
By Leslie Shimp, Pharm.D., M.S.
Associate Professor of Pharmacy,
College of Pharmacy, University of Michigan
Consultant pharmacist, Department of Family Practice, Medical School,
University of Michigan
| Contents | Previous | Next |
 |
By Leslie Shimp, Pharm.D., M.S. |
Yeast infection (Candida vulvovaginids) is a common vaginal infection affecting significant numbers of women during their childbearing years. At least 75% of women experience one or more Candida vaginal infections during their childbearing years, and 20-25% of all visits to physicians' offices for vaginiris are for Candida vulvovaginitis.1,2 The availability of non prescription, over-the-counter (OTC) products for the treatment of Candida vaginitis is changing the way these conditions are managed (see Table 1).
| Table 1: Nonprescription Drugs for the Treatment of Candida Vulvovaginitis | ||
|---|---|---|
| Vaginal antifungal drugs | Recommended Regimen | |
| Clotrimazole (Gyne-Lotrimin™, Mycelex-7™, others) | ||
| 100 mg vaginal tab | 1 tab at bedtime for 7 days | |
| 1 % vaginal cream | 1 applicatorful at bedtime for 7 days | |
| 100 mg vaginal tab plus 1 % vaginal cream | 1 tab at bedtime for 7 days; apply topical cream to affected area twice daily (morning and evening) for 7 days | |
| 200 mg vaginal tab | 1 tab at bedtime for 3 days | |
| 200 mg vaginal tab plus 1 % vaginal cream | 1 tab at bedtime for 3 days; apply topical cream to affected area twice daily (morning and evening) for 3 days | |
| Miconazole (Monistat-7™, others) | ||
| 100 mg vaginal suppository (supp) | 1 supp at bedtime for 7 days | |
| 2% vaginal cream | 1 applicatorful at bedtime for 7 days | |
| 100 mg vaginal supp plus 2% vaginal cream | 1 supp at bedtime for 7 days; apply topical cream to affected area twice daily (morning and evening) for 7 days | |
| 200 mg vaginal supp | 1 supp at bedtime for 3 days | |
| 200 mg vaginal supp plus 2% vaginal cream | 1 supp at bedtime for 3 days; apply topical cream to affected area twice daily (morning and evening) for 3 days | |
| Butoconazole (Femstat-3™) | ||
| 2% vaginal cream | 1 applicatorful at bedtime for 3 days | |
| Ticonazole (Vagistat-1™) | ||
| 6.5% vaginal ointment | 1 applicatorful at bedtime one time | |
Despite the availability of effective therapy, many women with Candida vaginitis remain inadequately treated. It has been suggested that chronic or recurrent Candida infections are often due to noncompliance. A common barrier to compliance is lack of knowledge about the disease, available treatments, and the proper use of vaginal antifungal products.3 This article reviews the symptoms of Candida vulvovaginitis, describes who should—and who should not—self-treat, and outlines the appropriate use of OTC vaginal antifungals.
Candida vulvovaginitis, commonly referred to as a yeast infection, is caused by the Candida fungi. These organisms are normally present in low numbers within the gastrointestmal tract or vagina of asymptomatic women, but infections occur when Candida proliferates and invades vaginal tissue. About 85% of infections are caused by Candida albicans; the remainder are primarily caused by Candida tropicalis and Candida glabrata. The incidence of infections caused by C. tropicalis and C. glabrata has increased over the last two decades, and these species are more likely than C. albicans to be resistant to vaginal antifungal dierapy.4
A number of risk factors for Candida vaginitis have been studied.1, 5, 6 Considerable controversy exists concerning the role of most of these factors in the development of Candida infection (see Table 2).
| Table 2: Possible Risk Factors for Candida Vulvovaginitis 5,9,10 | |
|---|---|
| Broad-spectrum antibiotics | Not all women are affected: there may be a subgroup of patients who develop increased vaginal Candida. |
| Estrogen-containing oral contraceptives | Recent studies do not show an increased risk with low-dose (30-35 mcg) contraceptives. |
| Corticosteroids, Antineoplastics, Immunosuppressants | Can decrease host immune defenses and allow Candida to proliferate. |
| Pregnancy | Studies are inconclusive; some women may be affected. |
| Diabetes mellitus | Risk is increased, particularly with poor control of blood glucose. |
| Immunocornpromised patients | Increased risk in organ transplant recipients and HIV/AIDS patients. |
| Diet | Risk may increase with foods that elevate urinary sugar (e.g., milk, yogurt, cottage cheese). Conversely, daily consumption of active culture yogurt may protect against infection by controlling quantity of Candida in the body5 |
| Tight clothing/ pantyhose | While often implicated, studies do not support an increased risk. |
| Frequency of sexual intercourse | May facilitate entry of Candida to vagina and may cause minor vaginal trauma, increasing risk. |
| Sexual partners | There is no evidence that treatment of male partners prevents recurrence of vaginal Candida infections in women. |
Characteristic symptoms of Candida vulvovaginitis include intense vulvar or vaginal itching, a thick, sometimes clumpy, whitish (cottage cheese-like) vaginal discharge, and vulvar erythema and/or irritation.7 Most women experience itching or irritation, but only about 50% have the characteristic vaginal discharge. Other symptoms such as urinary frequency and external burning with urination are uncommon.8 The feature that best distinguishes Candida vulvovaginitis from other vaginal infections, such as bacterial vaginosis or trichomonas vaginitis, is the absence of an offensive odor from the vaginal discharge.
