| Contents | Previous | Next |
The past century has witnessed a remarkable lengthening of the average life span in the United States, from 47 years in 1900 to more than 75 years in the mid-1990s (National Center for Health Statistics [NCHS], 1993). Equally noteworthy has been the increase in the number of persons ages 85 and older (Figure 5-1). These trends will continue well into the next century and be magnified as the numbers of older Americans increase with the aging of the post–World War II baby boom generation.
Millions of older Americans—indeed, the majority—cope constructively with the physical limitations, cognitive changes, and various losses, such as bereavement, that frequently are associated with late life. Research has contributed immensely to our understanding of developmental processes that continue to unfold as we age. Drawing on new scientific information and acting on clinical common sense, mental health and general health care providers are increasingly able to suggest mental health strategies and skills that older adults can hone to make this stage of the life span satisfying and rewarding.
The capacity for sound mental health among older adults notwithstanding, a substantial proportion of the population 55 and older—almost 20 percent of this age group—experience specific mental disorders that are not part of “normal” aging (see Table 5-1). Research that has helped differentiate mental disorders from “normal” aging has been one of the more important achievements of recent decades in the field of geriatric health. Unrecognized or untreated, however, depression, Alzheimer’s disease, alcohol and drug misuse and abuse, anxiety, late-life schizophrenia, and other conditions can be severely impairing, even fatal; in the United States, the rate of suicide, which is frequently a consequence of depression, is highest among older adults relative to all other age groups (Hoyert et al., 1999).
 |
| Figure 5-1. Increases in the percent of the U.S. Population over age 65 years and over 85 years (Malmgren, 1994). |
| Table 5-1. Best estimate 1-year prevalence rates based on Epidemiologic Catchment Area, age 55+ | |
| Prevalence (%) | |
| Any Anxiety Disorder | 11.4 |
| Simple Phobia | 7.3 |
| Social Phobia | 1.0 |
| Agoraphobia | 4.1 |
| Panic Disorder | 0.5 |
| Obsessive-Compulsive Disorder | 1.5 |
| Any Mood Disorder | 4.4 |
| Major Depressive Episode | 3.8 |
| Unipolar Major Depression | 3.7 |
| Dysthymia | 1.6 |
| Bipolar I | 0.2 |
| Bipolar II | 0.1 |
| Schizophrenia | 0.6 |
| Somatization | 0.3 |
| Antisocial Personality Disorder | 0.0 |
| Anorexia Nervosa | 0.0 |
| Severe Cognitive Impairment | 6.6 |
| Any Disorder | 19.8 |
| Source: D. Regier & W. Narrow, personal communication, 1999. | |
The clinical challenges such conditions present may be exacerbated, moreover, by the manner in which they both affect and are affected by general medical conditions or by changes in cognitive capacities. Another complicating factor is that many older people, disabled by or at risk for mental disorders, find it difficult to afford and obtain needed medical and related health care services. Late-life mental disorders also can pose difficulties for the burgeoning numbers of family members who assist in caretaking tasks for their loved ones (Light & Lebowitz, 1991).
Fortunately, the past 15 to 20 years have been marked by rapid growth in the number of clinical, research, and training centers dedicated to the mental illness- and mental health-related needs of older people. As evident in this chapter, much has been learned. The chapter reviews, first, normal developmental milestones of aging, highlighting the adaptive capacities that enable many older people to change, cope with loss, and pursue productive and fulfilling activities. The chapter then considers mental disorders in older people—their diagnosis and treatment, and the various risk factors that may complicate the course or outcome of treatment. Risk factors include co-occurring, or comorbid, general medical conditions, the high numbers of medications many older individuals take, and psychosocial stressors such as bereavement or isolation. These are cause for concern, but, as the chapter notes, they also point the way to possible new preventive interventions. The goal of such prevention strategies may be to limit disability or to postpone or even eliminate the need to institutionalize an ill person (Lebowitz & Pearson, in press). The chapter reviews gains that have been realized in making appropriate mental health services available to older people and the challenges associated with the delivery of services to this population. The advantages of a decisive shift away from mental hospitals and nursing homes to treatment in community-based settings today are in jeopardy of being undermined by fragmentation and insufficient availability of such services (Gatz & Smyer, 1992; Cohen & Cairl, 1996). The chapter examines obstacles and opportunities in the service delivery sphere, in part through the lens of public and private sector financing policies and managed care.
Finally, the chapter reviews the supports for older persons that extend beyond traditional, formal treatment settings. Through support networks, self-help groups, and other means, consumers, families, and communities are assuming an increasingly important role in treating and preventing mental health problems and disorders among older persons.
With improved diet, physical fitness, public health, and health care, more adults are reaching age 65 in better physical and mental health than in the past. Trends show that the prevalence of chronic disability among older people is declining: from 1982 to 1994, the prevalence of chronic disability diminished significantly, from 24.9 to 21.3 percent of the older population (Manton et al., 1997). While some disability is the result of more general losses of physiological functions with aging (i.e., normal aging), extreme disability in older persons, including that which stems from mental disorders, is not an inevitable part of aging (Cohen, 1988; Rowe & Kahn, 1997).
Normal aging is a gradual process that ushers in some physical decline, such as decreased sensory abilities (e.g., vision and hearing) and decreased pulmonary and immune function (Miller, 1996; Carman, 1997). With aging come certain changes in mental functioning, but very few of these changes match commonly held negative stereotypes about aging (Cohen, 1988; Rowe & Kahn, 1997). In normal aging, important aspects of mental health include stable intellectual functioning, capacity for change, and productive engagement with life.
Cognition subsumes intelligence, language, learning, and memory. With advancing years, cognitive capacity with aging undergoes some loss, yet important functions are spared. Moreover, there is much variability between individuals, variability that is dependent upon lifestyle and psychosocial factors (Gottlieb, 1995). Most important, accumulating evidence from human and animal research finds that lifestyle modifies genetic risk in influencing the outcomes of aging (Finch & Tanzi, 1997). This line of research is beginning to dispel the pejorative stereotypes of older people as rigidly shaped by heredity and incapable of broadening their pursuits and acquiring new skills.
A large body of research, including both cross-sectional studies and longitudinal studies, has investigated changes in cognitive function with aging. Studies have found that working memory declines with aging, as does long-term memory (Siegler et al., 1996), with decrements more apparent in recall than in recognition capacities. Slowing or some loss of other cognitive functions takes place, most notably in information processing, selective attention, and problem-solving ability, yet findings are variable (Siegler et al., 1996). These cognitive changes translate into a slower pace of learning and greater need for repetition of new information. Vocabulary increases slightly until the mid-70s, after which it declines (Carman, 1997). In older people whose IQ declines, somatic illness is implicated in some cases (Cohen, 1988). Fluid intelligence, a form of intelligence defined as the ability to solve novel problems, declines over time, yet research finds that fluid intelligence can be enhanced through training in cognitive skills and problem-solving strategies (Baltes et al., 1989).
Memory complaints are exceedingly common in older people, with 50 to 80 percent reporting subjective memory complaints (cited in Levy-Cushman & Abeles, in press). However, subjective memory complaints do not correspond with actual performance. In fact, some who complain about memory display performance superior to those who do not complain (Collins & Abeles, 1996). Memory complaints in older people, according to several studies, are thought to be more a product of depression than of decline in memory performance (cited in Levy-Cushman & Abeles, in press). (The importance of proper diagnosis and treatment of depression is emphasized in subsequent sections of this chapter.) Studies attempting to treat memory complaints associated with normal aging—using either pharmacological or psychosocial means—have been, with few exceptions, unsuccessful (Crook, 1993). In one of these exceptions, a recent study demonstrated a significant reduction in memory complaints with training workshops for healthy older people. The workshops stressed not only memory promotion strategies, but also ways of dealing with expectations and perceptions about memory loss (Levy-Cushman & Abeles, in press).
One large, ongoing longitudinal study found high cognitive performance to be dependent on four factors, ranked here in decreasing order of importance: education, strenuous activity in the home, peak pulmonary flow rate, and “self-efficacy,” which is a personality measure defined by the ability to organize and execute actions required to deal with situations likely to happen in the future (Albert et al., 1995). Education, as assessed by years of schooling, is the strongest predictor of high cognitive functioning. This finding suggests that education not only has salutary effects on brain function earlier in life, but also foreshadows sustained productive behavior in later life, such as reading and performing crossword puzzles (Rowe & Kahn, 1997).
The coexistence of mental and somatic disorders (i.e., comorbidity) is common (Kramer et al., 1992). Some disorders with primarily somatic symptoms can cause cognitive, emotional, and behavioral symptoms as well, some of which rise to the level of mental disorders. At that point, the mental disorder may result from an effect of the underlying disorder on the central nervous system (e.g., dementia due to a medical condition such as hypothyroidism) or an effect of treatment (e.g., delirium due to a prescribed medication). Likewise, mental problems or disorders can lead to or exacerbate other physical conditions by decreasing the ability of older adults to care for themselves, by impairing their capacity to rally social support, or by impairing physiological functions. For example, stress increases the risk of coronary heart disease and can suppress cellular immunity (McEwen, 1998). Depression can lead to increased mortality from heart disease and possibly cancer (Frasure-Smith et al., 1993, 1995; Penninx et al., 1998).
A new model postulates that successful aging is contingent upon three elements: avoiding disease and disability, sustaining high cognitive and physical function, and engaging with life (Rowe & Kahn, 1997). The latter encompasses the maintenance of interpersonal relationships and productive activities, as defined by paid or unpaid activities that generate goods or services of economic value. The three major elements are considered to act in concert, for none is deemed sufficient by itself for successful aging. This new model broadens the reach of health promotion in aging to entail more than just disease prevention.
Descriptive research reveals evidence of the capacity for constructive change in later life (Cohen, 1988). The capacity to change can occur even in the face of mental illness, adversity, and chronic mental health problems. Older persons display flexibility in behavior and attitudes and the ability to grow intellectually and emotionally. Time plays a key role. Externally imposed demands upon one’s time may diminish, and the amount of time left at this stage in life can be significant. In the United States in the late 20th century, late-life expectancy approaches another 20 years at the age of 65. In other words, average longevity from age 65 today approaches what had been the average longevity from birth some 2,000 years ago. This leaves plenty of time to embark upon new social, psychological, educational, and recreational pathways, as long as the individual retains good health and material resources.
In his classic developmental model, Erik Erikson characterized the final stage of human development as a tension between “ego integrity and despair” (Erikson, 1950). Erikson saw the period beginning at age 65 years as highly variable. Ideally, individuals at this stage witness the flowering of seeds planted earlier in the prior seven stages of development. When they achieve a sense of integrity in life, they garner pride from their children, students and protégés, and past accomplishments. With contentment comes a greater tolerance and acceptance of the decline that naturally accompanies the aging process. Failure to achieve a satisfying degree of ego integrity can be accompanied by despair.
Cohen (in press) has proposed that with increased longevity and health, particularly for people with adequate resources, aging is characterized by two human potential phases. These phases, which emphasize the positive aspects of the final stages of the life cycle, are termed Retirement/Liberation and Summing Up/Swan Song.
Retirement often is viewed as the most important life event prior to death. Retirement frequently is associated with negative myths and stereotypes (Sheldon et al., 1975; Bass, 1995). Cohen points out, however, that most people fare well in retirement. They have the opportunity to explore new interests, activities, and relationships due to retirement’s liberating qualities. In the Retirement/Liberation phase, new feelings of freedom, courage, and confidence are experienced. Those at risk for faring poorly are individuals who typically do not want to retire, who are compelled to retire because of poor health, or who experience a significant decline in their standard of living (Cohen, 1988). In short, the liberating experience of having more time and an increased sense of freedom can be the springboard for creativity in later life. Creative achievement by older people can change the course of an individual, family, community, or culture.
In the late-life Summing Up/Swan Song phase, there is a tendency to appraise one’s life work, ideas, and discoveries and to share them with family or society. The desire to sum up late in life is driven by varied feelings, such as the desire to complete one’s life work, the desire to give back after receiving much in life, or the fear of time evaporating. Important opportunities for creative sharing and expression ensue. There is a natural tendency with aging to reminisce and elaborate stories that has propelled the development of reminiscence therapy for health promotion and disease prevention. The swan song, the final part of this phase, connotes the last act or final creative work of a person before retirement or death.
There is much misunderstanding about thoughts of death in later life. Depression, serious loss, and terminal illness trigger the sense of mortality, regardless of age. Contrary to popular stereotypes, studies on aging reveal that most older people generally do not have a fear or dread of death in the absence of being depressed, encountering serious loss, or having been recently diagnosed with a terminal illness (Kastenbaum, 1985). Periodic thoughts of death—not in the form of dread or angst—do occur. But these are usually associated with the death of a friend or family member. When actual dread of death does occur, it should not be dismissed as accompanying aging, but rather as a signal of underlying distress (e.g., depression). This is particularly important in light of the high risk of suicide among depressed older adults, which is discussed later in this chapter.
