to discuss clients or cases with anyone other than his or her clinical supervisor, or the supervision group without a signed, written release of confidentiality and informed consent agreement approved by the practice, agency, institution or clinic. It should also be clearly stated that the supervisee understands that he or she should not discuss client cases with family members, significant others, friends, colleagues, supervisors, faculty, referral sources, administrators and other students who are not a part of the clinical supervision group.
Finally, the supervisee's understanding of the consequences of breaching confidentiality should be acknowledged and the document should be signed by all parties to the supervision relationship, the supervisee and both the individual and group clinical supervisors.
A sample Confidentiality Agreement - Supervisee form follows:
Confidentiality Agreement - SuperviseeI, __________________, indicate by my signature below, that I agree to maintain the confidentiality of my clients and the clients of my peers (other supervisees in the practice/agency/institution/clinic). I will refrain from revealing any identifying information regarding my clients when presenting cases in either individual or group supervision. I will protect the confidentiality of my client's records by bringing minimal information for supervision and Genograms will not contain any identifying data. I understand that case notes and client files shall not be removed from the office/agency/institute/clinic. I will not present a case in supervision without obtaining a prior signed Informed Consent & Release: Audio/Video Recording & Case Presentation Permission form. I will not discuss clients or cases with anyone other than my clinical supervisor, or my supervision group unless a person or persons are so designated on a Release of Confidentiality form. I understand that this includes my family, significant others, friends, colleagues, supervisors, faculty, referral sources, administrators and other students. I understand that if I should breach this confidentiality agreement it may result in the termination of my supervision with the undersigned individual and/or group supervisors and the automatic termination of my Informed Consent & Clinical Supervision Agreement. I further understand that a breach of confidentiality may also result in one or both of the undersigned supervisors reporting this breach to the agency/institute/clinic and the Ethics Committee of any and all professional associations to which I belong. This Agreement shall remain in effect from the date of execution until the termination of supervision with the undersigned supervisor(s). ________________________________/____/_____
________________________________/____/_____
________________________________/____/_____
|
The second clinical supervision practice standard is to comprehensively and systematically cover the general aspects of the clinical supervision relationship with each supervisee. Six general areas are essential topics for dialogue. They include:
Mutual understanding and agreement around the supervisee's expectations and learning goals are an important starting point in any new clinical supervision relationship. The clinical supervisor should invite and encourage open dialogue around the supervisee's expectations for the supervisory process. Some initial questions might include:
What do you hope to gain from your clinical supervision?
How will you know if your clinical supervision was a successful process?
What concerns do you have about your clinical supervision?
What expectations do you have of your clinical supervisor?
Each supervisee should be challenged to develop a set of learning goals when they begin a clinical supervision relationship. These learning goals should be discussed and modified as necessary with the clinical supervisor and documented in a learning contract between the clinical supervisor and the supervisee.
The learning contract should be viewed and used as a fluid document open for revisiting and revising throughout the course of the supervisory process. The primary objective for creating it is to provide a series of checkpoints to assist in assessing and evaluating the supervisee's progress in incremental learning and incremental skills development.
Each learning goal should be written in the GET SMART format.
Growth
Is it a "stretch" outside the supervisee's comfort zone? Will the supervisee grow as a result of achieving it?
Efficacious
Does it have the power to produce the intended results? Is it adequate enough to achieve the desired outcome?
Tangible
Does the targeted outcome have substance or value? Can the targeted outcome be clearly defined and understood?
Specific
Is the targeted outcome specially suited for a given use or purpose?
Measurable
Is the targeted outcome capable of being measured? Are there time frames? Are there dates? Are there scores?
Action-oriented
Is some specific behavior to be completed or accomplished?
Results-based
Is something expected to occur as a consequence of successfully achieving the targeted outcome?
Targeted
Does the goal focus on a specific, identifiable outcome?