Self-treatment with a nonprescription antifungal product is most appropriate when: 1) a patient believes she may have Candida vulvovaginitis based upon the similarity of current symptoms to those experienced during a previous clinician-diagnosed infection, 2) current symptoms are consistent with the characteristic symptoms of mild/moderate Candida vulvovaginitis, particularly the absence of a foul-smelling vaginal discharge and significant urinary symptoms, and 3) vaginal symptoms are infrequent; no more than three candidal vaginal infections per year and none within the previous two months (see Table 3).
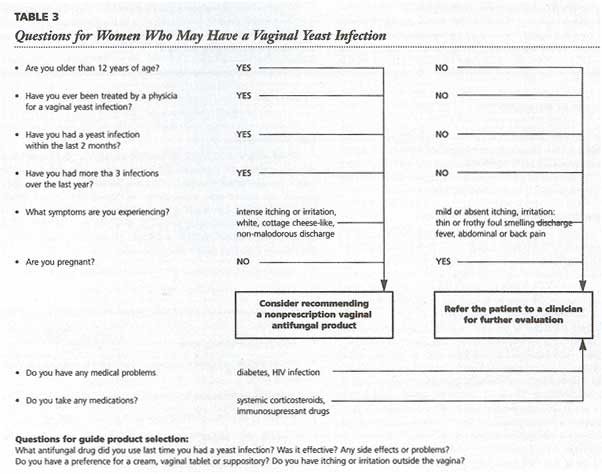
A small number of women, about 5 % of the population, have chronic, recurrent infections. Recurrent Candida vulvovaginitis is indicated by a return of symptoms within two months after treatment of a candidal vaginal infection, or four or more infections within 12 months.9 Women who experience recurrent symptoms require further evaluation and should not self-treat. Chronic vaginal symptoms may indicate the presence of an undiagnosed medical condition (e.g., diabetes mellitus, HIV infection) or a resistant infection (a mixed infection or non-albicans strain of candida.). Other patients who should not self-diagnose or self-treat include pregnant women, girls under the age of 12 years, patients with concurrent symptoms such as fever or abdominal pain, patients taking immunosuppressant drugs, and those with medical conditions (e.g., diabetes mellitus, HIV infection) which might predispose them to Candida infections.
There are currently four nonprescription imidazole vaginal antifungal drugs on the market: butoconazole, clotrimazole, miconazole, and tiocona-zole. Topical imidazole antifungals are the recommended initial therapy for Candida vulvovaginitis. All of the prescription and nonprescriprion imidazole products are very effective and are regarded as equally effective, with clinical cure rates in the range of 85-90%. 7
Therapy with vaginal antifungals involves once a day application, usually at bedtime. The duration of therapy varies; tioconazole offers one-day therapy, butoconazole has a three-day regimen, while clotrimazole and miconazole have both a three-day and a seven-day regimen. These regimens are equally effective for women with uncomplicated infections. While nonprescriprion products are available as suppositories, creams, or vaginal tablets, there is no evidence that one formulation is more effective than another.10 Patient preference often determines which type of product is used. A cream or the combined use of a cream and a vaginal suppository or tablet is recommended for women with vulvar symptoms so the antifungal can be applied both externally and vaginally (see Table 1 for dosage regimens).
The imidazoles have several effects which damage fungal cells. They inhibit the synthesis of essential fungal sterols, resulting in structural damage to the cell membrane and loss of membrane function. Imidazoles also inhibit enzyme activity, causing toxic concentrations of hydrogen peroxide to accumulate. This leads to deterioration of cell organelles and cell necrosis and inhibits the transformation of fungal cells into an invasive form.11
Topically applied imidazoles are absorbed to a limited extent (1-10%),2, 11, 12 and side effects are minimal. About 7% of patients experience some local burning, itching, or irritation, usually with the first dose of the vaginal preparation.11, 14 Local side effects may be more common with tioconazole. Headache, abdominal cramps, urinary frequency, abnormal sensations (e.g., burning, tingling), runny nose, fever and chills, and penile irritation during intercourse are possible but rarely occur.13 There are no clinically significant drag interactions with these agents, and the only absolute contraindication to their use is an allergy to the products.