Many older adults experience loss with aging—loss of social status and self-esteem, loss of physical capacities, and death of friends and loved ones. But in the face of loss, many older people have the capacity to develop new adaptive strategies, even creative expression (Cohen, 1988, 1990). Those experiencing loss may be able to move in a positive direction, either on their own, with the benefit of informal support from family and friends, or with formal support from mental health professionals.
The life and work of William Carlos Williams are illustrative. Williams was a great poet as well as a respected physician. In his 60s, he suffered a stroke that prevented him from practicing medicine. The stroke did not affect his intellectual abilities, but he became so severely depressed that he needed psychiatric hospitalization. Nonetheless, Williams, with the help of treatment for a year, surmounted the depression and for the next 10 years wrote luminous poetry, including the Pulitzer Prize-winning Pictures From Bruegel, which was published when he was 79. In his later life, Williams wrote about “old age that adds as it takes away.” What Williams and his poetry epitomize is that age can be the catalyst for tapping into creative potential (Cohen, 1998a).
Loss of a spouse is common in late life. About 800,000 older Americans are widowed each year. Bereavement is a natural response to death of a loved one. Its features, almost universally recognized, include crying and sorrow, anxiety and agitation, insomnia, and loss of appetite (Institute of Medicine [IOM], 1984). This constellation of symptoms, while overlapping somewhat with major depression, does not by itself constitute a mental disorder. Only when symptoms persist for 2 months and longer after the loss does the DSM-IV permit a diagnosis of either adjustment disorder or major depressive disorder. Even though bereavement of less than 2 months’ duration is not considered a mental disorder, it still warrants clinical attention (DSM-IV). The justification for clinical attention is that bereavement, as a highly stressful event, increases the probability of, and may cause or exacerbate, mental and somatic disorders.
Bereavement is an important and well-established risk factor for depression. At least 10 to 20 percent of widows and widowers develop clinically significant depression during the first year of bereavement. Without treatment, such depressions tend to persist, become chronic, and lead to further disability and impairments in general health, including alterations in endocrine and immune function (Zisook & Shuchter, 1993; Zisook et al., 1994). Several preventive interventions, including participation in self-help groups, have been shown to prevent depression among widows and widowers, although one study suggested that self-help groups can exacerbate depressive symptoms in certain individuals (Levy et al., 1993). These are described later in this chapter.
Bereavement-associated depression often coexists with another type of emotional distress, which has been termed traumatic grief (Prigerson et al., in press). The symptoms of traumatic grief, although not formalized as a mental disorder in DSM-IV, appear to be a mixture of symptoms of both pathological grief and post-traumatic stress disorder (Frank et al., 1997a). Such symptoms are extremely disabling, associated with functional and health impairment and with persistent suicidal thoughts, and may well respond to pharmacotherapy (Zygmont et al., 1998). Increased illness and mortality from suicide are the most serious consequences of late-life depression.
The dynamics around loss in later life need greater clarification. One pivotal question is why some, in confronting loss with aging, succumb to depression and suicide—which, as noted earlier, has its highest frequency after age 65—while others respond with new adaptive strategies. Research on health promotion also needs to identify ways to prevent adverse reactions and to promote positive responses to loss in later life. Meanwhile, despite cultural attitudes that older persons can handle bereavement by themselves or with support from family and friends, it is imperative that those who are unable to cope be encouraged to access mental health services. Bereavement is not a mental disorder but, if unattended to, has serious mental health and other health consequences.
Older adults are encumbered by many of the same mental disorders as are other adults; however, the prevalence, nature, and course of each disorder may be very different. This section provides a general overview of assessment, diagnosis, and treatment of mental disorders in older people. Its purpose is to describe issues common to many mental disorders. Subsequent sections of this chapter provide more detailed reviews of late-life depression and Alzheimer’s disease. Also, to shed light on the range and frequency of disorders that impair the mental well-being of older Americans, the chapter reviews the impact on older adults of anxiety, schizophrenia, and alcohol and substance abuse.
Assessment and diagnosis of late-life mental disorders are especially challenging by virtue of several distinctive characteristics of older adults. First, the clinical presentation of older adults with mental disorders may be different from that of other adults, making detection of treatable illness more difficult. For example, many older individuals present with somatic complaints and experience symptoms of depression and anxiety that do not meet the full criteria for depressive or anxiety disorders. The consequences of these subsyndromal conditions may be just as deleterious as the syndromes themselves. Failure to detect individuals who truly have treatable mental disorders represents a serious public health problem (National Institutes of Health [NIH] Consensus Development Panel on Depression in Late Life, 1992).
Detection of mental disorders in older adults is complicated further by high comorbidity with other medical disorders. The symptoms of somatic disorders may mimic or mask psychopathology, making diagnosis more taxing. In addition, older individuals are more likely to report somatic symptoms than psychological ones, leading to further underidentification of mental disorders (Blazer, 1996b).
Primary care providers carry much of the burden for diagnosis of mental disorders in older adults, and, unfortunately, the rates at which they recognize and properly identify disorders often are low. With respect to depression, for example, a significant number of depressed older adults are neither diagnosed nor treated in primary care (NIH Consensus Development Panel on Depression in Late Life, 1992; Unutzer et al., 1997b). In one study of primary care physicians, only 55 percent of internists felt confident in diagnosing depression, and even fewer (35 percent of the total) felt confident in prescribing antidepressants to older persons (Callahan et al., 1992). Physicians were least likely to report that they felt “very confident” in evaluating depression in other late-life conditions (Gallo et al., in press). Researchers estimate that an unmet need for mental health services may be experienced by up to 63 percent of adults aged 65 years and older with a mental disorder, based on prevalence estimates from the Epidemiologic Catchment Area (ECA) study (Rabins, 1996).
The large unmet need for treatment of mental disorders reflects patient barriers (e.g., preference for primary care, tendency to emphasize somatic problems, reluctance to disclose psychological symptoms), provider barriers (e.g., lack of awareness of the manifestations of mental disorders, complexity of treatment, and reluctance to inform patients of a diagnosis), and mental health delivery system barriers (e.g., time pressures, reimbursement policies).
Stereotypes about normal aging also can make diagnosis and assessment of mental disorders in late life challenging. For example, many people believe that “senility” is normal and therefore may delay seeking care for relatives with dementing illnesses. Similarly, patients and their families may believe that depression and hopelessness are natural conditions of older age, especially with prolonged bereavement.
Cognitive decline, both normal and pathological, can be a barrier to effective identification and assessment of mental illness in late life. Obtaining an accurate history, which may need to be taken from family members, is important for diagnosis of most disorders and especially for distinguishing between somatic and mental disorders. Normal decline in short-term memory and especially the severe impairments in memory seen in dementing illnesses hamper attempts to obtain good patient histories. Similarly, cognitive deficits are prominent features of many disorders of late life that make diagnosis of psychiatric disorders more difficult.
Prevention in mental health has been seen until recently as an area limited to childhood and adolescence. Now there is mounting awareness of the value of prevention in the older population. While the body of published literature is not as extensive as that for diagnosis or treatment, investigators are beginning to shape new approaches to prevention. Yet because prevention research is driven, in part, by refined understanding of disease etiology—and etiology research itself continues to be rife with uncertainty—prevention advances are expected to lag behind those in etiology.
There are many ways in which prevention models can be applied to older individuals, provided a broad view of prevention is used (Lebowitz & Pearson, in press). Such a broad view entails interventions for reducing the risk of developing, exacerbating, or experiencing the consequences of a mental disorder. Consequently, this section covers primary prevention (including the prevention of depression and suicide), treatment-related prevention, prevention of excess disability, and prevention of premature institutionalization. However, many of the research advances noted in this section have yet to be translated into practice. Given the frequency of memory complaints and depression, the time may soon arrive for older adults to be encouraged to have “mood and memory checkups” in the same manner that they are now encouraged to have physical checkups (N. Abeles, personal communication, 1998).
Primary prevention, the prevention of disease before it occurs, can be applied to late-onset disorders. Progress in our understanding of etiology, risk factors, pathogenesis, and the course of mental disorders—discussed later in this chapter for depression, Alzheimer’s disease, and other conditions—stimulates and channels the development of prevention interventions.
The largest body of primary prevention research focuses on late-life depression, where some progress has been documented. With other disorders, primary prevention research is in its infancy. Prevention in Alzheimer’s disease might target individuals at increased genetic risk with prophylactic nutritional (e.g., vitamin E), cholinergic, or amyloid-targeting interventions. Prevention research on late-onset schizophrenia might explore potential protective factors, such as estrogen.
Depression is strikingly prevalent among older people. As noted below, 8 to 20 percent of older adults in the community and up to 37 percent in primary care settings experience symptoms of depression.
One approach to preventing depression is through grief counseling for widows and widowers. For example, participation in self-help groups appears to ameliorate depression, improve social adjustment, and reduce the use of alcohol and other drugs of abuse in widows (Constantino, 1988; Lieberman & Videka-Sherman, 1986). The efficacy of self-help groups approximates that of brief psychodynamic psychotherapy in older bereaved individuals without significant prior psychopathology (Marmar et al., 1988). The battery of psychosocial and pharmacological treatments to prevent recurrences of depression (i.e., secondary prevention) is discussed later in this chapter under the section on depression.
Depression is a foremost risk factor for suicide in older adults (Conwell, 1996; Conwell et al., 1996). Older people have the highest rates of suicide in the U.S. population: suicide rates increase with age, with older white men having a rate of suicide up to six times that of the general population (Kachur et al., 1995; Hoyert et al., 1999). Despite the prevalence of depression and the risk it confers for suicide, depression is neither well recognized nor treated in primary care settings, where most older adults seek and receive health care (Unutzer et al., 1997a). Studies described in the depression section of this chapter have found that undiagnosed and untreated depression in the primary care setting plays a significant role in suicide (Caine et al., 1996). This awareness has prompted the development of suicide prevention strategies expressly for primary care. One of the first published suicide prevention studies, an uncontrolled experiment conducted in Sweden, suggested that a depression training program for general practitioners reduces suicide (Rihmer et al., 1995). Suicide interventions, especially in the primary care setting, have become a priority of the U.S. Public Health Service, with lead responsibility assumed by the Office of the Surgeon General and the National Institute of Mental Health.
Depression and suicide prevention strategies also are important for nursing home residents. About half of patients newly relocated to nursing homes are at heightened risk for depression (Parmelee et al., 1989).
Prevention of relapse or recurrence of the underlying mental disorder is important for improving the mental health of older patients with mental disorders. For example, treatments that are applied with adequate intensities for depression (Schneider, 1996) and for depression in Alzheimer’s disease (Small et al., 1997) may prevent relapse or recurrence. Substantial residual disability in chronically mentally ill individuals (Lebowitz et al., 1997) suggests that treatment must be approached from a longer term perspective (Reynolds et al., 1996).
Prevention of medication side effects and adverse reactions also is an important goal of treatment-related prevention efforts in older adults. Comorbidity and the associated polypharmacy for multiple conditions are characteristic of older patients. New information on the genetic basis of drug metabolism and on the action of drug-metabolizing enzymes can lead to a better understanding of complex drug interactions (Nemeroff et al., 1996). For example, many of the selective serotonin reuptake inhibitors compete for the same metabolic pathway used by beta-blockers, type 1C antiarrhythmics, and benzodiazepines (Nemeroff et al., 1996). This knowledge can assist the clinician in choosing medications that can prevent the likelihood of side effects. In addition, many older patients require antipsychotic treatment for management of behavioral symptoms in Alzheimer’s disease, schizophrenia, and depression. Although doses tend to be quite low, age and length of treatment represent major risk factors for movement disorders (Saltz et al., 1991; Jeste et al., 1995a). Recent research on older people suggests that the newer antipsychotics present a much lower risk of movement disorders, highlighting their importance for prevention (Jeste et al., in press). Finally, body sway and postural stability are affected by many drugs, although there is wide variability within classes of drugs (Laghrissi-Thode et al., 1995). Minimizing the risk of falling, therefore, is another target for prevention research. Falls represent a leading cause of injury deaths among older persons (IOM, 1999).
Prevention efforts in older mentally ill populations also target avoidance of excessive disability. The concept of excess disability refers to the observation that many older patients, particularly those with Alzheimer’s disease and other severe and persistent mental disorders, are more functionally impaired than would be expected according to the stage or severity of their disorder. Medical, psychosocial, and environmental factors all contribute to excess disability. For example, depression contributes to excess disability by hastening functional impairment in patients with Alzheimer’s disease (Ritchie et al., 1998). The fast pace of modern life, with its emphasis on independence, also contributes to excess disability by making it more difficult for older adults with impairments to function autonomously. Attention to depression, anxiety, and other mental disorders may reduce the functional limitations associated with concomitant mental and somatic impairments. Many studies have demonstrated that attention to these factors and aggressive intervention, where appropriate, maximize function (Lebowitz & Pearson, in press).
Another important goal of prevention efforts in older adults is prevention of premature institutionalization. While institutional care is needed for many older patients who suffer from severe and persistent mental disorders, delay of institutional placement until absolutely necessary generally is what patients and family caregivers prefer. It also has significant public health impact in terms of reducing costs. A randomized study of counseling and support versus usual care for family caregivers of patients with Alzheimer’s disease found the intervention to have delayed patients’ nursing home admission by over 300 days (Mittelman et al., 1996). The intervention also resulted in a significant reduction in depressive symptoms in the caregivers. The intervention consisted of three elements: individual and family counseling sessions, support group participation, and availability of counselors to assist with patient crises.
