| Contents | Previous | Next |
Drug therapy is the cornerstone of the many modalities available to manage cancer pain because it is effective, relatively low risk, inexpensive, and usually of rapid onset. An essential principle in using medications to manage cancer pain is to individualize the regimen to the patient (Foley, 1985a).
Three major classes of drugs are used alone or, more commonly, in combination to manage pain in the cancer patient:
Before choosing drugs to manage pain or other symptoms, identify the specific cause(s) of the pain, evaluate its intensity and quality, and then match the drug to the pain intensity and other characteristics. The simplest dosage schedules and least invasive pain management modalities should be used first. After drug therapy has been started, pain should be assessed to determine the ongoing effectiveness of the analgesic therapy. For opioid analgesics, if pain relief is inadequate, the dose should be increased until pain relief is achieved or unacceptable side effects occur. In the case of NSAIDs and adjuvant analgesic drugs, which have ceiling effects to their analgesic efficacy, if the upper limit of the recommended dose is reached and pain relief is not achieved, then that particular drug should be discontinued and a second drug in that class should be used.
Most cancer pain can be managed by oral administration of drugs; however, difficulty in swallowing, gastrointestinal (GI) disturbances that render drug absorption unreliable, the amount of drug required, and many other factors may require alternative routes of administration (Coyle, Adelhardt, Foley, et al., 1990; Grond, Zech, Schug, et al.. 1991). Table 8 summarizes some of the advantages and disadvantages of cancer pain therapies.
A simple, well-validated, and effective method for assuring the rational titration of therapy for cancer pain has been devised by WHO (World Health Organization, 1990). It has been shown to be effective in relieving pain for approximately 90 percent of patients with cancer (Ventafridda, Caraceni, and Gamba, 1990) and over 75 percent of cancer patients who are terminally ill (Grond, Zech, Schug, et al., 1991). This approach is based on the concept of an analgesic ladder (Figure 2).
The five essential concepts in the WHO approach to drug therapy of cancer pain are:
The first step in this approach is the use of acetaminophen, aspirin, or another NSA1D for mild to moderate pain. Adjuvant drugs to enhance analgesic efficacy, treat concurrent symptoms that exacerbate pain, and provide independent analgesic activity for specific types of pain may be used at any step.
When pain persists or increases, an opioid such as codeine or hydrocodone should be added (not substituted) to the NSAID. Opioids at this step are often administered in fixed dose combinations with acetaminophen or aspirin because this combination provides additive analgesia (Weingart, Sorkness, and Earhart, 1985). Fixed-combination products may be limited by the content of acetaminophen or NSAID, which may produce dose-related toxicity. When higher doses of opioid are necessary, the third step is used. At this step separate dosage forms of the opioid and nonopioid analgesic should be used to avoid exceeding maximally recommended doses of acelaminophen or NSAID.
Table 8. Advantages and disadvantages of pain therapies
| Intervention | Advantages | Disadvantages |
| Oral analgesics Acetaminophen Aspirin NSAlDs |
|
|
| Oral opioids |
|
|
| Transdermal opioids (fentanyQ |
|
|
| Rectal opioids |
|
|
| Subcutaneous infusion |
|
|
| Intravenous infusion |
|
|
| Epidural, intrathecal, and intracerebral ventricular routes |
|
|
| Regional neurolytic blocks |
|
|
| Ablative neurosurgery |
|
|
| Corticosteroids |
|
|
| Anticonvulsants |
|
|
| Antidepressants |
|
|
| Hydroxyzine |
|
|
| Radiation therapy |
|
|
| Relaxation, imagery, biofeedback, distraction, and reframing |
|
|
| Patient education |
|
|
| Psychotherapy, structured support, and hypnosis |
|
|
| Cutaneous stimulation (superficial heat, cold, and massage) |
|
|
| Transcutaneous electrical nerve stimulation |
|
|
| Acupuncture |
|
|
| Peer support groups |
|
|
| Pastoral counseling |
|
|
Pain that is persistent, or moderate to severe at the outset, should be treated by increasing opioid potency or using higher dosages.
Drugs such as codeine or hydrocodone are replaced with more potent opioids (usually morphine, hydromorphone, methadone, fentanyl, or levorphanol), as described below.
Medications for persistent cancer-related pain should be administered on an around-the-clock basis, with additional "as-needed" doses, because regularly scheduled dosing maintains a constant level of drug in the body and helps to prevent a recurrence of pain. Patients who have moderate to severe pain when first seen by the clinician should be started at the second or third step of the ladder.
NSAIDs are used as initial therapy in mild pain because they are effective, are often available over the counter, and can be used effectively in combination with opioids and adjuvant analgesics if pain intensity increases. Acetaminophen is included with this group, even though its anti inflammatory effects are less potent, because it has similar analgesic potency and pharmacologic characteristics. A major advantage of acetaminophen in comparison to other NSAIDs is its lack of effect on platelet function, which makes it less risky to use in thrombocytopenic patients. It is also relatively inexpensive.
NSAIDs decrease levels of inflammatory mediators generated at the site of tissue injury by inhibiting the enzyme cyclooxygenase, which catalyzes the conversion of arachidonic acid to prostaglandins and leukotrienes (Sunshine and Olson, 1989). These mediators sensitize nerves to painful stimuli. Although NSAIDs may also affect the central nervous system, these drugs do not activate opioid receptors and therefore produce analgesia by a different mechanism than opioids. Hence:
In contrast to opioids, NSAIDs do not produce tolerance, physica or psychological dependence, are antipyretic, and have a different spectrum of toxicity. Used as single agents, NSAIDs have a ceiling effect on their analgesic potential, so the use of doses higher than those specified in the package insert is not recommended.
The nonacetylated salicylates such as salsalate, sodium salicylate, and choline magnesium trisalicylate do not affect platelet aggregation profoundly and do not alter bleeding time (Danesh, Saniabadi, Russell, et al., 1987; Day, Furst, Graham, et al., 1987; Estes and Kaplan, 1980; Morris, Sherman, McQuain, et al., 1985; Stuart and Pisko, 1981; Zucker and Rothwell, 1978). Aspirin, the prototype of tl acetylated salicylate, produces an irreversible inhibition of platelet aggregation, which may prolong bleeding time for up to several days after ingestion (Stuart, Murphy, Oski, et al., 1972; Sutor, Bowie, and Owen, 1971; Weiss, Aledont, and Kochwa, 1968). The nonacetylated salicylates, such as sodium salicylate and choline magnesium trisaliq late, have minimal effects on platelet aggregation and do not appear to alter bleeding time clinically (Day, Furst, Graham, et al., 1987; Morris, Sherman, McQuain, et al., 1985; Stuart and Pisko, 1981; Zucker and Rothwell, 1978). Other NSAIDs produce a reversible inhibition of platelet aggregation, which persists while the drug is in the systemic circulation (Schlegel, 1987). Therefore, with the exception of the nonacetylated salicylates noted above, NSAIDs should be avoided if possible in patients who are thrombocytopenic or who have a clotting impairment.
NSAIDs bind extensively to plasma proteins and therefore may be displaced by or may displace other protein-bound drugs such as coumadin, methotrexate, digoxin, cyclosporine, oral antidiabetic agents, and sulfa drugs. Such interactions may enhance therapeutic or toxic effects of either drug. The use of NSAIDs has been associated with both minor (dyspepsia, heartburn, nausea, vomiting, anorexia, diarrhea, constipation, flatulence, bloating, epigastric pain, and abdominal pain) and major (bleeding, ulceration, and perforation) GI toxicities. Serious effects are not always preceded by minor GI effects; patients should be advised to report any GI disturbances.
Hepatic and renal dysfunction or toxicity, which can occur at any time in the course of NSAID therapy, are of particular concern during long-term use (Sunshine and Olson, 1989). The risk of renal dysfunction is greatest in patients with advanced age, preexisting renal impairment, heart failure, hepatic dysfunction, hypovolemia, concomitant therapy with other nephrotoxic drugs such as diuretics, or elevated levels of angiotensin II or catecholamines. Antipyretic and anti-inflammatory effects of NSAIDs may mask the usual signs and symptoms of infections.
Adverse effects of NSAIDs that may appear at any time include:
Even though NSAIDs are effective in relieving mild pain and are opioid sparing for moderate to severe pain, patients who take them, especially if elderly, should be monitored carefully for adverse effects.