The second general area for discussion is the supervisee's related education, clinical training and related experiences. Talking about the supervisee's graduate education will give the clinical supervisor insights into the supervisee's educational preparation for clinical practice. Knowing what specific coursework was taken will also help to provide the clinical supervisor with insights into the educational foundation of the supervisee's training.
It may also be helpful to determine whether or not the program was accredited by the COAMFTE (Commission on Accreditation for Marriage and Family Therapy Education), approved by the APA (American Psychological Association), or accredited by the NLNAC (National League for Nursing Accrediting Commission)?
Talking about the supervisee's internship experiences will assist the supervisor in determining the types of cases the supervisee may be able to treat during the supervision process. This discussion should include the location, length of time spent at that location, type of clients treated, size of caseload, the total number of clinical hours completed and the type and style of supervision used.
If the supervisee has completed additional clinical training or continuing education experiences, these should be discussed as well. This would include conferences, workshops, post-graduate internships, fellowships and hospital or agency in-service education programs.
Any relevant certifications should also be reviewed and discussed too. These could include addictions counseling (CAADAC, CAC, CAS), professional nursing certifications/registrations (RNC), counseling (NCC).
A careful examination of the supervisor's clinical supervision model and personal supervision philosophy is important in aiding the supervisee's understanding of the supervisor's approach, orientation, and expectations in the supervisory relationship. A dialogue should also occur seeking contrasts and comparisons with the supervisee's philosophy of the supervisory relationship.
Each supervisee should be required to read, sign, and date an Informed Consent & Clinical Supervision Agreement form prior to the commencement of the clinical supervision relationship. The length of the supervisory relationship should be discussed and agreed to at this time too. This document should be placed in the supervisee's personnel folder.
Next, the supervisor and supervisee should review and discuss the Confidentiality Agreement - Supervisee form. This executed document should also be filed in the supervisee's personnel folder.
Other forms are also recommended to accurately document the supervisory relationship and the type, frequency and duration of the supervisee's experiences. These forms should also be reviewed and discussed to ensure that the supervisee understands the intent and purpose of these documents. These forms include the: Clinical Supervision Record Form, Clinical Supervision Monthly Report Form and Annual Clinical Supervision Summary Log Form.
There are numerous legal and ethical issues that may arise during the course of the supervisory relationship. Many of these issues are best handled proactively and preventively. Engaging supervisees in dialogue over these issues can assist the supervisor in uncovering potential areas in which the supervisee may need additional training and education.
Scope of Practice
Scope of practice issues should be identified and defined. You, as the supervisor, should know your scope of practice and be able to articulate it to your supervisees. This will assist you in determining each supervisee's scope of practice and how it can be expanded within your own.
Disclosure of Supervisory Relationship
Disclosure of the supervisory relationship to clients is an essential, ethical action. It is recommended that you instruct your supervisees to use the Informed Consent & Release: Audio / Video Recording & Case Presentation Permission form to document this discussion and disclosure with each client assigned to them.
Codes of Ethics
Each professional association has a set of ethical guidelines or a code of ethics by which members are expected to practice their profession. Copies of various codes of ethics should be provided to each supervisee. In cases where either the supervisor or the supervisee is a member of a specific professional association, that association's code of ethics should also be included. The American Association for Marriage and Family Therapy, American Psychological Association, American Nurses Association, National Association of Social Workers and the American Counseling Association all have codes of ethics governing member's conduct (See Resources Section for contact information).
Confidentiality: Issues & Limits
Confidentiality issues between the supervisor and supervisee, supervisee and clients, and supervisees in a group supervision experience should be discussed in detail. The limits of confidentiality and mandated reporting responsibilities should be explored as well.
Emergency Contact Procedures
Although emergencies may be infrequent, whenever one occurs it is critical that policies and procedures have been created and reviewed beforehand to ensure that everyone's safety and well-being are managed effectively. Even if you are a solo practitioner supervising one supervisee in your private practice it is essential that you develop emergency contact procedures to safeguard your clients, your supervisee and yourself.