The growing importance of avoiding premature institutionalization is illustrated by its use as one measure of the effectiveness of pharmacotherapy in older individuals. For example, clinical trials of drugs for Alzheimer’s disease have begun using delay of institutionalization as a primary outcome (Sano et al., 1997) or as a longer-term outcome in a followup study after the double-blind portion of the clinical trial ended (Knopman et al., 1996).
Treatment of mental disorders in older adults encompasses pharmacological interventions, electroconvulsive therapy, and psychosocial interventions. While the pharmacological and psychosocial interventions used to treat mental health problems and specific disorders may be identical for older and younger adults, characteristics unique to older adults may be important considerations in treatment selection.
The special considerations in selecting appropriate medications for older people include physiological changes due to aging; increased vulnerability to side effects, such as tardive dyskinesia; the impact of polypharmacy; interactions with other comorbid disorders; and barriers to compliance. All are discussed below.
The aging process leads to numerous changes in physiology, resulting in altered blood levels of certain medications, prolonged pharmacological effects, and greater risk for many side effects (Kendell et al., 1981). Changes may occur in the absorption, distribution, metabolism, and excretion of psychotropic medications (Pollock & Mulsant, 1995).
As people age, there is a gradual decrease in gastrointestinal motility, gastric blood flow, and gastric acid production (Greenblatt et al., 1982). This slows the rate of absorption, but the overall extent of gastric absorption is probably comparable to that in other adults. The aging process is also associated with a decrease in total body water, a decrease in muscle mass, and an increase in adipose tissue (Borkan et al., 1983). Drugs that are highly lipophilic, such as neuroleptics, are therefore more likely to be accumulated in fatty tissues in older patients than they are in younger patients.
The liver undergoes changes in blood flow and volume with age. Phase I metabolism (oxidation, reduction, hydrolysis) may diminish or remain unchanged, while phase II metabolism (conjugation with an endogenous substrate) does not change with aging. Renal blood flow, glomerular surface area, tubular function, and reabsorption mechanisms all have been shown to diminish with age. Diminished renal excretion may lead to a prolonged half-life and the necessity for a lower dose or longer dosing intervals.
Pharmacodynamics, which refers to the drug’s effect on its target organ, also can be altered in older individuals. An example of aging-associated pharmacodynamic change is diminished central cholinergic function contributing to increased sensitivity to the anticholinergic effects of many neuroleptics and antidepressants in older adults (Molchan et al., 1992).
Because of the pharmacokinetic and pharmacodynamic concerns presented above, it is often recommended that clinicians “start low and go slow” when prescribing new psychoactive medications for older adults. In other words, efficacy is greatest and side effects are minimized when initial doses are small and the rate of increase is slow. Nevertheless, the medication should generally be titrated to the regular adult dose in order to obtain the full benefit. The potential pitfall is that, because of slower titration and the concomitant need for more frequent medical visits, there is less likelihood of older adults receiving an adequate dose and course of medication.
Older people encounter an increased risk of side effects, most likely the result of taking multiple drugs or having higher blood levels of a given drug. The increased risk of side effects is especially true for neuroleptic agents, which are widely prescribed as treatment for psychotic symptoms, agitation, and behavioral symptoms. Neuroleptic side effects include sedation, anticholinergic toxicity (which can result in urinary retention, constipation, dry mouth, glaucoma, and confusion), extrapyramidal symptoms (e.g., parkinsonism, akathisia, and dystonia), and tardive dyskinesia. Chapter 4 contains more detailed information about the side effects of neuroleptics.
Tardive dyskinesia is a frequent and persistent side effect that occurs months to years after initiation of neuroleptics. In older adults, tardive dyskinesia typically entails abnormal movements of the tongue, lips, and face. In a recent study of older outpatients treated with conventional neuroleptics the incidence of tardive dyskinesia after 12 months of neuroleptic treatment was 29 percent of the patients. At 24 and 36 months, the mean cumulative incidence was 50.1 percent and 63.1 percent, respectively (Jeste et al., 1995a). This study demonstrates the high risk of tardive dyskinesia in older patients even with low doses of conventional neuroleptics. Studies of younger adult patients reveal an annual cumulative incidence of tardive dyskinesia at 4 to 5 percent (Kane et al., 1993).
Unlike conventional neuroleptics, the newer atypical ones, such as clozapine, risperidone, olanzapine, and quetiapine, apparently confer several advantages with respect to both efficacy and safety. These drugs are associated with a lower incidence of extrapyramidal symptoms than conventional neuroleptics are. For clozapine, the low risk of tardive dyskinesia is well established (Kane et al., 1993). The incidence of tardive dyskinesia with other atypical antipsychotics is also likely to be lower than that with conventional neuroleptics because extrapyramidal symptoms have been found to be a risk factor for tardive dyskinesia in older adults (Saltz et al., 1991; Jeste et al., 1995a). The determination of exact risk of tardive dyskinesia with these newer drugs needs long-term studies.
In addition to the effects of aging on pharmacokinetics and pharmacodynamics and the increased risk of side effects, older individuals with mental disorders also are more likely than other adults to be medicated with multiple compounds, both prescription and nonprescription (i.e., polypharmacy). Older adults (over the age of 65) fill an average of 13 prescriptions a year (for original or refill prescriptions), which is approximately three times the number filled by younger individuals (Chrischilles et al., 1992). Polypharmacy greatly complicates effective treatment of mental disorders in older adults. Specifically, drug-drug interactions are of concern, both in terms of increasing side effects and decreasing efficacy of one or both compounds.
Compliance with the treatment regimen also is a special concern in older adults, especially in those with moderate or severe cognitive deficits. Physical problems, such as impaired vision, make it likely that instructions may be misread or that one medicine may be mistaken for another. Cognitive impairment may also make it difficult for patients to remember whether or not they have taken their medication. Although in general, older patients are more compliant about taking psychoactive medications than other types of drugs (Cooper et al., 1982), when noncompliance does occur, it may be less easily detected, more serious, less easily resolved, mistaken for symptoms of a new disease, or even falsely labeled as “old-age” symptomatology. Accordingly, greater emphasis must be placed on strict compliance by patients in this age group (Lamy et al., 1992). Medication noncompliance takes different forms in older adults, that is, overuse and abuse, forgetting, and alteration of schedules and doses. The most common type of deliberate noncompliance among older adults may be the underuse of the prescribed drug, mainly because of side effects and cost considerations. Factors that contribute to medication noncompliance in older patients include inadequate information given to them regarding the necessity for drug treatment, unclear prescribing directions, suboptimal doctor-patient relationship, the large number of times per day drugs must be taken, and the large number of drugs that are taken at the same time (Lamy et al., 1992). Better compliance may be achieved by giving simple instructions and by asking specific questions to make sure that the patient understands directions.
Several types of psychosocial interventions have proven effective in older patients with mental disorders, but the research is more limited than that on pharmacological interventions (see Klausner & Alexopoulos, in press). Both types are frequently used in combination. Most of the research has been restricted to psychosocial treatments for depression, although, as discussed below, there is mounting interest in dementia. For other mental disorders, psychosocial interventions found successful for younger adults are often tailored to older people in the practice setting without the benefit of efficacy research.
Despite the relative paucity of research, psychosocial interventions may be preferred for some older patients, especially those who are unable to tolerate, or prefer not to take, medication or who are confronting stressful situations or low degrees of social support (Lebowitz et al., 1997). The benefits of psychosocial interventions are likely to assume greater prominence as a result of population demographics: as the number of older people grows, progressively more older people in need of mental health treatment—especially the very old—are expected to be suffering from greater levels of comorbidity or dealing with the stresses associated with disability. Psychosocial interventions not only can help relieve the symptoms of a variety of mental disorders and related problems but also can play more diverse roles: they can help strengthen coping mechanisms, encourage (and monitor) patients’ compliance with medications, and promote healthy behavior (Klausner & Alexopoulos, in press).
New approaches to service delivery are being designed to realize the benefits of established psychosocial interventions. Many older people are not comfortable with traditional mental health settings, partially as a result of stigma (Waters, 1995). In fact, many older people prefer to receive treatment for mental disorders by their primary care physicians, and most older people do receive such care in the primary care setting (Brody et al., 1997; Unutzer et al., 1997a). Since older people show willingness to accept psychosocial interventions in the primary care setting, new models are striving to integrate into the primary care setting the delivery of specialty mental health services. The section of this chapter on service delivery discusses new models in greater detail.
A problem common to both pharmacological and psychosocial interventions is the disparity between treatment efficacy, as demonstrated in randomized controlled clinical trials, and effectiveness in real-world settings. While this problem is certainly not unique to older people (see Chapter 2 for a broader discussion of the problem), this problem is especially significant for older people with mental disorders. Older people are often undertreated for their mental disorders in primary care settings (Unutzer et al., 1997a). When they do receive appropriate treatment, older people are more likely than other people to have comorbid disorders and social problems that reduce treatment effectiveness (Unutzer et al., 1997a). An additional overlay of barriers, including financing and systems of care, is discussed later in this chapter.
Depression in older adults not only causes distress and suffering but also leads to impairments in physical, mental, and social functioning. Despite being associated with excess morbidity and mortality, depression often goes undiagnosed and untreated. The startling reality is that a substantial proportion of older patients receive no treatment or inadequate treatment for their depression in primary care settings, according to expert consensus (NIH Consensus Development Panel on Depression in Late Life, 1992; Lebowitz et al., 1997). Part of the problem is that depression in older people is hard to disentangle from the many other disorders that affect older people, and its symptom profile is somewhat different from that in other adults. Depressive symptoms are far more common than full-fledged major depression. However, several depressive symptoms together represent a condition—explained below as “minor depression”—that can be as disabling as major depression (Unutzer et al., 1997a). Minor depression, despite the implications of the term, is major in its prevalence and impact. Eight to 20 percent of older adults in the community and up to 37 percent in primary care settings suffer from depressive symptoms. Treatment is successful, with response rates between 60 and 80 percent, but the response generally takes longer than that for other adults. In addition to reviewing information on prevalence and treatment, this section also discusses depression’s course, barriers to diagnosis, interactions with physical disease, consequences, cost, and etiology.
The term “major depression” refers to conditions with a major depressive episode, such as major depressive disorder, bipolar disorder, and related conditions. Major depressive disorder, the most common type of major depression in adults, is characterized by one or more episodes that include the following symptoms: depressed mood, loss of interest or pleasure in activities, significant weight loss or gain, sleep disturbance, psychomotor agitation or retardation, fatigue, feelings of worthlessness, loss of concentration, and recurrent thoughts of death or suicide. (For further discussion of the diagnosis of major depressive disorder, see Chapter 4.) Major depressive disorder cannot be diagnosed if symptoms last for less than 2 months after bereavement, among other exclusionary factors (DSM-IV).
Most older patients with symptoms of depression do not meet the full criteria for major depression. The new diagnostic entity of minor depression has been proposed to characterize some of these patients. “Minor depression,” a subsyndromal form of depression, is not yet recognized as an official disorder, and DSM-IV proposes further research on it.
Minor depression is more frequent than major depression, with 8 to 20 percent of older community residents displaying symptoms (Alexopoulos, 1997; Gallo & Lebowitz, 1999). The diagnosis of minor depression is not yet standardized; the research criteria proposed in DSM-IV are the same as those for major depression, but a diagnosis would require fewer symptoms and less impairment. Minor depression, in fact, is not thought to be a single syndrome, but rather a heterogeneous group of syndromes that may signify either an early or residual form of major depression, a chronic, though mild, form of depression that does not present with a full array of symptoms at any one time, called dysthymia, or a response to an identifiable stressor (Judd et al., 1994; Pincus & Wakefield-Davis, 1997). Since depression is more difficult to assess and detect in older adults, research is needed on what clinical features might help identify older adults at increased risk for sustained depressive symptoms and suicide.
Both major and minor depression are associated with significant disability in physical, social, and role functioning (Wells et al., 1989). The degree of disability may not be as great with minor depression, but because of its higher prevalence, minor depression is associated with 51 percent more days lost from work than is major depression (Broadhead et al., 1990). Major and minor depression are associated with high health care utilization and poor quality of life (see Unutzer et al., 1997a, for a review).
Major or minor depression diagnosed with first onset later than age 60 has been termed late-onset depression. Late-onset depression is not a diagnosis; rather, it refers to a subset of patients with major or minor depression whose later age at first onset imparts slightly different clinical characteristics, suggesting the possibility of distinct etiology. Late-onset depression shares many clinical characteristics with early-onset depression, yet some distinguishing features exist. Patients with late-onset depression display greater apathy (Krishnan et al., 1995) and less lifetime personality dysfunction (Abrams et al., 1994). Cognitive deficits may be more prominent, with more impaired executive and memory functioning (Salloway et al., 1996) and greater medial temporal lobe abnormalities on magnetic resonance imaging, similar to those seen in dementia (Greenwald et al., 1997). Other studies, however, have shown no differences in cognition between patients with late- and early-onset depression (Holroyd & Duryee, 1997). The risk of recurrence of depression is relatively high among patients with onset of depression after the age of 60 (Reynolds, 1998).