Most NSAIDs are available as oral tablets, caplets, or capsules, and several are available as oral liquids. Rectal suppositories of aspirin, acetaminophen, and other NSAIDs are commercially available or can be compounded easily by pharmacists. Ketorolac tromethamine is the only NSAID that is currently available for short-term parenteral administration. Table 9 provides dosing data for acetaminophen and NSAIDs.
Table 9. Dosing data for acetaminophen (APAP) and NSAIDs
| Drug | Usual dose for adults and children > 50 kg body weight | Usual dose for children1 and adults2 < 50 kg body weight |
| Acetaminophen and over-the-counter NSAIDs | ||
| Acetaminophen3 | 650 mg q 4 h 975 mg q 6 h | 10-15mg/kgq4h 15-20 mg/kg q 4 h (rectal) |
| Aspirin4 | 650 mg q 4 h 975 mg q 6 h | 10-15mg/kgq4h 15-20 mg/kg q 4 h (rectal) |
| Ibuprofen (Motrin, others) | 400-600 mg q 6 h | 10 mg/kg q 6-8 h5 |
| Prescription NSAIDs | ||
| Carprofen (Rimadyl) | 100 mg tid | |
| Choline magnesium trisalicylate6 (trilisate) | 1,000-1,500 mg tid | 25 mg/kg tid |
| Choline salicylate (Arthropan)6 | 870 mg q 3-4 h | |
| Diflunisal (Dolobid)7 | 500 mg q 12 h | |
| Etodolac (Lodine) | 200-400 mg q 6-8 h | |
| Fenoprofen calcium (Nalfon) | 300-600 mg q 6 h | |
| Ketoprofen (Orudis) | 25-60 mg q 6-8 h | |
| Ketorolac tromethamine8 (Toradol) | 10 mg q 4-6 h to a maximum of 40 mg/day | |
| Magnesium salicylate (Doan's. Magan, Mobidin, others) | 650 mg q 4 h | |
| Meclofenamate sodium (Meclomen)9 | 50-100mg q 6 h | |
| Mefenamic acid (Ponstel) | 250 mg q 6 h | |
| Naproxen (Naprosyn) | 250-275 mg q 6-8 h | 5 mg/kg q 8 h |
| Naproxen sodium (Anaprox) | 275 mg q 6-8 h | |
| Sodium salicylate (Generic) | 325-650 mg q 3-4 h | |
| Parenteral NSAIDs | ||
| Ketorolac tromethamine8,10 (Toradol) | 60 mg initially, then 30 mg q 6 h Intramuscular dose not to exceed 5 days | |
| 1 Only drugs that are FDA approved as
an analgesic for use in children are included. 2 Acetaminophe^ and NSAID dosages for adults weighing less than 50 kg should be adjusted for weight. 3 APAP lacks the peripheral anti-inflammatory and antiplatelet activities of the other NSAIDs. 4 The standard against which other NSAIDs are compared. May inhibit platelet aggregation for >1 week and may cause bleeding. Aspirin is contraindicated in children with fever or other viral disease because of its association with Reye's syndrome. 5 Not FDA approved for use in children as an over-the-counter drug; has FDA approval for use; in children as a prescription drug for fever. However, clinicians have experience in prescribing ibuprofen for pain in children. 6 May have minimal antiplatelet activity. 7 Administration with antacids may decrease absorption. 8 For short-term use only. 9 Coombs-positive autoimmune hemolytic anemia has been associated with prolonged use. 10 Has the same Gl toxicities as oral NSAIDs. Note: Only the above NSAIDs have FDA approval for use as simple analgesics, but clinical experience has been gained with other drugs as well. |
||
It is impossible to predict which NSAID will be best tolerated by a particular patient: no particular NSAID has demonstrated superiority over others for pain relief. Once an NSAID has been selected, the dose should be increased until pain has been relieved or the maximal recommended dose has been achieved. The duration of analgesm dues not always correlate with the serum half-life of the NSAID. Therefore, the response of the patient should guide the clinician in selecting dosing, intervals of these agents. Because NSAIDs and adjuvant analgesics have ceiling effects to their efficacy, if a patient does not respond to the maximal dose of one NSAID, another should be tried before discontinuation of NSAID therapy. The initial choice of NSAID should be based on the efficacy, safety, and relative expense; generally, the least expensive NSAID should be chosen.
Opioids are the major class of analgesics used in the management of moderate to severe pain because of their effectiveness, ease of titration, and favorable risk-to-benefit ratio. Opioids produce analgesia by binding to specific receptors both within and outside the CNS (Stein, 1993; Hargreaves and Joris, 1993). Opioid analgesics are classified as full agonists, partial agonists, or mixed agonist-antagonists, depending on the specific receptors to which they bind and their intrinsic activity at that receptor.
Commonly used full agonists include morphine, hydromorphone, codeine, oxycodone, hydrocodone, methadone, levorphanol, and fentanyl. These opioids are classified as full agonists because they do not have a ceiling to their analgesic efficacy and will not reverse or antagonize the effects of other opioids within this class given simultaneously. Side effects include constipation, nausea, urinary retention, confusion, sedation, and respiratory depression.
Buprenorphine is a partial agonist. It has a relatively low intrinsic efficacy at the opioid receptor in comparison to full opioid agonists and displays a ceiling effect to analgesia.
Mixed agonist-antagonists in clinical use include pentazocine, butorphanol tartrate, dezocine, and nalbuphine hydrochloride. These drugs have an analgesic ceiling. In contrast to full agonists, these drugs block opioid analgesia at one type of opioid receptor (mu) or are neutral at this receptor while simultaneously activating a different opioid receptor (kappa). Patients receiving full opioid agonists should not be given a mixed agonist-antagonist because doing so may precipitate a withdrawal syndrome and increase pain.
Morphine is the most commonly used opioid for moderate to severe pain because of its availability in a wide variety of dosage forms, its wellcharacterized pharmacokinetics and pharmacodynamics, and its relatively low cost.
Meperidine may be useful for brief courses (e.g., a few days) to treat acute pain and to manage rigors (shivering) induced by medication, but it generally should be avoided in patients with cancer because of its short duration of action (2.5 to 3.5 hours) and its toxic metabolite, normeperidine. This metabolite accumulates, particularly when renal function is impaired, and causes CNS stimulation, which may lead to dysphoria, agitation, and seizures (Kaiko, Foley, Grabin-ski, et al., 1983). Therefore) meperidine should not be used if continued opioid use is anticipated.
Equianalgesic doses of commonly used opioids and starting doses for those drugs are listed in Tables 10 and 11.
Opioid tolerance and physical dependence are expected with longterm opioid treatment and should not be confused with psychological dependence ("addiction"), manifested as drug abuse behavior. The misunderstanding of these terms in relation to opioid use leads to ineffective practices in prescribing, administering, and dispensing opioids for cancer pain and contributes to the problem of undertreatment.
The presence of opioid tolerance and physical dependence does not equate with "addiction."
Physical dependence on opioids is revealed when the opioid is abruptly discontinued or when naloxone is administered and is typically manifested as anxiety, irritability, chills and hot flashes, joint pain, lacrimation, rhinorrhea, diaphoresis, nausea, vomiting, and abdominal cramps and diarrhea. The mildest form of the opioid abstinence syndrome may be confused with viral "flu-like*" syndromes. For opioids with short half-lives (i.e., codeine, hydrocodone, morphine, hydromorphone), the onset of withdrawal symptoms can occur within 6 to 12 hours and peak at 24 to 72 hours after discontinuation. For opioids with long half-lives (i.e., methadone, levorphanol, transdermal fentanyl), the onset of the abstinence syndrome may be delayed for 24 hours or more after drug discontinuation and may be of milder intensity. The appearance of the abstinence syndrome defines physical dependence on opioids, which may occur after just 2 weeks of opioid therapy, but does not imply psychological dependence or addiction. Most patients with cancer take opioids for more than 2 weeks, and only very rarely do they exhibit the drug abuse behaviors and psychological dependence that characterize addiction (Portenoy and Payne,1992).
Patients with cancer occasionally require discontinuation or rapid decreases in doses of opioids when the cause of pain is effectively eliminated by antineoplastic treatments or pain perception is modified by neuroablative or neurolytic procedures. In such circumstances, the opioid abstinence syndrome can be avoided by withdrawal of the opioid on a schedule that provides half the prior daily dose for each of the first 2 days and then reduces the daily dose by 25 percent every 2 days thereafter until the total dose (in morphine equivalents) is 30 mg/day. The drug may be discontinued after 2 days on the 30 mg/day dose (American Pain Society, 1992). Transdermal clonidine (0.1 to 0.2 mg/day) may reduce anxiety, tachycardia, and other autonomic symptoms associated with opioid withdrawal.