At a minimum, there should be contact phone numbers for yourself and a back-up person in your absence. Many clinicians use an answering service or a voice mail and pager service for emergency contacts during a clinical emergency.
In the event of a suicidal or homicidal client, additional emergency procedures should be carried out. Emergency phone numbers for the local law enforcement agency, local county mental health, and the psychiatric emergency response team (if available in your area) should also be easily accessible to staff members.
Discussing assessment and evaluation procedures and emergency interventions with clients who are actively suicidal, homicidal or an immediate threat or danger to themselves or others is another important part of preparing for clinical emergencies before they arise.
Dual Relationships
A dual relationship is created at any time a counselor or therapist engages in two roles simultaneously or sequentially with another person with whom they currently have or previously have had a professional relationship involving the delivery of professional services. These dual roles are not restricted to a professional category. For the purposes of our discussion in this text, we will focus on dual relationships between clinical supervisors and supervisees. Some examples of dual relationships include:
Simultaneous Relationships (Between therapist and another person)
Sequential Relationships (Between therapist and another person)
Most professional associations for professional counselors and therapists have specific standards in their Codes of Ethics regarding dual relationships. Some samples follow:
American Association for Marriage and Family Therapy, Revised AAMFT Code of Ethics, effective July 1, 2001.
1.3 Marriage and family therapists are aware of their influential positions with respect to clients, and they avoid exploiting the trust and dependency of such persons. Therapists, therefore, make every effort to avoid conditions and multiple relationships with clients that could impair professional judgment or increase the risk of exploitation. Such relationships include, but are not limited to, business or close personal relationships with a client or the client’s immediate family. When the risk of impairment or exploitation exists due to conditions or multiple roles, therapists take appropriate precautions.
1.4 Sexual intimacy with clients is prohibited.
1.5 Sexual intimacy with former clients is likely to be harmful and is therefore prohibited for two years following the termination of therapy or last professional contact. In an effort to avoid exploiting the trust and dependency of clients, marriage and family therapists should not engage in sexual intimacy with former clients after the two years following termination or last professional contact. Should therapists engage in sexual intimacy with former clients following two years after termination or last professional contact, the burden shifts to the therapist to demonstrate that there has been no exploitation or injury to the former client or to the client’s immediate family.
1.7 Marriage and family therapists do not use their professional relationships with clients to further their own interests (AAMFT, 2001).
The American Association of Pastoral Counselors, Code of Ethics, Amended April 28, 1994.
The American Counseling Association, Code of Ethics and Standards of Practice.
A.6. Dual Relationships
a. Avoid When Possible. Counselors are aware of their influential positions with respect to clients, and they avoid exploiting the trust and dependency of clients. Counselors make every effort to avoid dual relationships with clients that could impair professional judgment or increase the risk of harm to clients. (Examples of such relationships include, but are not limited to, familial, social, financial, business, or close personal relationships with clients.) When a dual relationship cannot be avoided, counselors take appropriate professional precautions such as informed consent, consultation, supervision, and documentation to ensure that judgment is not impaired and no exploitation occurs. (See F.1.b.)
b. Superior/Subordinate Relationships. Counselors do not accept as clients, superiors or subordinates with whom they have administrative, supervisory, or evaluative relationships.A.7. Sexual Intimacies With Clients
a. Current Clients. Counselors do not have any type of sexual intimacies with clients and do not counsel persons with whom they have had a sexual relationship.
b. Former Clients. Counselors do not engage in sexual intimacies with former clients within a minimum of 2 years after terminating the counseling relationship. Counselors who engage in such relationship after 2 years following termination have the responsibility to examine and document thoroughly that such relations did not have an exploitative nature, based on factors such as duration of counseling, amount of time since counseling, termination circumstances, client's personal history and mental status, adverse impact on the client, and actions by the counselor suggesting a plan to initiate a sexual relationship with the client after termination.