Risk factors for late-onset depression, based on results of prospective studies, include widowhood (Bruce et al., 1990; Zisook & Shuchter, 1991; Harlow et al., 1991; Mendes de Leon et al., 1994), physical illness (Cadoret & Widmer, 1988; Harlow et al., 1991; Bachman et al., 1992), educational attainment less than high school (Wallace & O’Hara, 1992; Gallo et al., 1993), impaired functional status (Bruce & Hoff, 1994), and heavy alcohol consumption (Saunders et al., 1991).
Estimates of the prevalence of major depression vary widely, depending on the definition and the procedure used for counting persons with depression (Gallo & Lebowitz, 1999). Researchers applying DSM criteria for major depression have found 1-year U.S. prevalence rates of about 5 percent or less in older people (Gurland et al., 1996). The prevalence of major depression declines with age, while depressive symptoms increase (symptoms that now might warrant classification as minor depression). Romanoski and colleagues, on the basis of psychiatric interviews of adults in the Baltimore Epidemiologic Catchment Area (ECA), showed that major depression declined with advancing age (Romanoski et al., 1992). Prevalence estimates derived from symptom scales are consistent with the clinical impression that prevalence of depressive symptoms increases with advancing age. Depressive symptoms and syndromes have been identified in 8 to 20 percent of older community residents (Alexopoulos, 1997; Gallo & Lebowitz, 1999) and 17 to 35 percent of older primary care patients (Gurland et al., 1996).
Several incidence studies based on DSM criteria reflect a similar pattern of decline in rates of major depression with advancing age (Eaton et al., 1989; Eaton et al., 1997). The 13-year followup of the participants of the Baltimore Epidemiologic Catchment Area sample revealed, however, that the distribution of the incidence of DSM-based major depression across the life span was bimodal, with a primary peak in the fourth decade and a secondary peak in the sixth decade (Eaton et al., 1997). In contrast to studies based on DSM criteria, several incidence studies report increased rates of depressive symptoms with age. A Swedish study reported that rates of depressive symptoms were highest in the older age groups and that rates of depression had increased in the interval from 1947–1957 to 1957–1972 (Hagnell et al., 1982). Incidence studies reveal an increased risk of depression among women as they age, consistent with findings based on prevalence surveys (Hagnell et al., 1982; Eaton et al., 1989; Gallo et al., 1993).
Thus, both prevalence and incidence studies that rely on DSM-based diagnosis of major depression suggest a decline with age, whereas symptom-based assessment studies show increased rates of depression among older adults, especially women. Evidence that older adults are less likely than younger persons to report feelings of dysphoria (i.e., sadness, unhappiness, or irritability) suggests that the standard criteria for depression may be more difficult to apply to older adults (Gallo et al., 1994) or that older adults are disinclined to report such feelings.
Other mood disorders, such as dysthymia, bipolar disorder, and hypomania,1 also are present in older individuals. Little difference has been found in the prevalence of affective disorders between African Americans and whites over the age of 65 (Weissman et al., 1991). The prevalence of bipolar disorder among people aged 65 and over is reportedly less than 1 percent (Robins & Regier, 1991). Approximately 5 to 10 percent of older patients presenting with mood disorders are manic or hypomanic (Yassa et al., 1988). However, these mood disorders will not be the focus of this section of the report, as they are much less common in older adults than depression.
The underdiagnosis and undertreatment of depression in primary care represent a serious public health problem (NIH Consensus Development Panel on Depression in Late Life, 1992). One study found that only about 11 percent of depressed patients in primary care received adequate antidepressant treatment (in terms of dose and duration of pharmacotherapy), while 34 percent received inadequate treatment and 55 percent received no treatment (Katon et al., 1992).
There are many barriers to the diagnosis of depression in late life. Some of these barriers reflect the nature of the disorder: depression occurs in a complex medical and psychosocial context. In the elderly, the signs and symptoms of major depression are frequently attributed to “normal aging,” atherosclerosis, Alzheimer’s disease, or any of a host of other age-associated afflictions. Psychosocial antecedents such as loss, combined with decrements in physical health and sensory impairment, can also divert attention from clinical depression.
Another reason for the underdiagnosis is that older patients are less likely to report symptoms of dysphoria and worthlessness, which are often considered hallmarks of the diagnosis of depression. The consequences of underdiagnosis of this subset of patients can be severe. On the basis of a followup of older adults in the Baltimore Epidemiologic Catchment Area sample, persons with depressive symptoms (e.g., sleep and appetite disturbance) without sadness (e.g., hopelessness, worthlessness, thoughts of death, wanting to die, or suicide) were at increased risk for subsequent functional impairment, cognitive impairment, psychological distress, and death over the course of the 13-year interval (Gallo et al., 1997).
Other barriers to diagnosis are patient related. Depression can and frequently does amplify physical symptoms, distracting patients’ and providers’ attention from the underlying depression; and many older patients may deny psychological symptoms of depression or refuse to accept the diagnosis because of stigma. This appears to be particularly the case with older men, who also have the highest rates of suicide in later life (Hoyert et al., 1999).
Provider-related factors also appear to play a role in underdetection of depression and suicide risk. Providers may be reluctant to inform older patients of a diagnosis of depression, owing to uncertainty about diagnosis, reluctance to stigmatize, uncertainty about optimal treatment, concern about medication interactions or lack of access to psychiatric care, and continuing concern about the effectiveness and cost-effectiveness of treatment intervention (NIH Consensus Development Panel on Depression in Late Life, 1992; Unutzer et al., 1997a).
Societal stereotypes about aging also can hamper efforts to identify and diagnose depression in late life. Many people believe that depression in response to the loss of a loved one, increased physical limitations, or changing societal role is an inevitable part of aging. Even physicians appear to hold such stereotyped views. Three-quarters of physicians in one study thought that depression “was understandable” in older persons (Gallo et al., in press), consistent with other studies (Bartels et al., 1997). Suicidal thoughts are sometimes considered a normal facet of old age. These mistaken beliefs can lead to underreporting of symptoms by patients and lack of effort on the part of family members to seek care for patients.
Finally, the health care system itself is increasingly restricting the time spent in patient care, forcing mental health concerns to compete with comorbid general medical conditions. Primary care physicians often report feeling too pressured for time to investigate depression in older people (Glasser & Gravdal, 1997). Given the inseparability of mental and general health in later life particularly, this trend is worrisome.
Across the life span, the course of depression is marked by recurrent episodes of depression followed by periods of remission. In late life, the course of depression tends to be more chronic than that in younger adults (Alexopoulos & Chester, 1992; Callahan et al., 1994; Cole & Bellavance, 1997). This means that recurrences extend for longer duration, while intervals of remission are shorter. It also means that cycles of recurrence and remission persist over a longer period of time. Patients’ response to treatment is highly variable, and the determinants of treatment response and its temporal profile are the subjects of intense research (Reynolds & Kupfer, 1999). A slower, less consistent response, which suggests a higher probability of relapse, is related to older age, presence of acute and chronic stressors, lower levels of perceived social support, higher levels of pretreatment anxiety, and greater biologic dysregulation as reflected in higher levels of rapid eye movement sleep (Dew et al., 1997). The temporal profile of the initial treatment response also may provide important clues about which patients are likely to fare well on maintenance treatment and which ones are likely to have a brittle treatment response and stormy long-term course.
A recent update of the NIH Consensus Development Conference on the Diagnosis and Treatment of Late-Life Depression emphasized the need for more data to guide long-term treatment planning, especially in patients 70 years and older with major depression (Lebowitz et al., 1997). Little is currently known about differences, if any, in speed and rate of remission, relapse, recovery, and recurrence in patients aged 60 to 69 and those aged 70 and above. In a study at the University of Pittsburgh, two groups of patients (ages 60 to 69 and 70+) showed comparable times to remission and recovery, as well as similar absolute rates of remission during acute therapy, relapse during continuation therapy, and recovery. However, patients aged 70 and older experienced a significantly higher rate of recurrence during the first year of maintenance therapy (Reynolds, 1998). Thus, the course of depression and its interaction with treatment are influenced by age. This highlights the importance of research targeted at older age groups instead of reliance on extrapolations from younger patients.
Late-life mental disorders are often detected in association with somatic illness (Reynolds & Kupfer, 1999). The prevalence of clinically significant depression in later life is estimated to be highest—approximately 25 percent—among those with chronic illness, especially with ischemic heart disease, stroke, cancer, chronic lung disease, arthritis, Alzheimer’s disease, and Parkinson’s disease (Borson et al., 1986; Blazer, 1989; Oxman et al., 1990; Callahan et al., 1994; Beekman et al., 1995; Borson, 1995).
The relationship between somatic illness and mental disorders is likely to be reciprocal, but the mechanisms are far from understood. Biological and psychological factors are thought to play a role (Unutzer et al., 1997a). The nature and course of late-life depression can be greatly affected by the coexistence of one or more other medical conditions.
Insomnia and sleep disturbance play a large role in the clinical presentation of older depressed patients. Sleep complaints over time in community-residing older people have been found to vary with the intensity of depressive symptoms (Rodin et al., 1988). Sleep disturbances in older men and women have also been recently linked to poor health, depression, angina, limitations in activities of daily living, and chronic use of benzodiazepines (Newman et al., 1997). Furthermore, persistent or residual sleep disturbance in older patients with prior depressive episodes predicts a less successful maintenance response to pharmacotherapy (Buysse et al., 1996). The prevalence of chronic, primary insomnia in older adults is estimated at 5 to 10 percent (Ohayon et al., 1996). Relatively little is known about the etiology or pathophysiology of chronic primary insomnia and why it constitutes a risk factor for depression in older adults. An important issue for further research is whether effective treatment for chronic insomnia could prevent the subsequent development of clinical depression in midlife and later.
The most serious consequence of depression in later life—especially untreated or inadequately treated depression—is increased mortality from either suicide or somatic illness. Older persons (65 years and above) have the highest suicide rates of any age group. The suicide rate for individuals age 85 and older is the highest, at about 21 suicides per 100,000, a rate almost twice the overall national rate of 10.6 per 100,000 (CDC, 1999). The high suicide rate among older people is largely accounted for by white men, whose suicide rate at age 85 and above is about 65 per 100,000 (CDC, 1999). Trends from 1980 to 1992 reveal that suicide rates are increasing among more recent cohorts of older persons (Kachur et al., 1995). Since national statistics are unlikely to include more veiled forms of suicide, such as nursing home residents who stop eating, estimates are probably conservative.
Suicide in older adults is most associated with late-onset depression: among patients 75 years of age and older, 60 to 75 percent of suicides have diagnosable depression (Conwell, 1996). Using a “psychological autopsy,” Conwell and coworkers investigated all suicides within a geographical region and found that with increasing age, depression was more likely to be unaccompanied by other conditions such as substance abuse (Conwell et al., 1996). While thoughts of death may be developmentally expected in older adults, suicidal thoughts are not. From a stratified sample of primary care patients over age 60, Callahan and colleagues estimated the prevalence of specific suicidal thoughts at 0.7 to 1.2 percent (Callahan et al., 1996b). Unfortunately, no demographic or clinical variables distinguished depressed suicidal patients from depressed nonsuicidal patients (Callahan et al., 1996b).
Swedish researchers found much higher rates of suicidal ideation after interviewing adults aged 85 years and older. They found a 1-month prevalence of any suicidal feelings in 9.6 percent of men and 18.7 percent of women (Skoog et al., 1996). Suicidal feelings were strongly associated with depression. For example, 6.2 percent of the participants who did not meet criteria for depression or anxiety reported suicidal thoughts, while almost 50 percent of those meeting criteria for depression reported such thoughts. The higher prevalence of suicidal feelings in this study, compared with that cited earlier, is likely due to the older age of subjects and to methodological differences.
Studies of older persons who have committed suicide have revealed that older adults had seen their physician within a short interval of completing suicide, yet few were receiving mental health treatment. Caine and coworkers studied the records of 97 adults aged 50 years and older who completed suicide (Caine et al., 1996). Of this group, 51 had seen their primary care physician within 1 month of the suicide. Forty-five had psychiatric symptoms. Yet in only 29 of the 45 individuals were symptoms recognized, in only 19 was treatment offered, and in only 2 of these 19 cases was the treatment rendered considered adequate. Treatment was deemed inadequate if an incorrect medicine (such as a benzodiazepine for severe major depression) or inadequate dose was prescribed. This line of research highlights important opportunities for suicide prevention.
Depression also can lead to increased mortality from other diseases, such as heart disease and possibly cancer. How depression exerts these effects is not yet understood. In nursing home patients, major depression increases the likelihood of mortality by 59 percent, independent of physical health measures (Rovner, 1993). In the case of myocardial infarction, depression elevates mortality risk fivefold (Frasure-Smith et al., 1993, 1995). Depression also has been linked to the onset of cancer, but results have been inconsistent. Yet a new epidemiological study, considered the most compelling to date, finds that chronic depression (lasting an average of about 4 years) raises the risk of cancer by 88 percent in older people (Penninx et al., 1998). Thus, increased understanding of depression in older people may be, literally, a matter of life and death.