Tolerance to opioids is defined as the need to increase dose requirements over time to maintain pain relief. For most cancer patients, the first indication of tolerance is a decrease in the duration of analgesia for a given dose. Increasing dose requirements are most consistently correlated with progressive disease, which produces increased pain intensity (Foley, 1985a). Patients with stable disease do not usually require increasing doses (Foley, 1993; Levy, 1989).
Opioid doses should be adjusted in each patient to achieve pain relief with an acceptable level of adverse effects. Dosage typically requires adjustment over time. With the exception of fentanyl delivered by the transdermal route, there is no ceiling or maximal recommended dose for full opioid agonists, and in fact, very large doses of morphine, e.g., several hundred milligrams every 4 hours, may be needed for severe pain (Foley, 1985a).
Effective pain relief can be accomplished by the anticipation and prevention of pain. Because many patients have persistent or daily pain, it is important to use opioids on a regular schedule rather than only "as needed." Around-the-clock administration of analgesics allows each dose to become effective before the previous dose has lost its effectiveness. A patient should be given "as-needed" doses for the first 24 to 48 hours when a new drug is started to define the best daily dosing requirements for that individual patient.
Table 10. Dose equivalents for opiod analgesics in opiod-naive adults and children > 50 kg body weight1
| Drug | Approximate equianalgesic dose | Usual starting dose for moderate to severe pain | ||
| Oral | Parenteral | Oral | Parenteral | |
| Opioid agonist2 | ||||
| Morphine3 | 30 mg q 3-4 h (repeat around-the-clock dosing) 60 mg q 3-4 h (single dose or intermittent dosing) | 10 mg q3-4h | 30 mg q 3-4 h | 10 mg q3-4h |
| Morphine, Controlled release3,4 (MS Contin, Oramorph) |
90-120 mg q 12 h | N/A | 90-120 mg q12h | N/A |
| Hydromorphone3 (Oilaudid) | 7.5 mg q 3-4 h | 1.5 mg q 3-4 h | 6 mg q 3-4 h | 1.5 mg q 3-4 h |
| Levorphanol (LevoDromoran) | 4 mg q 6-8 h | 2 mg q 6-8 h | 4 mg q 6-8 h | 2 mg q 6-8 h |
| Meperidine (Demerol) | 300 mg q 2-3h | 100 m g q 3 h | N/R | 100 m g q 3 h |
| Methadone (Dolophine, other) | 20 mg q 6-8 h | 10mgq6-8h | 20 mg q 6-8 h | 10mgq6-8h |
| Oxymorphone3 (Numorphan) | N/A | 1 mg q 3-4 h | N/A | 1 mg q 3-4 h |
| Combination opioid/NSAID preparations5 | ||||
| Codeine6 (with aspirin or acetaminophen) | 180-200 mg q 3-4h | 130 mg q3-4h | 60 mg q 3-4 h | 60 mg q 2 h (IM/SC) |
| Hydrocodone (in Lorcet, Lortab. Vicodin. others) | 30 mg q 3-4 h | N/A | 10 mg q 3-4 h | N/A |
| Oxycodone (Roxicodone. also in Percocet, Percodan, Tyiox, others) | 30 mg q 3-4 h | N/A | 10 mg q 3-4 h | N/A |
1Caution: Recommended doses do not apply for adult patients with body weight less than 50 kg. For recommended starting doses for children and adults < 50 kg body weight, see Table 11. 2Caution: Recommended doses do not apply to patients with renal or hepatic insufficiency or other conditions affecting drug metabolism and kinetics. 3Caution: For morphine, hydromorphone, and oxymorphone, rectal administration is an alternate route for patients unable to take oral medications. Equianalgesic doses may differ from oral and parenteral doses because of pharmacokinetic differences. 4Transdermal fentanyl (Duragesic) is an alternative option. Transdermal fentanyl dosage is not calculated as equianalgesic to a single morphine dose. See the package insert for dosing calculations. Doses above 25 µ-g/h should not be used in opiod-naive patients. 5caution: Doses of aspirin and acetaminophen in combination opioid/NSAID preparations must also be adjusted to the patient's body weight. Aspirin is contraindicated in children in the presence of fever or other viral disease because of its association with Reye's syndrome. 6Caution: Codeine doses above 65 mg often are not appropriate because of diminishing incremental analgesia with increasing doses but continually increasing nausea, constipation. and other side effects. Note: Published tables vary in the suggested doses that are equianalgesic to morphine. Clinical response is the criterion that must be applied for each patient: titration to clinical responses is necessary. Because there is not complete cross-tolerance among these drugs. it is usually necessary to use a lower than equianalgesic dose when changing drugs and to retitrate to response. Codes: q=every. N/A=not available. N/R=not recommended. IM=intramuscular. SC=subcutaneous. |
||||
In addition to the titration of individual drugs, the modalities for pain management are titrated when the pain is persistent and is moderate to severe in intensity (see Figure 3).
Pain management for moderate to severe pain should begin with oral opioids in combination with an NSAID or acetaminophen. The optimal dose will control pain with the fewest side effects, such as sedation, mental clouding, nausea, or constipation.
Adjuvant drugs (see below) may be used to counteract the predictable side effects of opioids. For example, hydroxyzine may be added to opioids and NSAIDs to manage anxiety and nausea, especially when they occur simultaneously and are not intense. Dietary caffeine supplementation may provide additive analgesia and counteract opioid induced sedation. Antiemetic drugs such as phenothiazines and metoclopramide may be added to manage opioid-induced nausea.
It is usually advisable to observe the patient's response to several different opioids, sequentially, before switching routes of administration or trying an anesthetic, neurosurgical, or other invasive approach to relieve persistent pain (Galer, Coyle, Pasternak, et al., 1992). For example, patients who experience dose-limiting sedation, nausea, or mental clouding on oral morphine should be switched to an equianalgesic dose of hydromorphone or fentanyl. The dose of the second opioid should then be adjusted. Sequential analgesic trials should be based on regular assessments of pain, with continuous attention to antineoplastic and noninvasive nonpharmacologic therapies (see Figure 1).
Table 11. Dose equivalent for opiod analgesics in opiod-naive children and adults < 50 kg body weight1
| Drug | Approximate equianalgesic dose | Usual starting dose for moderate to severe pain | ||
| Oral | Parenteral | Oral | Parenteral | |
| Opioid agonist2 | ||||
| Morphine3 | 30 mg q 3-4 h (repeat around-the-clock dosing) 60 mg q 3-4 h (single dose or intermittent dosing) | 10mg q3-4h | 0.3mg/kg q3-4h | 0.1 mg/kg q3-4h |
| Morphine controlled-release3,4 (MS Contin, Oramorph) | 90-120 mg q12h | N/A | N/A | N/A |
| Hydnomorphone3 (Dilaudid) | 7.5 mg q3-4h | 1.5 mg q3-4h | 0.06mg/kg q3-4h | 0.015 mg/kg q3-4h |
| Levorphanol (Levo-Dromoran) | 4mg q6-8h | 2mg q6-8h | 0.04mg/kg q6-8h | 0.02 mg/kg q6-8h |
| Meperidine (Demerol) | 300 mg q2-3h | 100 mg q3h | N/R | 0.75 mg/kg q2-3h |
| Methadone (Dotophine, others) | 20 mg q6-8h | 10mg q6-8h | 0.2 mg/kg q6-8h | 0.1 mg/kg q6-8h |
| Combination opioid/NSAID preparations5 | ||||
| Codeine6 (with aspirin or acetaminophen) | 180-200 mg q3-4h | 130mg q3-4h | 0.5-1 mg/kg q3-4h | N/R |
| Hydrocodone (in Lorcet, Lortab, Vicodin, others) | 30 mg q3-4h | N/A | 0.2 mg/kg q3-4h | N/A |
| Oxycodone (Roxicodone. also in Percocet. Percodan, Tytox. others) | 30 mg q3-4h | N/A | 0.2 mg/kg q3-4h | N/A |
| 1Caution: Doses listed for patients
with body weight less than 50 kg cannot be used as initial starting doses in
babies less than 6 months of age. 2Caution: Recommended doses do not apply to patients with renal or hepatic insufficiency or other conditions affecting drug metabolism and kinetics. 3Caution: For morphine, hydromorphone. and oxymorphone, rectal administration is an alternate route for patients unable to take oral medications. Equianalgesic doses may differ from oral and parenteral doses because of pharmacokinetic differences. 4Transdermal fentanyl (Duragesic) is an alternative option. Transdermal fentanyl dosage is not calculated as equianalgesic to a single morphine dosage. See the package insert for dosing |
||||
The speed of onset and duration of action for any opioid depend on the specific drug chosen and its formulation (tablet, elixir, etc.). Most are well absorbed after oral or rectal administration, yet absorption may not be complete. Further, drugs absorbed from the gut are subject to first-pass metabolism in the liver and, hence, should be given at higher doses than when given parenterally. Although dosage requirements for different parenteral routes (intravenous, subcutaneous, and intramuscular) are comparable or equivalent, the onset of drug action is typically most rapid after intravenous dosing because there is no delay in absorption. Therefore, drug dose and frequency should be titrated to the individual patients response and analgesic needs when changing the route of administration or the type of formulation.