All three codes of ethics share common themes concerning dual relationships. These include the exploitation of influence/power, trust, and dependency.
Counselors are in a unique position of influence and power over their clients. This power differential is so significant that many would argue there is an actual inability on the part of the client to make an informed consent decision regarding a dual relationship. Therefore, the responsibility for avoiding such relationships falls completely on the shoulders of the therapist.
Clients place a great deal of trust in their counselors. They also depend upon them for ethical, competent and professional service delivery. This dependency should be regarded with care and all decisions should be made with the client's best interests and well-being at the forefront.
Professional Boundaries
Boundaries are differentiations between self and other and between self and the universe. As newborn children, we are thrust into a turbulent, new existence where we experience the familiar and the unknown. We cannot differentiate between self and others. A lifelong process is begun in which we wrestle with self-creation and how to function as an individual self in a world of others.
Boundaries during infancy, childhood and adolescence allow us to experience security and containment, support and independence, belonging and autonomy, and joining and separating, all of which can occur without the loss of love, protection, safety or acceptance. They must be simultaneously flexible and restricting yet clearly understood by both the child and the caregiver.
As adults, boundaries continue to serve important roles for creating safety and security within the context of our relationships with one another. We may develop patterns of boundary responses depending on the outcomes of our relationships with others. Some people may establish a pattern of rigid boundaries within which they become so fearful of being hurt by another that they close off themselves from intimacy and closeness. They give up their ability to be resilient and flexible and in the process of attempting to protect themselves, they injure themselves deeply through isolation, withdrawal and loneliness.
Others choose the opposite boundary response and develop patterns of extreme openness, conflict avoidance and a smothering pattern of relating to others. They develop such a deep-seated fear of abandonment that they lose their sense of self in relationship with another. It is almost a state of boundarylessness, within which a sense of self becomes so blurred and undifferentiated that they may come to believe that there is nothing of self left to be rejected by someone else.
The third possible boundary response is the bipolar response. People who choose this pattern of relating to others move from one extreme phase of rigid boundaries to the other extreme phase of boundarylessness. This pattern of relationship choices often creates confusion and frustration because the individual is perceived as unpredictable and unsteady.
Clinical supervisors have a professional responsibility to be aware of and effectively set and manage their own professional role boundaries in relationship to their supervisees. Additionally, they are responsible for effectively managing and directing supervisees in the process of professional role boundary setting and management with their clients.
Professional role definition boundaries may be crossed in both inappropriate and appropriate ways. When a boundary is crossed inappropriately, it is called a boundary violation. Professional role boundary violations result in harm, damage and exploitation to someone else. Professional role boundary crossings that are not violations may be classified as a change in role or behavior that does more good than harm to another without the occurrence of exploitation.
Professional role boundaries may be grouped into several general categories. These include:
Money -- professional fees, insurance reimbursement, sliding scales
Time -- session time frames and time of day sessions are held
Location -- physical space and environmental settings for sessions
Self-disclosure -- from supervisor/counselor to supervisee/client
Physical contact -- physical contact including handshakes, hugs, embraces, touching arms, shoulders, backs
Gifts -- giving and receiving gifts to or from supervisees or clients
Favors -- receiving favors from supervisees/clients
Confidentiality -- discussing other supervisee's supervision or other client's treatment progress or therapeutic issues
Gabbard (1995) identifies a set of warning signs that can alert both therapists and clients to the possibility that boundary violations may be occurring. These include such therapist behaviors as:
Like many professions, counselors are not exempt from the risks of burnout, unmanageable stresses and the potentially damaging effects of unattended transference and countertransference issues. Supervisors should discuss each of these issues with their supervisees. Together, strategies for coping with them can be formulated and implemented as necessary.