The high prevalence of depressive syndromes and symptoms in older adults exacts a large economic toll. Depression as a whole for all age groups is one of the most costly disorders in the United States (Hirschfeld et al., 1997). The direct and indirect costs of depression have been estimated at $43 billion each year, not including pain and suffering and diminished quality of life (Finkelstein et al., 1996). Late-life depression is particularly costly because of the excess disability that it causes and its deleterious interaction with physical health. Older primary care patients with depression visit the doctor and emergency room more often, use more medication, incur higher outpatient charges, and stay longer at the hospital (Callahan et al., 1994; Cooper-Patrick et al., 1994; Callahan & Wolinsky, 1995; Unutzer et al., 1997b).
Despite major advances, the etiology of depression occurring at any age is not fully understood, although biological and psychosocial factors clearly play an important and interactive role.
With respect to late-onset depression, several risk factors have been identified. Persistent insomnia, occurring in 5 to 10 percent of older adults, is a known risk factor for the subsequent onset of new cases of major depression both in middle-aged and older persons (Ford & Kamerow, 1989). Grief following the death of a loved one also is an important risk factor for both major and minor depression. At least 10 to 20 percent of widows and widowers develop clinically significant depression during the first year of bereavement. Without treatment, such depressions tend to persist, becoming chronic and leading to further disability and impairments in general health (Zisook & Shuchter, 1993). A final pathway to late-onset depression, suggested by computed tomography and magnetic resonance imaging studies, may involve structural, neuroanatomic factors. Enlarged lateral ventricles, cortical atrophy, increased white matter hyperintensities, decreased caudate size, and vascular lesions in the caudate nucleus appear to be especially prominent in late-onset depression associated with vascular risk factors (Ohayon et al., 1996; Baldwin & Tomenson, 1995). These findings have generated the vascular hypothesis of late-onset depression; namely, that even in the absence of a clear stroke, disorders that cause vascular damage, such as hypertension, coronary artery disease, and diabetes mellitus, may induce cerebral pathology that constitutes a vulnerability for depression (Alexopoulos et al., 1997; Steffens & Krishnan, 1998).
A broad array of effective treatments, both pharmacological and psychosocial, exists for depression. Despite the pervasiveness of depression and the existence of effective treatments, a substantial fraction of patients receive either no treatment or inadequate treatment, as described earlier. Some of the barriers relate to underdiagnosis, while others relate to treatment where there are patient, provider, and clinical barriers (for more details see Unutzer et al., 1996).
There is consistent evidence that older patients, even the very old, respond to antidepressant medication (Reynolds & Kupfer, 1999). About 60 to 80 percent of older patients respond to treatment, while the placebo response rate is about 30 to 40 percent (Schneider, 1996). These rates are comparable to those in other adults (see Chapter 4). Treatment response is typically defined by a significant reduction—usually 50 percent or greater—in symptom severity. Yet because patients 75 years old and older typically have higher prevalence of medical comorbidity, both they and their physicians are often reluctant to add another medication to an already complex regimen in a frail individual. However, newer antidepressants are less frequently associated with factors contraindicating their use. Moreover, because the very old are also at high risk for adverse medical outcomes of depression and for suicide, treatment may be favored. Despite the availability of effective treatments, a minority of patients properly diagnosed with depression receive adequate dosage and duration of pharmacotherapy, as noted earlier.
In general, pharmacological treatment of depression in older people is similar to that in other adults, but the selection of medications is more complex because of side effects and interactions with other medications for concomitant somatic disorders. Treatment of minor depression is generally the same as treatment for major depression, but there is not a large body of evidence to support this practice. Studies are under way to identify effective pharmacological treatments for minor depression (Lebowitz et al., 1997).
The following paragraphs describe the major classes of medications for treatment of depression in older adults. They focus on side effects and other concerns that distinguish the treatment of depression in older adults from that in younger ones.
Tricyclic antidepressants (TCAs) have been widely used to treat depressed patients of all ages. Alexopoulos and Salzman (1998) reviewed studies of TCAs in older depressed patients and concluded that these compounds are similar in efficacy across the age spectrum, but the side effect profiles differ considerably. Widespread use of the TCAs in older adults is limited by adverse reactions. While anticholinergic effects such as dry mouth, urinary retention, and constipation can be annoying in younger adults, they can lead to severe problems in older adults. For example, constipation can lead to impaction, and dry mouth can prevent the wearing of dentures. The anticholinergic effects of the TCAs may also cause tachycardia or arrhythmias and can further compromise preexisting cardiac disease (Roose et al., 1987; Glassman et al., 1993). Central anticholinergic effects may result in acute confusional states or memory problems in the depressed older adult (Branconnier et al., 1982). Orthostatic hypotension, which may lead to falls and hip fractures, is also a concern when the TCAs are administered. Nevertheless, TCAs are still frequently used in older adults.
Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, paroxetine, and sertraline, whose use is increasing across age groups, may be especially useful in the treatment of late-life depression, because these agents are reported to have fewer anticholinergic and cardiovascular side effects than the TCAs. The more commonly observed side effects with SSRIs include sexual dysfunction and gastrointestinal effects such as nausea, vomiting, and loose stools. Treatment with the SSRIs may also produce insomnia, anxiety, and restlessness. The few studies that have examined the efficacy of these compounds in older adults have shown efficacy similar to the TCAs and fewer side effects (see Small & Salzman, 1998, for a review). While the relative efficacy of SSRIs and TCAs is still debated, SSRIs are easier to prescribe because of simpler dosing patterns and more manageable side effects.
One concern when prescribing the SSRIs in older adults is the potential for drug-drug interactions. This is of clinical importance since older adults commonly receive a large number of medications. The SSRIs vary in their inhibition of the cytochrome p450 family of isoenzymes. Knowledge of these patterns of inhibition in the SSRIs and other medications commonly used in older adults (such as other psychoactive compounds, calcium channel blockers, or warfarin) can help to avoid or minimize interactions. Other newer non-SSRI antidepressants (venlafaxine, bupropion, trazodone, and nefazodone) are often suggested for treating later life depression because their side effects are better tolerated by older adults.
Some compounds that are useful in other individuals may be less useful for treatment of older patients. For example, despite evidence of the efficacy of monamine oxidase inhibitors (see Alexopoulos & Salzman, 1998, for a review), clinical use is often restricted to patients who are refractory to other antidepressant drugs. This is due to potentially life-threatening pharmacodynamic interactions with sympathomimetic drugs or tyramine-containing foods and beverages. The sympathomimetic amines (e.g., phenylpropanolamine and pseudoephedrine) may be present in over-the-counter decongestant products that older patients are prone to self-administer. An additional concern is the risk of orthostatic hypotension, which occurs even at therapeutic doses (Alexopoulos & Salzman, 1998). In addition, bupropion has been shown in older patients to be as effective as TCAs (Branconnier et al., 1983; Kane et al., 1983). Although generally well tolerated, its use requires added caution because of an increased risk of seizures and thus should be avoided in patients with seizure disorder or focal central nervous system disease. Its advantages include a relatively low incidence of cardiovascular complications and a lack of confusion.
Combining pharmacotherapy with psychosocial interventions also appears to be effective in older depressed patients. A high response rate of about 80 percent was found for acute and continuation treatment with combined nortriptyline and interpersonal psychotherapy. The response rate was similar between so-called “young old” patients (primarily in their 60s and early 70s) and patients in their 30s and 40s (Reynolds et al., 1996). Yet older patients showed a somewhat longer time to remission than did other patients (about 2 weeks longer) and twice the rate of relapse during continuation treatment (about 15 percent versus 7 percent). However, because the trial was not controlled, it is not known whether multimodal treatment was more effective than either pharmacological or psychosocial treatment alone. Treatment resistance—defined by the lack of recovery in spite of combined treatment with nortriptyline and interpersonal psychotherapy—was seen in about 18 percent of older patients with recurrent major depression (nonpsychotic unipolar depression) (Little et al., 1998). Nortriptyline and interpersonal psychotherapy (IPT) have been shown to be effective maintenance treatments for late-life depression. After 3 years of comparing various treatments, the percentage of older adults who did not experience recurrence were 57 percent of older adults receiving nortriptyline, 36 percent receiving IPT, and 80 percent of those receiving nortriptyline plus IPT. Those receiving a placebo and routine clinical visits had a 90 percent recurrence rate (Reynolds et al., 1999).
Although 60 to 80 percent of older patients with moderate to severe unipolar2 depression can be expected to respond well to antidepressant treatment (especially combined treatment with medication and psychotherapy), the clinical response to antidepressant treatment in later life follows a variable course, with a median time to remission of 12 weeks (J. L. Cummings & D. J. Kupfer, personal communication, 1999). Thus, treatment response takes 1 month or more longer than that for other adults, for whom treatment response takes an average of 6 to 8 weeks (see Chapter 4). In addition to highly variable trajectories to recovery, reliable prediction of response status (recovery/nonrecovery) is generally not possible in older adults before 4 to 5 weeks of treatment. The delayed onset of antidepressant activity in older adults leads to unique problems. Suffering and disability are prolonged, which often reduces compliance and may increase risk for suicide. The development of strategies to accelerate treatment response and to improve the early identification of nonresponders would be an important advance (Reynolds & Kupfer, 1999).
Data from naturalistic studies have identified several predictors of relapse and recurrence in late-life depression, including a history of frequent episodes, first episode after age 60, concurrent somatic illness, especially a history of myocardial infarction or vascular disease, high pretreatment severity of depression and anxiety, and cognitive impairment, especially frontal lobe dysfunction. These factors appear to interact with low treatment intensity—that is, at dosage and duration below recommended levels—in determining more severe courses of illness. Despite the evidence that high treatment intensity is effective in preventing relapse and recurrence (Reynolds et al., 1995), naturalistic studies have shown that intensity of treatment prescribed by psychiatrists begins to decline within 16 weeks of entry and approximately 10 weeks prior to recovery (Alexopoulos et al., 1996). Residual symptoms of excessive anxiety and worrying predict early recurrence after tapering continuation treatment in older depressed patients (Meyers, 1996).
Although progress has been made in identifying effective pharmacological and combined treatments for late-life depression, there is a need for more outcome studies with newer antidepressants. In addition, studies examining effectiveness in real-world settings—rather than in clinical trials conducted in academic clinical sites—are particularly crucial in the older population because of medical comorbidity and provision of care in primary, rather than specialty, care.
Electroconvulsive therapy (ECT) is regarded as an effective intervention for some forms of treatment-resistant depression across the life cycle (NIH & NIMH Consensus Conference, 1985; Depression Guideline Panel, 1993). It may offer a particularly attractive benefit:risk ratio in older persons with depression (NIH Consensus Development Panel on Depression in Late Life, 1992; Sackeim, 1994). Chapter 4 reviews research on ECT and considers risk-benefit issues and controversy surrounding them. As described there, ECT entails the electrical induction of seizures in the brain, administered during a series of 6 to 12 treatment sessions on an inpatient or outpatient basis. Practice guidelines recommend that ECT should be reserved for severe cases of depression, particularly with active suicidal risk or psychosis; patients unresponsive to medications; and those who cannot tolerate medications (NIH & NIMH Consensus Conference, 1985; Depression Guideline Panel, 1993). For those patients, the response rate to ECT is on the order of 50 to 70 percent, and there is no evidence that ECT is any less effective in older individuals than younger ones (Sackeim, 1994; Weiner & Krystal, 1994). ECT is advantageous for older people with depression because of the special problems they encounter with medications, including sensitivity to anticholinergic toxicity, cardiac conduction slowing, and hypotension (see above). Although the newer antidepressants offer a more favorable side-effect profile than do the older tricyclics, their efficacy in melancholic depression, for which ECT is particularly helpful (Rudorfer et al., 1997), is not yet firmly established. Moreover, as noted earlier, older adults respond more slowly than younger ones to antidepressant medications, rendering the faster onset of action of ECT another advantage in the older patient (Markowitz et al., 1987). Immobility and reduced food and fluid intake in the older person with depression may pose a greater imminent physical health risk than would typically be the case in a younger patient, again strengthening the case for considering ECT early in the treatment hierarchy (Sackeim, 1994).
Although the clinical effectiveness of ECT is documented and acknowledged, the treatment often is associated with troubling side effects, principally a brief period of confusion following administration and a temporary period of memory disruption (Rudorfer et al., 1997). As described in Chapter 4, there may also be longer term memory losses for the time period surrounding the use of ECT. Although the exception rather than the rule, persistent memory loss following ECT is reported. Its actual incidence is unknown. There are no absolute medical contraindications to ECT. However, a recent history of myocardial infarct, irregular cardiac rhythm, or other heart conditions suggests the need for caution due to the risks of general anesthesia and the brief rise in heart rate, blood pressure, and load on the heart that accompany ECT administration. On the other hand, the safety of ECT is enhanced by the time-limited nature of treatment sessions, which enables this intervention to be administered under controlled conditions, for example, with a cardiologist or other specialist in attendance. Following completion of a course of ECT, maintenance treatment, typically with antidepressant or mood-stabilizing medication or less frequent maintenance ECT, in most cases is required to prevent relapse (Rudorfer et al., 1997).