Oral. The oral route is the preferred route of analgesic administration because it is the most convenient and cost-effective. Oral opioids are available in tablet, capsule, and liquid forms and in immediate and controlled-release formulations; morphine is available in immediate and controlled-release forms. Controlled-release tablets become immediately released when crushed and are therefore not appropriate for patients who are unable to swallow whole tablets. A small percentage may require alternate routes during their illness and when they are unable to swallow, such as during mucositis or in the terminal phase. Coyle, Adelhardt, Foley, et al. (1990) found that many patients required more than one route of administration to maintain pain control in the last 4 weeks of life. When patients cannot take medications orally, other less invasive routes such as rectal or transder-mal routes should be tried. During intravenous and subcutaneous administration, local irritation of the skin or vein may occur. Therefore, parenteral routes should be used only when simpler, less demanding, and less costly methods are inappropriate or ineffective.
Rectal. The rectal route may be used when patients have nausea or vomiting or are fasting either preoperatively or postoperatively. The rectal route is contraindicated if there are lesions of the anus or rectum because placement of the suppository will cause pain. This route is also not useful if there is diarrhea or in elderly or infirm patients who are physically unable to place the suppository.
There are commercially available suppositories of morphine, hydro-morphone, and oxymorphone. Medications can also be placed in a colostomy or similar stoma, provided that the flow of effluent is slow • enough to allow the drug to be absorbed via the mucosa (McCaffery, Martin, and Ferrell, 1992). When converting from the oral to the rectal route, start with the same amount as the oral dose and titrate as needed.
Transdermal. Transdermal administration bypasses GI absorption. Fentanyl is currently the only opioid commercially available in a trans-dermal form (TDS-Fentanyl). Four patch sizes are available and provide delivery of fentanyl at 25,50,75, or 100 u-g/hour; therefore, there is flexibility in drug dosing. The maximal recommended daily dose is 300 p.g/hour. Patients requiring larger doses should be switched to an equianalgesic dose of an oral or subcutaneously administered opioid.
Each patch contains a 72-hour supply of fentanyl, which is passively absorbed through the skin over this period. Levels in plasma rise slowly over 12 to 18 hours after patch placement, and the dosage form has an elimination half-life of 21 hours. Therefore, unlike intravenous fentanyl, the transdermal administration of fentanyl is not suitable for rapid dose titration (Payne, 1992: Portenoy, Southam, Gupta, et al., 1993). Transdermal fentanyl should be considered when patients already on opioid therapy have relatively constant pain and infrequent episodes of breakthrough pain such that rapid increases or decreases in pain intensity are not anticipated. As with other long acting analgesics, all patients should be provided with oral or parenteral rapidly acting short duration opioids to manage breakthrough pain (Portenoy and Hagen, 1990). The most commonly reported side effects of transdermal fentanyl administration are nausea, mental clouding, and skin irritation.
Nasal. The transnasal route is an alternative delivery method that may be useful when patients are no longer able to tolerate the oral route. Although several agents are currently being studied, the only commercially available formulation is the mixed agonist-antagonist drug butorphanol, which is rapidly taken up by the vascular nasal mucosa. The major indication for its use is acute headache. Although this formulation has general appeal by virtue of its potential for rapid action because it is a mixed agonist-antagonist, this drug is not recommended for routine use in cancer pain treatment.
Intravenous or Subcutaneous. Intramuscular administration of drugs should be avoided because this route can be painful and inconvenient, and absorption is not reliable. Intravenous or subcutaneous administration are effective alternatives. Patients who may benefit from continuous infusions of opioids include:
The benefits of opioid infusions, compared with those of intermittent "as-needed" doses by intramuscular or subcutaneous injection, include less pain on injection, fewer delays awaiting preparation and administration of medication, and improved effectiveness (Bruera, Brenneis, and MacDonald, 1987; Portenoy, 1986,1987). The intravenous route provides the most rapid onset of analgesia, but the duration of analgesia after a bolus dose is shorter than with other routes.
A continuous intravenous infusion provides the most consistent level of analgesia and is easily accomplished for patients who have permanent intravenous access for other purposes such as hydration, alimentation, chemotherapy, or antibiotic administration. If intravenous access is not available or desirable, continuous subcutaneous opioid infusion offers a practical alternative in the hospital and home. The subcutaneous administration of opioids provides levels in blood comparable to those with intravenous doses; therefore, the intravenous dose recommendations can be used (Tables 10 and 11) (Moulin, Kreeft, Murray-Parsons, et al., 1991).
Intraspinal. Analgesics may be administered intraspinally when pain cannot be controlled by oral, transdermal, subcutaneous, or intravenous routes because side effects such as confusion and nausea limit further dose escalation. Documentation of the failure of maximal doses of opioids and coanalgesics administered through other routes should precede consideration ofintraspinal analgesia. Furthermore, this route requires experience, meticulous technique, significant family and professional support systems, and sophisticated follow up, which are not available in all settings. Before implantation of a permanent device, screening should be conducted to ensure adequate response to spinal therapy. A trial of graded opioid doses administered percutaneously through an epidural catheter generally will indicate whether intraspinal therapy is warranted.
As with systemic opioid administration, the dose range for intraspinal opioid therapy varies widely, depending on the level of pain and tolerance (Du Pen and Williams, 1992). Any agent delivered •into the epidural or intrathecal space should be free of preservatives because some preservatives and antioxidants can produce neurotoxicity when used intraspinally (Du Pen, Ramsey, and Chin, 1987; Wang, Hillman, Spielholz, et al., 1984). All patients treated with intraspinal drugs should have access to rescue medications (oral or parenteral) for periods of breakthrough pain or in the case of catheter or drug delivery system malfunction. The coadministration of systemic opioids (which generally is not recommended for postoperative pain management) is safe in most cancer patients because they are tolerant to the respiratory-depressant effects of the drugs.
Morphine is the most commonly used intraspinal drug. Alternative opioids such as hydromorphone, fentanyl, or sufentanil have been used intraspinally to manage cancer pain and may be useful substitutes when the patient experiences side effects from morphine. Intraspinal morphine may produce the same side effects of nausea, mental clouding, and sedation as in oral, rectal, or parenteral dosing, because epidural or subarachnoid morphine is absorbed into the circulation by way of the rich epidural vascular plexus and is also carried in the normal flow of cerebrospinal fluid (CSF) from spinal levels to the brain (Bromage, Camporesi, Durant, et al., 1982; Chauvin, Samii, Schermann, et al., 1982; Cousins, 1988; Max, Inturrisi, Kaiko, et al., 1985). Single-dose epidural administration of 10 mg of morphine produces levels in blood comparable to an intramuscular injection of the same dose (Max, Inturrisi, Kaiko, et al., 1985). Very lipophilic opioids such as fentanyl and sufentanil have a more limited CSF distribution, but these drugs also gain access to the blood and are delivered to the brain via the systemic circulation.
In some patients, it is possible to give relatively small doses of opioid spinally and produce pain relief while avoiding the side effects that can limit prior oral or parenteral dosing. However, patients with a high degree of tolerance to systemic opioids may require large doses of spinal opioids (Cousins and Bridenbaugh, 1987), which may negate the advantages of this targeted approach because side effects may still be prominent at high dosage levels.