Monitoring for effectiveness is based on patient symptoms. Relief of symptoms can occur within hours of the initial dose, although this is not indicative of cure. It is important for women to finish the recommended course of therapy because many recurrences of Candida vulvovaginiris are thought to result from incomplete treatment.14 Annfimgal activity persists longer than the short courses of therapy (1 or 3 days), and resolution of symptoms may occur several days after treatment, If a woman has not experienced any improvement in symptoms within three days after beginning therapy, or if symptoms persist after a week, she should be referred for clinician evaluation. A pelvic exam and an examination of vaginal secretions should be done to confirm a diagnosis, and rule out pathogens other than Candida albicans. It is estimated that 15-20% of vaginal infections are mixed infections.10 A woman should also be referred for further evaluation if vaginal symptoms recur within two months of nonprescription therapy.
The nonprescription antifungals are not recommended for use by pregnant women. However, under the direction of a physician, topically applied imidazole anrifungal agents are the drugs of choice during pregnancy because there is lit-de systemic absorption. Candida vulvovaginitis tends to be more difficult to cure during pregnancy. For this reason, the prescribed duration of treatment is usually longer (e.g., 1 or 2 weeks for clotrimazole or miconazole and 6 days for buto-conazole).10, 14 Most clinicians recommend that the vaginal antifimgals be used only during the second and third trimesters.13, 15 However, clinical trials, some of which included women in the first trimester of pregnancy, have not shown any adverse effects on the baby or the mother.16 It is not known whether these agents are excreted in breast milk, but it is unlikely that clinically significant concentrations occur. Adverse effects in human infants have not been documented.
When nonprescription antifungal therapy is ineffective, a physician may recommend a second course of vaginal therapy, a longer course of therapy (e.g., 2-3 weeks), the use of boric acid capsules intravaginally, or terconazole therapy this triazole antifimgal is more effective against non-albicans species of Candida).13,17,18 Intravaginal boric acid has been shown to be quite effective for chronic non-candida albicans mycotic vaginal infections with mycologic cure rates of 77-85%. The oral anrifungals—fluconazole, itraconazole, and ketoconazole— have also been studied for the treatment of Candida vulvovaginitis, but only fluconazole (Diflucan™) is currently FDA approved for this indication.
The oral antifiingals are comparable in efficacy to the topical agents and are promoted as compliance-enhancing because of convenience and patient preference for oral therapy.13,15 However, some clinicians feel oral therapy should be reserved for severe, recurrent cases of Candida vulvovaginitis because the risks of oral therapy outweigh the benefits for uncomplicated infections.13 Disadvantages of the oral agents include a greater incidence of side effects, increased risk of serious adverse drug effects, and a potential for drug interactions. Oral therapy can also be more expensive, due to greater cost of the medication and the need for physician visits and laboratory monitoring.
Recurrent Candida vulvovaginitis is difficult to treat and often requires long-term (6 months) suppressive therapy. The vaginal imidazole antifiingals are often administered once or twice weekly as suppression therapy13,15 Oral agents may also be used; 100 mg ketoconazole daily or 150 mg fluconazole once monthly are two common regimens.13,15
Advise women to consult a physician before using the OTC vaginal antifungal products if it is their first experience with vaginal itch or discomfort.
Self-treatment is not appropriate during pregnancy, in a woman with diabetes, or if the woman has symptoms that indicate a systemic infection (e.g., fever, abdominal or back pain). Women taking systemic corticosteroids or anti-cancer medications should not self-treat for Candida vulvovaginitis.
If menses begins during the course of therapy with a vaginal antifungal. therapy should be continued. Instruct women not to use tampons while using a vaginal antifungal, as they can absorb the medication. If a woman prefers not to use these products during menses, treatment can be postponed until afterwards.
Patients should be advised to abstain from sexual intercourse during therapy and instructed that vaginal antifiingals may decrease the effectiveness of condoms. diaphragms, and cervical caps. The use of condoms and diaphragms should be avoided for 72 hours after vaginal insertion of noconazole. Concurrent use of a vaginal antifungal and a contraceptive foam (or cream) can result in decreased effectiveness of both products.
Side effects from vaginal antifiingals are uncommon. Some women experience transient burning, irritation, or itching when therapy is started. There may be some leakage of the product from the vagina, and it is suggested that women use sanitary napkins during therapy.