Most research to date on psychosocial treatment of mental disorders has concentrated on depression. These studies suggest that several forms of psychotherapy are effective for the treatment of late-life depression, including cognitive-behavioral therapy, interpersonal psychotherapy, problem-solving therapy, brief psychodynamic psychotherapy, and reminiscence therapy, an intervention developed specifically for older adults on the premise that reflection upon positive and negative past life experiences enables the individual to overcome feelings of depression and despair (Butler, 1974; Butler et al., 1991). Group and individual formats have been used successfully.
A meta-analysis of 17 studies of cognitive, behavioral, brief psychodynamic, interpersonal, reminiscence, and eclectic therapies for late-life depression found treatment to be more effective than no treatment or placebo (Scogin & McElreath, 1994). The following paragraphs spotlight some of the key studies incorporated into this meta-analysis and provide evidence from newer studies.
Cognitive-behavioral therapy is designed to modify thought patterns, improve skills, and alter the emotional states that contribute to the onset, or perpetuation, of mental disorders. In a 2-year followup study of cognitive-behavioral therapy, 70 percent of all patients studied no longer met criteria for major depression and maintained treatment gains (Gallagher-Thompson et al., 1990). In another trial, group cognitive therapy was found to be effective. Older patients with major depression partially randomized to receive group cognitive therapy with alprazolam (a benzodiazepine) or group cognitive therapy with placebo had more improvement in depressed mood and sleep efficiency than patients who received alprazolam alone or placebo alone (Beutler et al., 1987). Cognitive-behavioral therapy also has been demonstrated to be effective in other late-life disorders, including anxiety disorders (Stanley et al., 1996; Beck & Stanley, 1997). Cognitive-behavioral therapy’s effectiveness for mood symptoms in Alzheimer’s disease is discussed in the section on psychosocial treatments of Alzheimer’s disease.
Problem-solving therapy postulates that deficiencies in social problem-solving skills enhance the risk for depression and other psychiatric symptoms. Through improving problem-solving skills, older patients are given the tools to enable them to cope with stressors and thereby experience fewer symptoms of psychopathology (Hawton & Kirk, 1989). Problem-solving therapy has been found effective in the treatment of depression of older patients. For example, problem-solving therapy was found to significantly reduce symptoms of major depression, leading to the greatest improvement in a randomized controlled study comparing problem-solving therapy, reminiscence therapy, and placement on a waiting list for treatment (Arean et al., 1993). In a randomized study of depressed younger primary care patients, six sessions of problem-solving therapy were as effective as amitriptyline, with about 50 to 60 percent of patients in each group recovering (Mynors-Wallis et al., 1995).
Interpersonal psychotherapy was initially designed as a time-limited treatment for midlife depression. It focuses on grief, role disputes, role transitions, and interpersonal deficits (Klerman et al., 1984). This form of treatment may be especially meaningful for older patients given the multiple losses, role changes, social isolation, and helplessness associated with late-life depression. Controlled trials suggest that interpersonal psychotherapy alone, or in combination with pharmacotherapy, is effective in all phases of treatment for late-life major depression. Interpersonal psychotherapy was as effective as the antidepressant nortriptyline in depressed older outpatients, and both were superior to placebo (Sloane et al., 1985; Reynolds et al., 1992; Schneider, 1995). In an open trial, a treatment protocol combining interpersonal psychotherapy with nortriptyline and psychoeducational support groups led to minimal attrition and high remission rates (approximately 80 percent) in older patients with recurrent major depression (Reynolds et al., 1992, 1994). Finally, interpersonal psychotherapy also is effective in the treatment of depression following bereavement (Pasternak et al., 1997).
Brief psychodynamic therapy, typically of 3 to 4 months’ duration, also is successful in older depressed patients. Brief psychodynamic therapy is distinguished from traditional psychodynamic therapy primarily by duration of treatment. The goals of brief psychodynamic therapy vary according to patients’ medical health and function. In disabled older people, the purpose of psychodynamic psychotherapy is to facilitate mourning of lost capacities, promote acceptance of physical limitations, address fears of dependency, and promote resolution of interpersonal difficulties with family members (Lazarus & Sadavoy, 1996). In older patients who are not disabled, psychodynamic psychotherapy deals with the resolution of interpersonal conflicts, adaptation to loss and stress, and the reconciliation of personal accomplishments and disappointments (Pollock, 1987). Brief psychodynamic therapy has been found to be as effective as cognitive-behavioral therapy in reducing symptoms of late-life major depression. An early study found brief psychodynamic therapy to yield higher relapse and recurrence rates than did cognitive and behavioral therapy (Gallagher & Thompson, 1982). However, with a greater number of patients, brief psychodynamic therapy was determined to be as effective as cognitive and behavioral therapy (and superior to being on a waiting list) in preventing recurrences of major depression up to 2 years after treatment (Gallagher-Thompson et al., 1990).
Alzheimer’s disease, a disorder of pivotal importance to older adults, strikes 8 to 15 percent of people over the age of 65 (Ritchie & Kildea, 1995). Alzheimer’s disease is one of the most feared mental disorders because of its gradual, yet relentless, attack on memory. Memory loss, however, is not the only impairment. Symptoms extend to other cognitive deficits in language, object recognition, and executive functioning.3 Behavioral symptoms—such as psychosis, agitation, depression, and wandering—are common and impose tremendous strain on caregivers. Diagnosis is challenging because of the lack of biological markers, insidious onset, and need to exclude other causes of dementia.
This section covers assessment and diagnosis, behavioral symptoms, course, prevalence and incidence, cost, etiology, and treatment. It features Alzheimer’s disease because it is the most prevalent form of dementia. However, many of the issues raised also pertain to other forms of dementia, such as multiinfarct dementia, dementia of Parkinson’s disease, dementia of Huntington’s disease, dementia of Pick’s disease, frontal lobe dementia, and others.
Declines in cognitive functioning have been identified both as part of the normal process of aging and as an indicator of Alzheimer’s disease. DSM-IV first designated this as “age-related cognitive decline” and, more recently, as “mild cognitive impairment” (MCI). MCI characterizes those individuals who have a memory problem but do not meet the generally accepted criteria for Alzheimer’s disease such as those issued by the National Institute of Neurological and Communicative Disorders and Stroke–Alzheimer’s Disease and Related Disorders Association or DSM-IV. MCI is important because it is known that a certain percentage of patients will convert to Alzheimer’s disease over a period of time (probably in the range of 15 to 20 percent per year). Thus, if such individuals could be identified reliably, treatments could be given that would delay or prevent the progression to diagnosed Alzheimer’s disease. This is the rationale for the Alzheimer’s Disease Cooperative Study trial of vitamin E or donepezil for MCI, which began in 1999, and it is also the basis for the use of neuroimaging in early diagnosis. The evaluation of MCI spans the boundary between normal aging and Alzheimer’s disease, and this topic is being evaluated in a number of research groups.
The diagnosis of Alzheimer’s disease depends on the identification of the characteristic clinical features and on the exclusion of other common causes of dementia. There are currently no biological markers for Alzheimer’s disease except for pathological verification by biopsy or at autopsy (or through rare autosomal dominant mutations). With the reliance on clinical criteria and the need for exclusion of other causes of dementia, the current approach to Alzheimer’s disease diagnosis is time- and labor-intensive, costly, and largely dependent on the expertise of the examiner. Although genetic risk factors, such as Apo-E status (see etiology section), give some indication of the relative risk for Alzheimer’s disease, they are as yet rarely useful on an individual basis.
The diagnosis of Alzheimer’s disease not only requires the presence of memory impairment but also another cognitive deficit, such as language disturbance or disturbance in executive functioning. The diagnosis also calls for impairments in social and occupational functioning that represent a significant functional decline (DSM-IV). The other causes of dementia that must be ruled out include cerebrovascular disease, Parkinson’s disease, Huntington’s disease, subdural hematoma, normal-pressure hydrocephalus, brain tumor, systemic conditions (e.g., hypothyroidism, vitamin B12 or folic acid deficiency, niacin deficiency, hypercalcemia, neurosyphilis, HIV infection), and substance-induced conditions.
Some diagnostic schemes distinguish between possible, probable, and definite Alzheimer’s disease (McKhann et al., 1984). With these criteria, probable Alzheimer’s disease is confirmed to be Alzheimer’s disease at autopsy with 85 to 90 percent accuracy (Galasko et al., 1994). Definite Alzheimer’s disease can only be diagnosed pathologically through biopsy or at autopsy. The pathological hallmarks of Alzheimer’s disease are neurofibrillary tangles (intracellular aggregates of a cytoskeletal protein called tau found in degenerating or dead brain cells) and neuritic plaques (extracellular deposits largely made up of a protein called amyloid -peptide) (Cummings, 1998b). (See Figure 5-2.)
The diagnosis of dementia can be complicated by the possibility of other disorders that coexist with, or share features of, Alzheimer’s disease. For example, delirium is a common condition in older patients and can be confused with dementia in its acute stages. Other types of dementia, such as vascular dementia, share cognitive and behavioral symptoms with Alzheimer’s disease, and thus may be difficult to distinguish from Alzheimer’s disease. The cognitive symptoms of early Alzheimer’s disease and those associated with normal age-related decline also may be similar. Finally, cognitive deficits are prominent in both late-life depression and schizophrenia. While the severity of deficits is less in these disorders than that in later stages of dementia, distinctions may be difficult if the dementia is early in its course.
A further challenge in the identification of Alzheimer’s disease is the widespread societal view of “senility” as a natural developmental stage. Early symptoms of cognitive decline may be excused away or ignored by family members and the patient, making early detection and treatment difficult. The clinical diagnosis of Alzheimer’s disease relies on an accurate history of the patient’s symptoms and rate of decline. Such information is often impossible to obtain from the patient due to the prominence of memory dysfunction. Family members or other informants are usually helpful, but their ability to provide useful information sometimes is hampered by denial or lack of knowledge about signs and symptoms of the disorder.
With diagnosis so challenging, Alzheimer’s disease and other dementias are currently underrecognized, especially in primary care settings, where most older patients seek care. In a study in the United Kingdom, O’Connor and colleagues found that general practitioners recognized only 58 percent of patients identified by research psychiatrists using a structured diagnostic interview (O’Connor et al., 1988). Similarly, in a study conducted in the United States, Callahan and colleagues found that only 3.2 percent of patients with mild cognitive impairment were recognized by general practitioners as having intellectual compromise, and only 23.5 percent of those with moderate to severe dementia were identified as having a dementia syndrome (Callahan et al., 1995). The reasons for primary care provider difficulty with diagnosis are speculated to include lack of knowledge or skills, misdiagnosis of depression as dementia, lack of time, and lack of adequate referrals to specialty mental health care.
The urgency of addressing obstacles to recognition and accurate diagnosis is underscored by promising studies that point to the pronounced clinical advantages of early detection. Therapies that slow the progression of Alzheimer’s disease or improve existing symptoms are likely to be most effective if given early in the clinical course. Recognition of early Alzheimer’s disease, in addition to facilitating pharmacotherapy, has a variety of other benefits that improve the plight of patients and their families. Direct benefits to patients include improved diagnosis of other potentially reversible causes of dementia, such as hypothyroidism, and identification of sources of Alzheimer’s disease’s excess disability such as depression and anxiety that can be targeted with nonpharmacological interventions. Family members benefit from early detection by having more time to adjust and plan for the future and by having the opportunity for greater patient input into decisions regarding advanced directives while the patient is still at a mild stage of the illness (Cummings & Jeste, 1999).
Diagnosis of Alzheimer’s disease would be greatly improved by the discovery of a biological marker that correlates strongly with neuropathological signs of Alzheimer’s disease, reflects the severity of pathological changes in Alzheimer’s disease, and precedes the appearance of clinical symptomatology. Ideally, such a marker also would be used to monitor the effectiveness of treatment on the clinical manifestations of Alzheimer’s disease, would show specificity for Alzheimer’s disease with few false positives (i.e., a diagnosis of Alzheimer’s disease in someone who does not have the disease), and would be convenient and inexpensive enough to justify wide use, including screening (Cummings & Jeste, 1999). Discovery of such a marker is clearly a research priority.
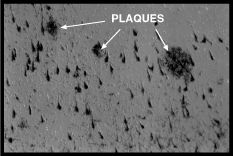 |
| Figure 5-2. Neuritic plaques and many neurofibrillary tangles in the hippocampus of an Alzheimer’s disease patient. |
Alzheimer’s disease is associated with a range of symptoms evident in cognition and other behaviors; these include, most notably, psychosis, depression, agitation, and wandering. Other behavioral symptoms of Alzheimer’s disease include insomnia; incontinence; catastrophic verbal, emotional, or physical outbursts; sexual disorders; and weight loss. Behavioral symptoms, however, are not required for diagnosis. While behavioral symptoms have received less attention than cognitive symptoms, they have serious ramifications: patient and caregiver distress, premature institutionalization, and significant compromise of the quality of life of patients and their families (Rabins et al., 1982; Ferris et al., 1987; Finkel et al., 1996; Kaufer et al., 1998). Alzheimer’s disease, especially behavioral symptoms, appears to place patients at risk for abuse by caregivers (Coyne et al., 1993).