The main indication for the long-term administration of intraspinal opioids is intractable pain in the lower part of the body, particularly when pain is bilateral or midline (Du Pen and Williams, 1992). With proper selection and screening, good to excellent pain relief can be expected in up to 90 percent of patients (Krames, Gershow, Glassberg, et al., 1985; Onofrio and Yaksh, 1990). Opioids (sometimes coadministered with other agents such as dilute local anesthetic) (Akerman, Arwestrom, and Post, 1988; Fraser, Chapman, and Dickenson, 1992; Maves and Gebhart, 1992; Tejwani, Rattan, and McDonald, 1992) are delivered to the epidural or subarachnoid space via percutaneously placed catheters connected to ports, reservoirs, or infusion pumps (Table 12). For short-term treatment of weeks to a few months, externalized catheters (tunneled or untunneled) can be used. For more prolonged treatment, the delivery system (catheter plus port or pump) can be internalized. Adverse sequelae include the development of tolerance, urinary retention, constipation, pruritus, device failure, and infection (Du Pen, Peterson, Williams, et al., 1990; Hogan, Haddox, Abram, et al., 1991).
Intraventricular. Experience with intraventricular morphine administration is steadily increasing, and results with this route compare favorably with those with intraspinal administration, with over 90 percent of patients in published series benefitting significantly (Choi, Ha, Ahn, et al., 1989). Most important, intraventricular morphine is beneficial for recalcitrant pain due to head and neck malignancies and tumors (e.g., superior sulcus tumors, breast carcinoma) that affect the brachial plexus. Small maintenance doses of morphine (less than 5 mg daily) are needed to achieve maximal comfort. Complications are rare, the most important being infection; as with intraspinal drug delivery, tolerance and respiratory depression do not appear to be major issues (Acute Pain Management Guideline Panel, 1992). Intraventricular morphine requires the placement of a ventricular catheter connected to a subcutaneous (e.g., Ommaya) reservoir for intermittent administration or an infusion pump for continuous infusion (Lazorthes, Verdie, Bastide, et al., 1985; Obbens, Hill, Leavens, et al., 1987).
Patient-Controlled Analgesia (PCA). PCA allows patients to control the amount of analgesia they receive (Ferrante, Ostheimer, and Covino, 1990). PCA can be accomplished by mouth or by the use of a special pump set to prescribed parameters to administer the drug intravenously, subcutaneously, or epidurally. In contrast to the use of PCA in postoperative pain management, the majority of the opioid dose is usually delivered via continuous systemic infusion. Patient-administered boluses are required to treat breakthrough pain and to provide a basis for more accurate and rapid upward titration of the continuous infusion rate.
Intravenous or subcutaneous PCA allows patients to accommodate transient changes in analgesic requirements (such as during dressing changes or positioning) and to tailor analgesic doses according to their own requirements. PCA is also useful in controlling pain quickly in the patient admitted to the hospital specifically for analgesia, and in determining the opioid dosage requirements for conversion to an oral regimen once a steady level of satisfactory analgesia is attained (Baumann, Batenhorst, Graves, et al., 1986). Intravenous and subcutaneous PCA is safe for both home and hospitalized patients (Baumann, Batenhorst, Graves, et al., 1986; Citron, Johnston-Early, Boyer. et al., 1986; Kerr, Sone, Deangelis, et al., 1988; Swanson, Smith, Bulich, et al., 1989) but is contraindicated for sedated and confused patients (Ferrell, Cronin Nash, and Warfield, 1992).
Table 12. Intraspinal drug delivery systems
| System | Advantages | Disadvantages |
| Percutaneous temporary catheter | Used extensively both intraoperatively and postoperatively. Useful when prognosis is limited (< 1 month). | Mechanical problems include catheter dislodgment, kinking, or migration. |
| Permanent silicone-rubber epidural | Catheter implantation is a minor procedure. Dislodgment and infection less common than with temporary catheters. Can deliver bolus injections, continuous infusions, or PCA (with or without continuous delivery). | |
| Subcutaneous implanted injection port | Increased stability, less risk of dislodgment Can deliver bolus injections or continuous infusions (with or without PCA). | Implantation more invasive than external catheters. Approved only for epidural catheter in U.S. Potential for infection increases with frequent injections. |
| Subcutaneous reservoir | Potentially, reduced infection in comparison to external system. | Difficult to access, and fibrosis may occur after repeated injection. |
| Implanted pumps (continuous and programmable) | Potentially, decreased risk of infection. | Need for more extensive operative procedure. Need for specialized, costly equipment with programmable systems. |
Constipation and sedation are the most common side effects associated with opioids; others include confusion, nausea and vomiting, respiratory depression, dry mouth, urinary retention, pruritus, myoclonus, altered cognitive function, dysphoria, euphoria, sleep disturbances, sexual dysfunction, physiologic dependence, tolerance, and inappropriate secretion of antidiuretic hormone (Table 13). Because there is great individual variation in the development of opioid-induced side effects, clinicians should monitor for them and prophylactically treat some inevitable ones.
Constipation. Constipation is a common problem associated with opioid administration. Tolerance to the constipating effects of opioids either does not occur or occurs very slowly during chronic therapy. Constipation may worsen with time because of the disease process (e.g., intestinal obstruction, paralytic ileus due to spinal cord compression, decreased food and fluid intake due to anorexia); therefore a careful search for other causes should be performed (Glare and Lickiss, 1992). Mild constipation can usually be managed by an increase in fiber consumption and the use of a mild laxative such as milk of magnesia. These cathartic agents should be administered on a regular schedule, barring contraindications. Severe constipation occurs as a result of the inhibition of peristalsis by opioids and can be treated with a stimulating cathartic drug, e.g., bisacodyl, standardized senna concentrate, or hyperosmotic agents (e.g., lactulose or sorbitol). Oral laxatives can be taken at bedtime, and rectal suppositories can be used in the morning if needed.
Stool softeners or emollient laxatives, e.g., docusate, are of limited usefulness because of colonic resorption of water from the forming stool. They should not be used as the sole regimen but may be useful when given in combination with stimulant laxatives to ease defecation. especially in bedridden patients (Levy, 1991).
Sedation. Transitory sedation is common when opioid doses are increased substantially, but tolerance usually develops rapidly. Persistent drug-induced sedation is usually best treated by reducing the opioid in each dose and increasing the dosage frequency. This strategy will decrease the peak concentrations in blood (and brain) while maintaining the same total dose. In some patients, switching to another opioid may reduce the sedative effects. CNS stimulants such as caffeine, dextroamphetamine (2.5 to 7.5 mg twice daily, orally), pemoline (18.5 to 37 mg, orally), or methylphenidate (5 to 10 mg, orally) (Bruera, Brenneis, and Paterson, 1989) may be added to increase alertness if the above approach is ineffective in reducing sedation (Forrest, Brown, Brown, et al., 1977).
| Table 13. General comments and cautions regarding the use of opioid analgesics |
|
These agents also improve the cognitive function of patients receiving opioids, most likely by counteracting the sedation. In these patients, methylphenidate has been demonstrated to improve functioning on a number of neuropsychological tests, including tests of memory, mental speed, and concentration (Bruera, Miller, Macmillan, et al., 1992).
Nausea and Vomiting. There are no controlled studies that establish the indications, efficacy, and dosing requirements for treatment of opioidinduced nausea and vomiting. As with other side effects, it is important to determine the cause. Clinical experience suggests that opioidinduced nausea and vomiting can be managed with antiemetics chosen according to their modes of action. Metoclopramide is helpful when neuroleptics such as prochlorperazine, chlorpromazine, or haloperidol fail to control nausea and vomiting. Scopolamine or hydroxyzine may ameliorate symptoms as a result of their effects on the vestibular system. Scopolamine, which is an acetylcholine receptor antagonist, can be given transdermally to reduce nausea due to motion sickness (Ferris, Kerr, Sone, et al., 1991) or related to cancer. When patients complain of nausea after opioid administration has begun, it is often helpful to administer an antiemetic on a fixed schedule for several days, after which as-needed dosing is usually adequate (Portenoy, 1988). Depending on the antiemetic chosen, patients should be monitored for the possibility of increased sedation.