Core competencies and supporting standards should be developed for the supervisee in the form of a position description (job description). These should be discussed in detail with the supervisee and used as a baseline for co-creating learning goals. A proposed set of seven competencies and the supporting standards are presented later in Chapter Five: Recruiting Competent Supervisees.
Creating a workplace environment that fosters maximum professional skills development and learning involves communication and understanding around practice logistics. The clinical supervisor should dialogue with the supervisee about the various mechanics, procedures and logistics impacting the day-to-day activities in the office/agency/institution environment.
Assigning Clients To Supervisees
The clinical supervisor is responsible for the client's treatment when an unlicensed counselor is providing psychotherapeutic services under his or her direction. Before a supervisor can make an effective client referral to his or her supervisee he or she must know the client's history, presenting problems, provisional diagnosis and a treatment plan.
Agencies may designate an Intake Clinician to conduct all intake assessments. If this practice is used, the Intake Counselor should be licensed and highly experienced in conducting initial assessments, taking comprehensive histories and functioning as a liaison with referring agencies, professionals and previous treatment providers.
By personally conducting the initial intake session and speaking with any referral sources and previous treatment providers, the supervising clinician can make an accurate assessment of the client's needs and the supervisee's skills, training and abilities to address them. This practice should be considered when an Intake Counselor is not available such as in private practice settings or small agencies.
If the clinical supervisor conducts the initial intake, the supervisee and the clinical supervisor could co-facilitate the first treatment session together so that continuity of care and a smooth transition are provided to clients.
Supervisor's Fee For Supervision Services
Some discussion is necessary around the supervisor's fee and payment arrangements for the delivery of clinical supervision services. Note that in California it is illegal for a supervisor to charge an intern in a private practice setting for supervision:
§4980.43 (f) An intern employed in a private practice setting shall not pay his or her employer for supervision. While an intern may be either a paid employee or a volunteer, employers are encouraged to provide fair remuneration (California Business and Professions Code, §4980.43 (f)).
Clarification of the supervisee's work status is also necessary. Is the supervisee an employee, independent contractor, or volunteer? Note that in California it is illegal for interns or trainees to be paid as independent contractors.
§4980.43(b) The requirements of this chapter regarding gaining hours of experience and supervision are applicable equally to employees and volunteers. Experience shall not be gained by interns or trainees as an independent contractor.
§4980.43(f) When an intern is employed in a private practice setting by any licensee enumerated in this section, … ,the intern shall be under the direct supervision of a licensee enumerated in subdivision (f) of Section 4980.40 who shall be employed by and practice at the same site as the intern's employer. While an intern may be either a paid employee or a volunteer, employers are encouraged to provide fair remuneration.
§4980.43(i) Trainees and interns shall not receive any remuneration from patients or clients, and shall only be paid by their employer (Cal. Bus. & Prof. Code, §4980.43(b), (f), (i)).
Additionally supervisees should clearly know where the supervision will be conducted, how frequently sessions will occur and how long each session will last. Supervisors should be aware that many state laws set parameters around the ratios between supervision sessions and client hours, the duration of supervision sessions and the number of supervisee participants in group supervision sessions to qualify the supervisee for licensure experience hours.
Supervisees should also be made aware of how clients will be referred or assigned for clinical treatment. The process for determining the supervisee's appropriate skill and experience level and assessing a client's initial diagnosis and treatment needs are also important points of discussion.
Many supervision formats and structures are available. Supervisees should be informed of the various methods employed by the supervisor. These include audio taped client sessions, video taped client sessions, live observation (one-way mirror), co-therapy, and case presentations. If both individual and group supervision sessions are used, then the role of other supervisees in the group should also be discussed. Will they be observers, co-supervisors, co-supervisees?
Talking about supervision session expectations beforehand can greatly reduce future conflicts around misunderstandings regarding punctuality, smoking, eating and drinking and preparation beforehand (cueing tapes, preparing case notes, etc.).