Behavioral symptoms occur at some point during the disease with high frequencies: 30 to 50 percent of individuals with Alzheimer’s disease experience delusions, 10 to 25 percent have hallucinations, and 40 to 50 percent have symptoms of depression (Mega et al., 1996; Cummings et al., 1998b). Patients with psychotic disorders have greater cognitive impairment, more rapidly progressive dementia, and greater frontal and temporal dysfunction on functional brain imaging (Jeste et al., 1992; Sultzer et al., 1995). Patients with psychotic illness also exhibit more agitation, depression, wandering, anger, personality change, family or marital problems, and lack of self-care (Rockwell et al., 1994). Depression in patients with Alzheimer’s disease accelerates loss of functioning in everyday activities (Ritchie et al., 1998). Even modest reduction in behavioral symptoms can produce substantial improvements in functioning and quality of life.
Patients with Alzheimer’s disease experience a gradual decline in functioning throughout the course of their illness. Typically, a loss of 4 points per year on the Mini Mental Status Exam is detected, but there is a great deal of heterogeneity in the rate of decline (Olichney et al., 1998). Memory dysfunction is not only the most prominent deficit in dementia but also is the most likely presenting symptom. Deficits in language and executive functioning, while common in the disorder, tend to manifest later in its course (Locascio et al., 1995). Depression is prevalent in the early stages of dementia and appears to recede with functional decline (Locascio et al., 1995). Although this may reflect decreasing awareness of depression by the patient, it also could reflect inadequate detection of depression by health professionals. Behavioral symptoms, such as agitation, seem to be more prevalent in the later stages of Alzheimer’s disease (Patterson & Bolger, 1994); however, psychosis has been observed in patients with varying levels of severity (Borson & Raskind, 1997). The duration of illness, from onset of symptoms to death, averages 8 to 10 years (DSM-IV).
Alzheimer’s disease is a prominent disorder of old age: 8 to 15 percent of people over age 65 have Alzheimer’s disease (Ritchie & Kildea, 1995). The prevalence of dementia (most of which is accounted for by Alzheimer’s disease) nearly doubles with every 5 years of age after age 60 (Jorm et al., 1987). Although more women than men have Alzheimer’s disease (that is, the prevalence of the disease appears to be higher among women), this may reflect women’s longer life spans, because studies do not show marked gender differences in incidence rates (Lebowitz et al., 1998). Incidence studies also reveal age-related increases in Alzheimer’s disease (Breteler et al., 1992; Paykel et al., 1994; Hebert et al., 1995; Johansson & Zarit, 1995; Aevarsson & Skoog, 1996). One percent of those age 60 to 64 are affected with dementia; 2 percent of those age 65 to 69; 4 percent of those age 70 to 74; 8 percent of those 75 to 79; 16 percent of those age 80 to 84; and 30 to 45 percent of those age 85 and older (Jorm et al., 1987; Evans et al., 1989).
The “graying of America” is likely to result in an increase in the number of individuals with Alzheimer’s disease, yet shifts in the composition of the affected population also are anticipated. Increased education is correlated with a lower frequency of Alzheimer’s disease (Hill et al., 1993; Katzman, 1993; Stern et al., 1994), and future cohorts are expected to have attained greater levels of education. For example, the portion of those currently 75 years of age and older—those most vulnerable to Alzheimer’s disease—with at least a high school education is 58.7 percent. Of those currently age 60 to 64 who will enter the period of maximum vulnerability by the year 2010, 75.5 percent have at least a high school education. A higher educational level among the at-risk cohort may delay the onset of Alzheimer’s disease and thereby decrease the overall frequency of Alzheimer’s disease (by decreasing the number of individuals who live long enough to enter the period of maximum vulnerability). However, this trend may be counterbalanced or overtaken by greater longevity and longer survival of affected individuals. Specifically, improvements in general health and health care may lengthen the survival of dementia patients, increasing the number of severely affected patients and raising their level of medical comorbidity. Similarly, through dissemination of information to patients and clinicians, better detection, especially of early-stage patients, is expected. Increased use of putative protective agents, such as vitamin E, also may increase the number of patients in the middle phases of the illness (Cummings & Jeste, 1999).
The growing number of patients with Alzheimer’s disease is likely to have serious public health and economic consequences. Direct and indirect costs for medical and long-term care, home care, and loss of productivity for caregivers are estimated at nearly $100 billion each year (Ernst & Hay, 1994; National Institute on Aging, 1996). This economic burden is borne mostly by families of patients with Alzheimer’s disease, although a significant portion of the direct costs is covered by Medicare, Medicaid, and private insurance companies. Costs are especially high among patients with behavioral symptoms, who often require earlier or more frequent institutionalization (Ferris et al., 1987).
The etiology of Alzheimer’s disease is still incompletely understood yet is thought to entail a complex combination of genetic and environmental factors. Genetic factors appear to play a significant role in the pathogenesis of Alzheimer’s disease. In the familial form, Alzheimer’s disease is caused by mutations in chromosomes 21, 14, and 1 and is transmitted in an autosomal dominant mode. Each of these mutations appears to result in overproduction of the protein found in neuritic plaques, B amyloid. Onset of the familial form is usually early, but the course and nature of the disorder appear to be influenced by environmental factors (Cummings et al., 1998b). However, the familial form accounts for only a small proportion of cases of Alzheimer’s disease (less than 5 percent) (Cummings et al., 1998b).
Approximately 50 percent of individuals with a family history of Alzheimer’s disease, if followed into their 80s and 90s, develop the disorder (Mohs et al., 1987). Certain genotypes (the pattern of genetic inheritance in an individual) appear to confer risk for the more common late-onset form of Alzheimer’s disease. For example, the ApoE-e4 allele4 on chromosome 19, which increases the deposition of B amyloid, has been shown to increase risk for developing Alzheimer’s disease (Corder et al., 1993). Other possible candidate genes are under study (Kang et al., 1997).
Other biological risk factors for the development of Alzheimer’s disease include aging and cognitive capacities (Cummings et al., 1998b). The mechanisms by which these traits confer increased risk have not yet been fully determined; however, several neurobiologic changes related to normal aging of the brain may play a role in the increased risk for Alzheimer’s disease with increasing age. These include neuron and synaptic loss, decreased dendritic span, decreased size and density of neurons in the nucleus basalis of Meynert, and lower cortical acetylcholine levels (Cummings et al., 1998b). These findings, as well as extrapolations from the prevalence and incidence curves for Alzheimer’s disease, have led some to suggest that most individuals would eventually develop Alzheimer’s disease if the human life span was extended (for example, to age 120).
Several protective factors that delay the onset of Alzheimer’s disease have been identified. Genetic endowment with the ApoE-e2 allele decreases the risk for Alzheimer’s disease (Duara et al., 1996), although the mechanism of action is not yet fully understood. Higher educational level also is related to delayed onset of Alzheimer’s disease (Stern et al., 1994; Callahan et al., 1996a). The use of certain medications, such as nonsteroidal anti-inflammatory drugs (Andersen et al., 1995; McGeer et al., 1996) and estrogen replacement therapy (Paganini-Hill & Henderson, 1994), may delay onset of the disorder. Vitamin E and the drug selegiline (also known as deprenyl) appear to delay the occurrence of important milestones in the course of Alzheimer’s disease, including nursing home placement, severe functional impairments even as the disease progresses, and death (Sano et al., 1997).
The mechanism of action of these protective agents is not fully understood but is thought to counter the deleterious action of oxidative stress (via antioxidants such as vitamin E or estrogen) (Behl et al., 1995) or the action of inflammatory mediators associated with plaque formation (via anti-inflammatories) (Mrak et al., 1995).
The pathophysiology of Alzheimer’s disease appears to be linked to the histopathologic changes in Alzheimer’s disease, which include neuritic plaques, neurofibrillary tangles, synaptic loss, hippocampal granulovacuolar degeneration, and B amyloid angiopathy. Most of the genetic and epigenetic risk factors have been related in some way to B amyloid. Thus, the generation of B amyloid peptide is increasingly regarded as the central pathological event in Alzheimer’s disease (Cummings et al., 1998b; Hardy & Higgins, 1992).
Effective intervention for Alzheimer’s disease may involve interfering with the multiple steps within the putative Alzheimer’s disease pathogenetic cascade. Targets of intervention include reducing B amyloid generation from the amyloid precursor protein, decreasing B amyloid aggregation and formation of beta-pleated sheets, and interfering with amyloid-related neurotoxicity. In addition, therapies could involve interruption of neuronal cell death, inhibition of the inflammatory response occurring in neuritic plaques, use of growth factors and hormonal therapies, and replenishment of deficient neurotransmitters. Because complete blockade of steps within the B amyloid cascade may interfere with normal cerebral metabolic processes, efficacious interventions could involve partial interruptions (Cummings & Jeste, 1999).
Researchers in the molecular neuroscience of Alzheimer’s disease are exploring a number of important aspects of pathophysiology and etiology. As understanding of mechanisms of cell death and neuronal degeneration increases, new opportunities for the development of therapeutics are expected to emerge (National Institute on Aging, 1996).
Loss of the neurotransmitter acetylcholine also is thought to play an instrumental role in the pathogenesis of Alzheimer’s disease. Postmortem studies of Alzheimer’s disease consistently have demonstrated the loss of basal forebrain and cortical cholinergic neurons and the depletion of choline acetyltransferase, the enzyme responsible for acetylcholine synthesis (Mesulam, 1996). The degree of this central cholinergic deficit is correlated with the severity of dementia, which has led to the “cholinergic hypothesis” of cognitive deficits in Alzheimer’s disease. This hypothesis has led, in turn, to promising clinical interventions discussed below. It should be emphasized, however, that acetylcholine is not necessarily the only neurotransmitter involved in Alzheimer’s disease; research has not ruled out the contributions of other substances in pathogenesis of the disease.
Pharmacological treatment of Alzheimer’s disease is a promising new focus for interventions. A delay in onset of Alzheimer’s disease for 5 years might reduce the prevalence of Alzheimer’s disease by as much as one-half (Breitner, 1991). In other words, to influence the prevalence of Alzheimer’s disease, it may be necessary only to delay the onset of the disease to the point where mortality from other sources supersedes the incidence of Alzheimer’s disease. Thus, a central goal in Alzheimer’s disease treatment research is the identification of agents that prevent the occurrence, defer the onset, slow the progression, or improve the symptoms of Alzheimer’s disease. Progress has been made in this research arena, with several agents showing beneficial effects in Alzheimer’s disease.
Recent attempts to treat Alzheimer’s disease have focused on enhancing acetylcholine function, using either cholinergic receptor agonists (e.g., nicotine) or, most commonly, using acetylcholinesterase (AChE) inhibitors (e.g., physostigmine, velnacrine, tacrine, donepezil, or metrifonate) to increase the availability of acetylcholine in the synaptic cleft. Such treatments have generally been beneficial in ameliorating global cognitive dysfunction and, more specifically, are most effective in improving attention (Norberg, 1996; Lawrence & Sahakian, 1998). Amelioration of learning and memory impairments, the most prominent cognitive deficits in Alzheimer’s disease, have been found less consistently (Lawrence & Sahakian, 1998), although some studies have shown improvements (Thal, 1996). It has been argued that failure of AChE inhibitors and nicotine to improve learning and memory may be due to high levels of neurodegeneration in the medial temporal lobe (Lawrence & Sahakian, 1998). Neuronal degeneration in this region of the brain leaves neurons impervious to the benefits of some types of replacement therapy. Detailed neuropsychological studies of the effects of the newer cognitive enhancers, donepezil and metrifonate (an experimental drug), have not yet been published, but global cognitive functioning appears to be improved with both compounds (Cummings et al., 1998a; Rogers et al., 1998). Treatment with these AChE inhibitors also appears to benefit noncognitive symptoms in Alzheimer’s disease, such as delusions (Raskind et al., 1997) and behavioral symptoms (Kaufer et al., 1996; Morris et al., 1998).
The behavioral symptoms of Alzheimer’s disease have received less therapeutic attention than cognitive symptoms. Few double-blind, placebo-controlled studies of medications for behavioral symptoms of Alzheimer’s disease have been performed. For the most part, behavioral symptoms have been treated with medications developed for primary psychiatric symptoms. The emergence of new antipsychotic and antidepressant medications requires that these agents be studied specifically for Alzheimer’s disease. The observation that cholinergic agents used to enhance cognition in Alzheimer’s disease may have beneficial behavioral effects also needs further exploration (Kaufer et al., 1996; Bodick et al., 1997; Raskind et al., 1997).
One area that has been studied is the treatment of depression in Alzheimer’s disease. Treatment with the antidepressants paroxetine and imipramine has been shown to be effective in depressed Alzheimer’s disease patients (Reifler et al., 1989; Katona et al., 1998). Treatment may not only be effective for relieving depressive symptoms but also for its potential to improve functional ability (Pearson et al., 1989; Ritchie et al., 1998).