Respiratory Depression. Patients receiving long-term opioid therapy usually develop tolerance to the respiratory-depressant effects of these agents. Occasionally, respiratory depression occurs when pain is abruptly relieved and the sedative effects of opioids are no longer opposed by the stimulating effects of pain (Hanks, Twycross, and Lloyd, 1981). In a symptomatic patient, physical stimulation may be enough to prevent significant hypoventilation. Opioid antagonists (e.g., naloxone) should be given cautiously to patients who are receiving opioids on a long-term basis. Because patients who have become tolerant to opioids show great sensitivity to the effects of antagonist drugs, symptomatic respiratory depression should be treated carefully using a dilute solution of naloxone (0.4 mg in 10 mL of saline), administered as 0.5 mL (0.02 mg) boluses every minute. The dose of naloxone should be titrated to the patient's respiratory rate. A return to full alertness is often accompanied by a severe withdrawal syndrome and a return of pain. Naloxone titration, when indicated for the reversal of opioid-induced respiratory depression, should be given incrementally in doses that improve respiratory function but do not reverse analge-sia. Repeated doses may be required (American Pain Society, 1992; Portenoy, 1988), or alternatively, an infusion of two ampules (total, 0.8 mg) in 250 mL of 5 percent dextrose in water may be continuously titrated toward this goal.
Far more common than acute respiratory depression is subacute overdose, in which sedation gradually builds and is followed by a slowing of respiratory rate and then by ventilatory failure. The degree of sedation rather than the respiratory rate is a better indicator of impending respiratory depression (Kaiko, Kanner, Foley, et al., 1987). The risk of this complication is highest during titration of opioids with long plasma half-lives, such as methadone and levorphanol, and is best managed by withholding one or two doses and then reducing the standing dose by 25 percent of its current level until symptoms have resolved. At that time, a cautious titration can be resumed. The maintenance of 25 percent of the dose has been found to be adequate to prevent acute opioid withdrawal (American Pain Society, 1992).
Clinicians are often concerned that high doses of opioids used for palliation may harm or kill a patient, particularly when doses are further increased to alleviate pain (Cain and Hammes, in press). This double effect of intended benefit and potential harm (Reich, 1992) is seen in the clinical situation when the intended treatment may have inextricably linked deleterious side effects. The administration of medication is always a riskversusbenefit calculation. When the patient's death is imminent because of the progression of primary disease, an increased risk of earlier death counts little against the benefit of pain relief and painless death. The ethical duty to benefit the patient through relieving pain is by itself adequate to support increasing doses to alleviate pain, even if there might be life-shortening and expected side effects. Because many patients in the terminal phase have been receiving opioid pain medications for a significant period of time, the fear of shortening life by medication is usually unfounded. Respiratory depression is not often a significant limiting factor in pain management'because, with repeated doses, tolerance develops to this effect, allowing for adequate pain treatment with escalating doses without respiratory compromise (Foley, 1991). The person dying from cancer should not be allowed to live out life with unrelieved pain because of fear of side effects; rather, appropriate, aggressive palliative support should be given (see Shapiro, in press, b; Cain and Hammes, in press).
Other Side Effects. Opioids occasionally cause myoclonus, seizures, hallucinations (Bruera, Schoeller, and Montejo, 1992), confusion, sexual dysfunction, sleep disturbances, and pruritus (Thangathu-rai. Bowks, Alien, et al., 1988). Prolonged use is known to affect sexual function and libido in both men and women. Women experience amenorrhea and infertility, whereas men report an inability to attain or maintain an erection. Changes in serum testosterone and other sex hormones have been described and may be responsible for some of these effects (Abel, F984).
Urinary retention may also occur, especially with spinal opioids (Cousins and Mather, 1984; Dray, 1988; Moulin, Kreeft, Murray-Parsons, et al., 1991; Rawal, Mollefors, Axelsson, et al., 1983), in men with prostatism, or in patients with pelvic tumors and bladder outlet obstruction. The management of urinary retention may include discontinuing adjuvant drugs with potentiating effects (e.g., tricyclic antidepressants) or changing to another opioid analgesic or route of administration. Diphenhydramine, an antihistamine, may reduce pruritus in some patients. The syndrome of the inappropriate secretion of antidiuretic hormone is a rare, often transitory, adverse effect of opioid drugs, most commonly reported with morphine and methadone; more often, it is a paraneoplastic complication.
Adjuvant drugs are used to enhance the analgesic efficacy of opioids, treat concurrent symptoms that exacerbate pain, and provide independent analgesia for specific types of pain. They may be used in all stages of the analgesic ladder. Commonly used agents are described below, with approximate daily dosage ranges listed in Table 14.
Corticosteroids provide a range of effects including mood elevation, anti-inflammatory activity, antiemetic activity, and appetite stimulation. These effects may be beneficial in the management of cachexia and anorexia in terminal illness (Bruera, Roca, Cedaro, et al., 1985). They also reduce cerebral and spinal cord edema and are essential in the emergency management of elevated intracranial pressure and epidural spinal cord compression. Steroids are part of the standard therapy for tumor-induced spinal cord compression (By me, 1992), and they are effective in reducing pain due to perineural edema and pressure on nerves. Dexamethasone (16 to 24 mg/day) or pred-nisone (40 to 100 mg/day) may be added to opioids for the management of pain in brachial or lumbosacral plexopathy. Undesirable effects such as myopathy, hyperglycemia, weight gain, and dysphoria may occur during prolonged steroid therapy.
Anticonvulsants are used to manage neuropathic pain, especially when the pain is lancinating or burning. Phenytoin, carbamazepine. valproate, and clonazepam suppress spontaneous neuronal firing and are used to control lancinating pain complicating nerve injury (Swcrd-low, 1984). Dose-related transient bone marrow suppression, which is associated with carbamazepine therapy (Horowitz, Patwardhan, and Marcus, 1988; Pellock, 1987), requires that it be used with caution in cancer patients undergoing other marrow-suppressant therapies, such as chemotherapy and radiation therapy. Toxicity often correlates with high concentrations in serum, and levels in serum of phenytoin, valproate, and carbamazepine should be monitored routinely (for example, monthly in the stable patient). Systemically administered local anesthetic (intravenous lidocaine, oral mexilitine, and tocainide) and antiarrhythmic agents have been used clinically to treat neuro-pathic pain (Brose and Cousins, 1991; Dejgard, Petersen, and Kastrup, 1988), although this is not currently an FDA-approved indication for these drugs.
Table 14. Adjuvant analgesic drugs for cancer pain
| Drug | Approximate adult daily dose range | Route of administration1 | Type of pain |
| Corticosteroids | |||
| Dexamethasone2 | 16-96 mg | PO.IV | Pain associated with brain metastases and epidural spinal cord compression |
| Prednisone | 40-100 mg | PO | |
| Anticonvulsants | |||
| Carbamazepine3 | 200-1.600 mg | PO | Neuropathic pain |
| Phenytoin4 | 300-500 mg | PO | |
| Antidepressants | |||
| Amitriptytine5 | 25-15 mg | PO | Neuropathic pain |
| Doxepin6 | 25-150 mg | PO | |
| Imipramine7 | 20-100 mg | PO | |
| Trazodone8 | 75-225 mg | PO | |
| Neuroleptics | |||
| Methotrimeprazine9 | 40-80 mg | IM | Analgesia; sedation; antiemetic |
| Antihistamines | |||
| Hydroxyzine10 | 300-450 mg | IM | Adjuvant to opioids in post-operative and other types of pain; relief of complicating symptoms including anxiety, insomnia, nausea |
| Local anesthestics/antiarrythmics | |||
| Udocaine11 | 5mg/kg | IV/SC | Neuropathic pain |
| Mexiletine12 | 450-600 mg | PO | |
| Tocainide13 | 20mg/kg | PO | |
| Psychostimulants | |||
| Dextroamphetamine14 | Dextroamphetamine14 5-1 Omg | PO | Improve opioid analgesia, decrease sedation |
| Methylphenidate15 | 10-15 mg | PO | |
| 1PO=orally.