In agency or institutional settings, copies of the employee handbook, policy and procedure manual, and benefits documentation should be provided to supervisees. Information about telephone procedures, answering service and paging, on-call coverage, scheduling, office hours, parking and scheduling consultation rooms is also important for maintaining a smooth operation.
A worksheet/checklist follows which may be used to document these dialogues between the clinical supervisor and the supervisee. This document should be kept in the supervisee's personnel file after it is completed.
Primary Clinical Supervision Discussion Points |
||
| 1 | Expectations, Learning Goals & Learning Contract | |
| Clarify supervisee's expectations from clinical supervision | ||
| Establish supervisee's personal and career learning goals directly related to clinical supervision relationship | ||
| Create a detailed learning contract for clinical supervision relationship | ||
| Contract for periodic re-visitation of learning goals and learning contract | ||
| Date completed: _____/____/_____ | ||
| 2 | Related Education, Clinical Training & Experience | |
Discuss graduate degree program supervisee completed
|
||
Discuss additional clinical training and educational experiences
|
||
| Date completed: _____/____/_____ | ||
| 3 | Clinical Supervision Model & Personal Philosophy | |
| Examine supervisor's clinical supervision model and personal philosophy of supervision and compare / contrast with supervisee's expectations and philosophy of the supervisory relationship | ||
| Review and Sign Informed Consent & Clinical Supervision Agreement | ||
| Length of supervisory relationship | ||
| Review and Sign Confidentiality Agreement - Supervisee Form | ||
| Review Clinical Supervision Record Form, Clinical Supervision Monthly Report Form and Annual Clinical Supervision Summary Log Form | ||
| Date completed: _____/____/_____ | ||
| 4 | Legal & Ethical Issues | |
| Scope of practice issues | ||
| Disclosure of supervisee/supervisor relationship to clients & use of Informed Consent & Release: Audio / Video Recording & Case Presentation Permission Form | ||
| Professional Association Code of Ethics (AAMFT, APA, ANA, ACA, NASW, etc.) | ||
| Confidentiality issues: (therapist / client, supervisee / supervisor, group supervision) | ||
| Confidentiality limitations: mandated reporting issues, court orders and subpoenas | ||
| Emergency contact procedures | ||
| Dual relationships | ||
| Professional boundaries: (supervisee / client, supervisee / supervisor, supervisee / supervisee in group supervision) | ||
| Coping with burnout, stress, transference / countertransference | ||
| Date completed: _____/____/_____ | ||
| 5 | Core Competencies & Standards | |
| Practice Management Competency | ||
| Therapeutic Milieu Competency | ||
| Processing Competency | ||
| Integration Competency | ||
| Therapeutic Structure Competency | ||
| Interventions Competency | ||
| Professional Development Competency | ||
| Date completed: _____/____/_____ | ||
| 6 | Practice Logistics | |
| Supervisor's fee & payment arrangements | ||
| Clarification of Supervisee's status (employee, contractor, etc.) | ||
| Location, times, frequency and duration of supervision sessions | ||
| Arrangements for client referrals | ||
| Arrangements for fee-splitting between supervisor/supervisee | ||
Discuss graduate degree program supervisee completed
|
||
Discuss additional clinical training and educational experiences
|
||
Session Expectations
|
||
Agency Worksite Policies & Procedures
|
||
| Date completed: _____/____/_____ | ||
The clinical supervisor and the supervisee both indicate by their signatures below that all the primary clinical supervision discussion points contained in this document have been discussed, understood and mutually agreed upon by both parties. ___________________ ___/___/___ ___________________ ___/___/___
|
||
Identify the five key supervisory relationship elements that should be documented
How would you prepare your own Informed Consent & Clinical Supervision Agreement?
How frequently would you conduct competency appraisals with supervisees?
How will you conduct clinical supervision? Live? Audio/Video? Case Reports? Co-Counseling?
Would you add anything to the Primary Clinical Supervision Discussion Points?
How would you implement this tool in your clinical supervision practice?