IV=intravenously. IM=intramuscularly. SC=subcutaneously. 2French and Galicich, 1964; Greenberg. Kirn, and Posner, 1980; Weissman. 1988. 3Undstrom and Undblom, 1987. 4 Yajnik, Singh, Singh. et al., 1992. 5 Max. Culnane, Schafer, et al., 1987; Max, Schafer. Culnane, et al.. 1988; Onghena and Van Houdenhove, 1992; Turkington, 1980: Ventafridda, Bonezzi, Caraceni, et al., 1987; Watson and Evans, 1985; Watson, Evans, Reed, et al., 1982; Young and Clarke, 1985. 6Cohn, Machado, Bier. et al.. 1988. 7Kvinesdal. Molin, Froland, et al., 1984; Turkington, 1980; Young and Clarke, 1985. 8Khurana, 1983; Ventafridda, Bonezzi, Caraceni, et al., 1987. 9Beaver, Wallenstein, Houde, et al., 1966; Rogers. 1989. 10Beaver and Feise, 1976; Bellville, Dorey, Capparell, et al., 1979; Glazier, 1990. 11Bach, Jensen, Kastrup, et al., 1990; Cousins and Brose, 1991. 12Dejgard, Petersen, and Kastrup, 1989. 13Lindstrom and Undblom, 1987. 14Josni. deJongh, Schnapper. et al.. 1982. 15Bruera, Chadwick, Brenneis, et al., .1987 |
|||
Tricyclic antidepressants are useful as adjuvant analgesics in the pharmacologic management of cancer pain, especially neuropathic pain. These drugs potentiate the analgesic effects of opioids in animal models of pain (Botney and Fields, 1983; Spiegel, Kalb, and Pasternak, 1983) and have innate analgesic properties (Kishore-Kumar, Max, Schafer, et al., 1990; Max, Culnane, Schafer, et al., 1987). They are effective through mechanisms that include: (1) mood elevation (France, 1987), (2) potentiation or enhancement of opioid analgesia (Ventafridda, Bianchi, Ripamonti, et al., 1990), and (3) direct analgesic effects (Max, Schafer, Culnane, et al., 1988).
The most widely reported experience has been with amitriptyline; therefore, it should be viewed as the tricyclic agent of choice, even though it produces anticholinergic side effects such as dry mouth, constipation, and urinary retention in many patients. Analgesic treatment failure may be due to low levels in serum (Max, Culnane, Schafer, et al., 1987; Max, Schafer, Culnane, et al., 1988). Doses of amitriptyline of up to 150 mg daily or higher may be required to obtain therapeutic effects (Kvinesdsal, Molin, Froland, et al., 1984; Watson and Evans, 1985). In the treatment of diabetic neuropathy pain, the therapeutic analgesic effects of amitriptyline appear to be correlated with concentrations in serum above 100 ng/mL. However, a corresponding relationship between amitriptyline concentrations in serum and analgesia has not been reported in cancer pain.
The onset of analgesic effects occurs within 1 to 2 weeks after the start of therapy and peaks at 4 to 6 weeks (Max, Culnane, Schafer, et al., 1987; Max, Schafer, Culnane, et al., 1988; Pilowsky, Hallett, Bassett, et al., 1982). Treatment should be initiated with a small dose of amitriptyline (10 to 25 mg at bedtime), especially in debilitated patients, and increased slowly by 10 to 25 mg every 2 to 4 days toward 150 mg. This approach takes advantage of the sedative effects of the drug and minimizes the risk of falling (especially in elderly patients) because of orthostatic hypotension. Amitriptyline is also useful when sleep disturbance complicates the presence of pain and depression, because its initial use is commonly associated with sedation.
Neuroleptics,which include the major tranquilizers generally used to treat psychoses and other psychiatric disorders, have also been used as adjunctive analgesics. Methotrimeprazine is a phenothiazine that has analgesic properties. Intramuscular doses of 15 mg methotri-meprazine and 10 mg of morphine are equianalgesic (Lasagna and De Kornfeld, 1961). This phenothiazine analgesic lacks opioid-inhibitory effects on gut motility and probably produces analgesia through a-adrenergic blockade (Beaver, Wallenstein, Houde, et al., 1966). In patients who are opioid tolerant or who are experiencing dose-limiting opioid side effects, especially intractable constipation, it is an alternative analgesic approach. It also has antiemetic and anxiolytic effects.
Methotrimeprazine can produce sedation and hypotension and should be given cautiously. Although it is approved only for intramuscular administration, clinicians have experience with oral and slow intravenous infusion to manage delirium, restlessness, and agitation in patients near death. Other phenothiazines have not been demonstrated to have analgesic properties (Maltbie, Cavenar, Sullivan, et al., 1979).
Hydroxyzine is a mild anxiolytic agent with sedating and analgesic properties that is used in treating the anxious patient with pain (Beaver and Feise, 1976). This antihistamine also has antiemetic activity.
Severe bone pain is a frequent complication of bone metastases. For example, Galasko (1972) reported that 65 percent of patients with hone metastases from breast cancer experience bone pain. Bone pain is probably caused by osteoclast-induced bone resorption by the tumor, which may also result in osteoporosis, hypercalcemia, microfractures. or pathologic fractures (Ascari, Attardo-Pamnello, and Merlini, 1989). Bisphosphonates (e.g., etidronate, pamidronate) are analogues of endogenous pyrophosphates, which inhibit bone resorption in vivo (Fleish, Russel, and Francis, 1969). Pamidronate and etidronate are currently available for the management of hypercalcemia associated with malignancy. Anecdotal reports and early clinical trials have reported relief of bone pain or decreased analgesic use after the initiation of a bisphosphonate (Delmas, Charhon, Chapuy, et al., 1982; Elomaa, Blomqvist, Grohn, et al., 1983). Other researchers have described similar findings with bisphosphonates that are not available in the United States (Attardo-Parrinello, Merlini, Pavesi, et al., 1987; van Holten-Verzantvoort, Zwinderman, Aaronson, et al., 1991). Smith (1989), however, reported no difference in symptomatic relief or analgesic requirements in 57 patients with advanced hormone-refractory prostate cancer treated with etidronate or placebo.
Calcitonin is also a potent inhibitor of osteoclast-induced bone resorption and, like the bisphosphonates, is used in the management of hypercalcemia of malignancy. At least one double-blind, randomized trial comparing salmon calcitonin to placebo demonstrated that 100 lU/day subcutaneously resulted in reduced analgesic consumption, shorter duration of pain, and subjective improvement (Roth and Kolaric, 1986).
Although these agents that inhibit bone resorption appear to be beneficial in some patients with painful bone metastases, other patients have failed to respond. Additional studies are warranted to define criteria that may predict a clinical response to these drugs and to define further their optimal use in this setting.
A mention of the placebo response is important to highlight the potentially harmful misunderstanding surrounding this phenomenon. The placebo response is common, and placebo-derived analgesia may be mediated to a great extent through endogenous opioid pathways. The deceptive use of placebo response to distinguish psychogenic pain from "real" pain should be avoided. Placebos are effective in a portion of patients for a short period of time only and should not be used in the management of cancer pain (American Pain Society, 1992; Foley, 1985a; World Health Organization, 1990).
Antineoplastic treatments for cancer include chemotherapy, hormonal and biologic therapies, and radiotherapy. Chemotherapy and hormonal therapies are generally used to treat all sites of cancer throughout the body and are not used specifically to treat pain. However, when the cause of cancer pain is direct tumor involvement, antineoplastic treatments may produce analgesia if they cause significant tumor shrinkage.
The major goal of antineoplastic treatment is either to cure by complete elimination of the cancer or, in situations in which cure is not possible, to prolong life and to achieve palliation of the tumor symptoms. Most important, the patient and clinician should discuss openly and thoroughly the expected goals and potential side effects of these therapies.
The presence of other medical conditions in cancer patients and the medications taken for them may influence the choice of analgesic regimen for pain management. Common medications or classes of meditation that produce clinically significant drug interactions with opioid analgesics include alcohol (as in elixirs) and other CNS depressants such as phenytoin, as well as rifampin (Kreek, Garfield, Gutjahr, et al., 1976) and monoamine oxidase inhibitors such as phenylzine sulfate and isocarboxazid (Breitbart and Holland, 1988).
Coexisting conditions also may influence the type and doses of opioid analgesics administered. For example, patients with newly recognized cancer pain who have been recently treated with opioids for another reason, such as surgery, may require higher than the recommended starting doses because they are opioid tolerant. Coagulopathy, neutropenia, and sepsis may contraindicate the use of epidural catheters or other regional anesthetic techniques because the risks of bleeding or "seeding" of infection are increased.
Many patients with cancer undergo surgery as part of their treatment. GI procedures such as gastrectomy and colectomy may markedly affect drug absorption and increase GI intolerance to some oral drugs. Drug pharmacokinetics can change after surgery because of changes in drug absorption and distribution caused by alterations in body weight, cardiac output, venous capacitance, extravascular fluid shifts, and protein binding. Fever and sepsis in the postoperative period can affect drug disposition, as do shock or trauma. Patients with such conditions may require higher than expected doses of opioids because of severe acute pain. In addition, they may not achieve clinically effective concentrations of opioids in plasma after intramuscular and subcutaneous injections because of the pharmacokinetic alterations described above.
Cancer often occurs in the elderly, who usually have decreased renal function as a normal result of aging. Mild age-related renal insufficiency (decline in glomerular filtration rate) can impede the excretion of the biologically active metabolites of many opioids, resulting in clinically significant sedation and respiratory depression (Sear, Hand, Moore, et al., 1989), as well as nausea (Hagen, Foley, Cerbone, et al., 1991). Meperidine, methadone, levorphano, pentazocine, and propoxyphene have increased bioavailability, prolonged half-lives, and decreased systemic clearance and thus accumulate in patients with hepatic or renal dysfunction. Renal excretion is a major route of elimination not only for opioids but also for their phannacologically active metabolites norpropoxyphene, normeperidine, morphine-6-glucuronide, and dihydrocodeine. Hence, in patients with renal dysfunction, doses of the parent compounds should be lowered or given less frequently.
A number of drugs and routes of administration are not recommended for the relief of cancer pain. These arc summarized in Table 15.
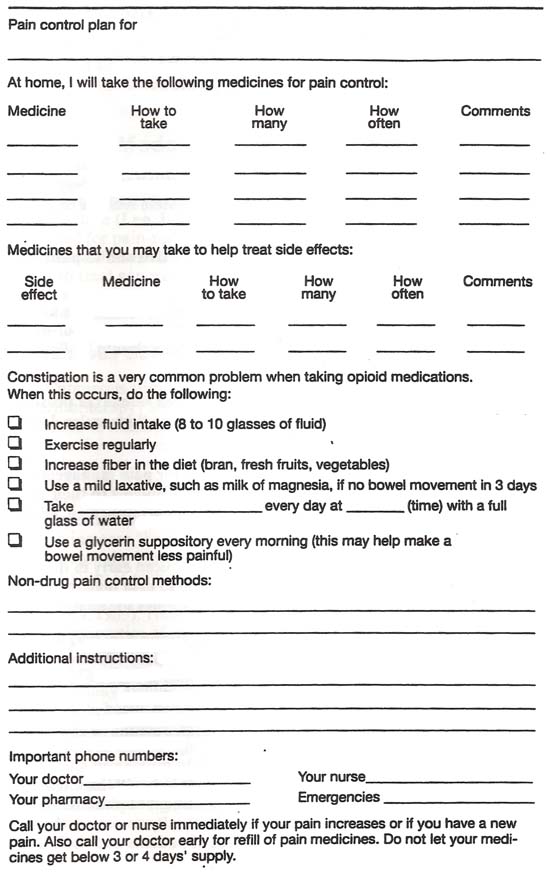
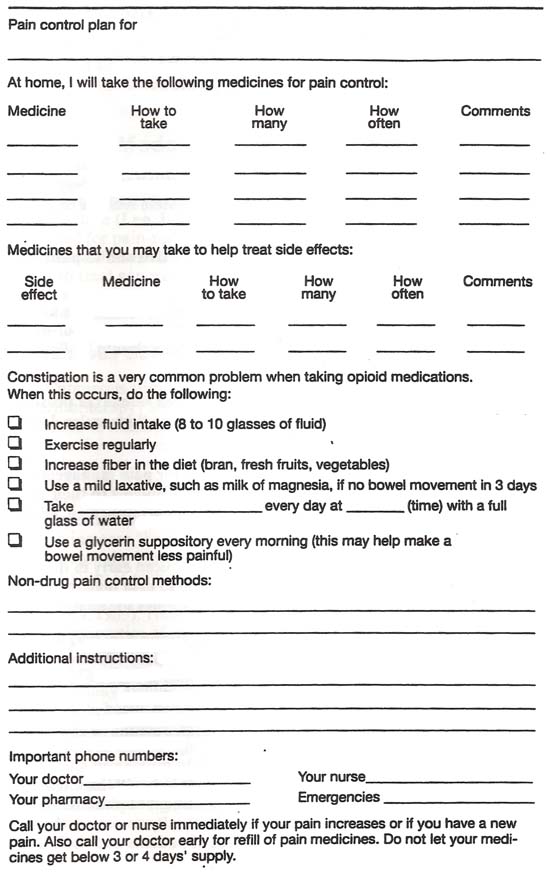
Patients and their families may have difficulty in understanding and remembering the details of the plan for managing pain. Therefore, patients should be given a written pain management plan (Figure 5, see page 74). Pertinent instructions related to the management of pain include the specific drugs to be taken; the type and purpose of pain medication (e.g., opioid, tricyclic antidepressant, anxiolytic); the frequency of drug administration, with an emphasis in most cases on taking the medication around the clock rather than as needed; potential side effects of each pain medication (particularly constipation for opioids) and a plan for their prevention or treatment; potential drug interactions; specific precautions to follow when taking a pain medication, such as physical activity limitations and dietary restrictions; and whom to notify about pain problems or concerns about the medication.
The plan should be reviewed with the patient, and the patient and/or caregiver should be given an opportunity to discuss fears or concerns about the use of opioid analgesics; to clarify issues related to tolerance, dependence, and addiction; to voice concerns about side effects; and to discuss when it is appropriate to communicate with a clinician regarding the need for a change in the plan.
| Table 15. Drugs and routes of administration not recommended for treatment of cancer pain | ||
| Class | Drug | Rationale for not recommending |
| Opioids | Meperidine | Short (2-3 hour) duration. Repeated administration may lead to CNS toxicity (tremor, confusion, or seizures) (Cleeland, 1985; Kaiko, Foley, Grabinski, et al., 1983; Szeto, Intumsi, Houde, et al., 1977). High oral doses required to relieve severe pain, and these increase the risk of CNS toxicity (American Pain Society, 1992; Weissman, Burchman, Dinndorf, etal., 1992). |
| Miscellaneous | Cannabinoids | Side effects of dysphoria. drowsiness, hypoten-sion, and bradycardia preclude its routine use as an analgesic (American Pain Society, 1992). |
| Cocaine | Has demonstrated no efficacy as an analgesic or coanalgesic in combination with opioids (American Pain Society, 1992). | |
| Opioid agonistantagonists | Pentazocine Butorphanol Nalbuphine | Risk of precipitating withdrawal in opioid-dependent patients. Analgesic celling (Kallos and Caruso. 1979; Nagashima, Karamanian, Malovany, et al., 1976). Possible production of unpleasant psychomimetic effects (e.g., dysphoria, hallucinations) (American Pain Society, 1992; Martin, 1984; Weissman, Burchman, Dinndorf, et al., 1992). |
| Partial agonist | Buprenorphine | Analgesic ceiling. Can precipitate withdrawal (American Pain Society, 1992; Weissman, Burchman, Dinndorf, et al., 1992). |
| Antagonist | Naloxone Naltrexone | May precipitate withdrawal. Limit use to treatment of life-threatening respiratory depression (Ellison.1993). |
| Combination preparations | Brompton's cocktail | No evidence of analgesic benefit to using Brompton's cocktail over single opioid analgesics (Twycross, 1977; Walsh, 1984: Weiss-man, Burchman, Dinndorf, et al., 1992; Wisconsin Cancer Pain Initiative, 1988). |
| DPT (Meperidine, Promethazine, and Chlorpromazine) | Efficacy is poor compared with that of other analgesics. High incidence of adverse effects (Nahata. Clotz, and Krogg, 1985). | |
| Anxiolytics alone | Benzodiazepine (e.g., alprazolam) |
Analgesic properties not demonstrated except for some instances of neuropathic pain. Added sedation from anxiotytics may limit opioid dosing (American Pain Society, 1992; Weissman. Burchman, Dinndorf, et al., 1992). |
| Sedative/ hypnotic drugs alone | Barbiturates Benzodiazepine | Analgesic properties not demonstrated. Added sedation from sedative/hypnotic drugs limits opioid dosing (American Pain Society, 1992). |
| Routes of administration Rationale for not recommending | ||
| Intramuscular (IM) | Painful. Absorption unreliable (American Pain Society, 1992). Should not be used for children or patients prone to develop dependent edema or in patients with thrombocytopenia (Weissman, Burchman, Dinndorf, et al., 1992). | |
| Transnasal | The only drug approved by the PDA for transnasal administration at this time is butor-phanol, an agonist-antagonist drug, which generally is not recommended. (See opioid agonist-antagonists above.) | |
Discharge planners should advise patients and clinicians to communicate the plan to other clinicians when the patient is being transferred from one health care setting to another, such as being discharged from an acute care facility to a hospice, in order to maintain continuity in pain management. Attachment B contains examples of forms that patients can use at home to document their pain.
Figure 5. Pain Management Plan