Several challenges are encountered with the pharmacological treatment of Alzheimer’s disease. First, because of the cognitive deficits that are the hallmark of dementia, caregiver assistance is crucial for compliance with pharmacotherapy regimens. Second, although the current pharmacotherapies are likely to be most useful if administered early in the course of the disorder, early detection of Alzheimer’s disease is encumbered by the lack of a verified biological or biobehavioral marker. Third, little is currently known about the optimal duration of treatment with pharmacotherapies.
Psychosocial interventions are extremely important in Alzheimer’s disease. Although there has been some research on preserving cognition, most research has focused on treating patients’ behavioral symptoms and relieving caregiver burden. Support for caregivers is crucial because caregivers of older patients are at risk for depression, anxiety, and somatic problems (Light & Lebowitz, 1991). Psychosocial interventions targeted either at patients or family caregivers can improve outcomes for patients and caregivers alike.
Psychosocial techniques developed for use in patients with cognitive impairment may be helpful in Alzheimer’s disease. Strengthening ways to deal with cognitive losses may reduce functional limitations for patients with the early stages of Alzheimer’s disease, before multiple brain systems become compromised. For example, training in the use of memory aids, such as mnemonics, computerized recall devices, or copious use of notetaking, may assist patients with mild dementia. While initial research on the use of cognitive rehabilitation in dementia is promising, further studies are needed (Pliskin et al., 1996).
Of the behavioral symptoms experienced by patients with Alzheimer’s disease, depression and anxiety occur most frequently during the early stages of dementing disorders, whereas psychotic symptoms and aggressive behavior occur during later stages (Alexopoulos & Abrams, 1991; Devanand et al., 1997). Early evidence suggested that cognitive and behavioral therapies are beneficial in treating depressed older patients with dementia (Teri & Gallagher-Thompson, 1991; Teri & Uomoto, 1991). Cognitive therapy, seen as more promising for the early stages of dementia, strives to help patients cope with depression by reducing cognitive distortions and by fostering more adaptive perceptions. Behavioral therapy, seen as more promising for more moderately or severely affected adults with dementia, targets family caregivers directly—and patients indirectly—by helping caregivers identify, plan, and increase pleasant activities for the patient, such as taking a walk, designed to improve their mood (Teri & Gallagher-Thompson, 1991).
Further affirmation for behavioral therapy for depression of patients with Alzheimer’s disease recently was provided by a controlled clinical trial. The trial compared two types of behavioral therapy with a typical care condition and a waiting list control. One of the behavioral therapies targeted family caregivers to help them increase pleasant events for the patients, while the other gave caregivers more latitude in choosing which behavioral problem-solving strategies to deal with patients’ depression. Both behavioral therapies led to significant improvement in patients’ depressive symptoms. Moreover, the caregivers also showed significant improvement in their own depressive symptoms (Teri et al., 1997).
For alleviating caregiver and family distress, a broad array of psychosocial interventions was assessed in a meta-analysis of 18 studies (Knight et al., 1993). The interventions included psychoeducation, support, cognitive-behavioral techniques, self-help, and respite care. Individual and respite programs were found moderately effective at reducing caregiver burden and dysphoria, but group interventions were only marginally effective. Subsequent research buttressed the utility of adult day care in reducing caregivers’ stress and depression and in enhancing their well-being (Zarit et al., 1998). Beyond direct benefits to caregivers, support interventions also have benefited patients and have saved resources. For example, a psychosocial intervention—individual and family counseling plus support group participation—aimed at caregiving spouses was shown to delay institutionalization of patients with dementia by almost a year in a randomized trial (Mittelman et al., 1993, 1996). Targeted behavioral techniques also improved the quality of caregivers’ sleep (McCurry et al., 1996), whereas psychoeducation and family support appeared to promote better patient management (Zarit et al., 1985).
The virtues of psychosocial interventions also extend to patients with Alzheimer’s disease in nursing homes. Until the late 1980s, nursing homes employed restraints and sedatives and other medications to control behavioral symptoms in patients with dementia. But the untoward consequences, in terms of injuries from physical restraints and increased patient disorientation, led to nursing home reform practices required by the Federal Nursing Home Reform Act of the Omnibus Budget Reconciliation Act of 1987 (Cohen & Cairl, 1996). In the past few years, a range of behavioral interventions for nursing home staff has been shown to be effective in improving behavioral symptoms of Alzheimer’s disease, such as incontinence (Burgio et al., 1990; Schnelle et al., 1995), dressing problems (Beck et al., 1997), and verbal agitation (Burgio et al., 1996; Cohen-Mansfield & Werner, 1997). A major problem is that interventions are not maintained or implemented correctly by nursing home staff (Schnelle et al., 1998). New approaches seek to teach and maintain behavior management skills of nursing home assistants through a formal staff management system (Barinaga, 1998; Stevens et al., 1998).
Anxiety symptoms and syndromes are important but understudied conditions in older adults. Overall, community-based prevalence estimates indicate that about 11.4 percent of adults aged 55 years and older meet criteria for an anxiety disorder in 1 year (Flint, 1994; Table 5-1). Phobic anxiety disorders are among the most common mental disturbances in late life according to the ECA study (Table 5-1). Prevalence studies of panic disorder (0.5 percent) and obsessive-compulsive disorder (1.5 percent) in older samples reveal low rates (Table 5-1) (Copeland et al., 1987a; Copeland et al., 1987b; Bland et al., 1988; Lindesay et al., 1989). Although the National Comorbidity Study did not cover this age range, and the ECA did not include this disorder, other studies showed a prevalence of generalized anxiety disorder in older adults ranging from 1.1 percent to 17.3 percent higher than that reported for panic disorder or obsessive-compulsive disorder (Copeland et al., 1987a; Skoog, 1993). Worry or “nervous tension,” rather than specific anxiety syndromes, may be more important in older people. Anxiety symptoms that do not fulfill the criteria for specific syndromes are reported in up to 17 percent of older men and 21 percent of older women (Himmelfarb & Murrell, 1984).
In addition, some disorders that have received less study in older adults may become more important in the near future. For example, post-traumatic stress disorder (PTSD) is expected to assume increasing importance as Vietnam veterans age. At 19 years after combat exposure, this cohort of veterans has been found to have a PTSD prevalence of 15 percent (cited in McFarlane & Yehuda, 1996). As affected patients age, there is a continuing need for services. In addition, research has shown that PTSD can manifest for the first time long after the traumatic event (Aarts & Op den Velde, 1996), raising the specter that even more patients will be identified in the future.
The effectiveness of benzodiazepines in reducing acute anxiety has been demonstrated in younger and older patients, and no differences in the effectiveness have been documented among the various benzodiazepines. Some research suggests that benzodiazepines are marginally effective at best in treating chronic anxiety in older patients (Smith et al., 1995).
The half-life of certain benzodiazepines and their metabolites may be significantly extended in older patients (particularly for the compounds with long half-life). If taken over extended periods, even short-acting benzodiazepines tend to accumulate in older individuals. Thus, it is generally recommended that any use of benzodiazepines be limited to discrete periods (less than 6 months) and that long-acting compounds be avoided in this population. On the other hand, use of short-acting compounds may predispose older patients to withdrawal symptoms (Salzman, 1991).
Side effects of benzodiazepines may include drowsiness, fatigue, psychomotor impairment, memory or other cognitive impairment, confusion, paradoxical reactions, depression, respiratory problems, abuse or dependence problems, and withdrawal reactions. Benzodiazepine toxicity in older patients includes sedation, cerebellar impairment (manifested by ataxia, dysarthria, incoordination, or unsteadiness), cognitive impairment, and psychomotor impairment (Salzman, 1991). Psychomotor impairment from benzodiazepines can have severe consequences, leading to impaired driver skills and motor vehicle crashes (Barbone et al., 1998) and falls (Caramel et al., 1998).
Buspirone is an anxiolytic (antianxiety) agent that is chemically and pharmacologically distinct from benzodiazepines. Controlled studies with younger patients suggest that the efficacy of buspirone is comparable to that of the benzodiazepines. It also has proven effective in studies of older patients (Napoliello, 1986; Robinson et al., 1988; Bohm et al., 1990). On the other hand, buspirone may require up to 4 weeks to take effect, so initial augmentation with another antianxiety medication may be necessary for some acutely anxious patients (Sheikh, 1994). Significant adverse reactions to buspirone are found in 20 to 30 percent of anxious older patients (Napoliello, 1986; Robinson et al., 1988). The most frequent side effects include gastrointestinal symptoms, dizziness, headache, sleep disturbance, nausea/vomiting, uneasiness, fatigue, and diarrhea. Still, buspirone may be less sedating than benzodiazepines (Salzman, 1991; Seidel et al., 1995).
Although the efficacy of antidepressants for the treatment of anxiety disorders in late life has not been studied, current patterns of practice are informed by the efficacy literature in adults in midlife (see Chapter 4).
Although schizophrenia is commonly thought of as an illness of young adulthood, it can both extend into and first appear in later life. Diagnostic criteria for schizophrenia are the same across the life span, and DSM-IV places no restrictions on age of onset for a diagnosis to be made. Symptoms include delusions, hallucinations, disorganized speech, disorganized or catatonic behavior (the so-called “positive” symptoms), as well as affective flattening, alogia, or avolition5 (the so-called “negative” symptoms). Symptoms must cause significant social or occupational dysfunction, must not be accompanied by prominent mood symptoms, and must not be uniquely associated with substance use.
One-year prevalence of schizophrenia among those 65 years or older is reportedly only around 0.6 percent, about one-half the 1-year prevalence of the 1.3 percent that is estimated for the population aged 18 to 54 (Tables 5-1 and 4-1).
The economic burden of late-life schizophrenia is high. A study using records from a large California county found the mean cost of mental health service for schizophrenia to be significantly higher than that for other mental disorders (Cuffel et al., 1996); the mean expenditure among the oldest patients with schizophrenia (> 74 years old) was comparable to that among the youngest patients (age 18 to 29). While long-term studies have shown that use of nursing homes, state hospitals, and general hospital care by patients with all mental disorder diagnoses has declined in recent decades, the rate of decline is lower for older patients with schizophrenia (Kramer et al., 1973; Redick et al., 1977). The high cost of these settings contributes to the greater economic burden associated with late-life schizophrenia.
Studies have compared patients with late onset (age at onset 45 years or older) and similarly aged patients with earlier onset of schizophrenia (Jeste et al., 1997); both were very similar in terms of genetic risk, clinical presentation, treatment response, and course.
Among key differences between the groups, patients with late-onset schizophrenia were more likely to be women in whom paranoia was a predominant feature of the illness. Patients with late-onset schizophrenia had less impairment in the specific neurocognitive areas of learning and abstraction/cognitive flexibility and required lower doses of neuroleptic medications for management of their psychotic symptoms. These and other differences between patients with early- and late-onset illness suggest that there might be neurobiologic differences mediating the onset of symptoms (DeLisi, 1992; Jeste et al., in press).
The original conception of “dementia praecox,” the early term for schizophrenia, emphasized progressive decline (Kraepelin, 1971); however, it now appears that Kraepelin’s picture captures the outcome for a small percentage of patients, while one-half to two-thirds significantly improve or recover with treatment and psychosocial rehabilitation (Chapter 4). Although the rates of full remission remain unclear, some patients with schizophrenia demonstrate remarkable recovery after many years of chronic dysfunction (Nasar, 1998). Research suggests that a factor in better long-term outcome is early intervention with antipsychotic medications during a patient’s first psychotic episode (see Chapter 4).
A recent cross-sectional study that compared middle-aged with older patients, all of whom lived in community settings, found some similarities and differences (Eyler-Zorrilla et al., 1999). The older patients experienced less severe symptoms overall and were on lower daily doses of neuroleptics than middle-aged patients who were similar in demographic, clinical, functional, and broad cognitive measures. In addition, positive symptoms were less prominent (or equivalent) in the older group, depending on the measure used. Negative symptoms were more prominent (or equivalent) in the older group, and older patients scored more poorly on severity of dyskinesia. Older patients were impaired relative to middle-aged ones on two measures of global cognitive function. This finding, however, appeared to reflect a normal degree of decline from an impaired baseline, as the degree of change in cognitive function with age in the patient group was equivalent to that seen in the comparison group.
A recent study used the Direct Assessment of Functional Status scale (DAFS) (Loewenstein et al., 1989) to compare the everyday living skills of middle-aged and older adults with schizophrenia with those of people without schizophrenia of similar ages (Klapow et al., 1997). The patients exhibited significantly more functional limitations than the controls did across most DAFS subscales. In another recent study that used a measure of overall disease impact, the Quality of Well-Being Scale, older outpatients with schizophrenia manifested significantly lower quality of well-being than did comparison subjects, and their scores were slightly worse than those of ambulatory AIDS patients (Patterson et al., 1996).
Thus, while schizophrenia may be less universally deteriorating than previously has been assumed, older patients with the disorder continue nonetheless to exhibit functional deficits that warrant research and clinical attention.
Recent studies support a neurodevelopmental view of late-onset schizophrenia (Jeste et al., 1997). Equivalent degrees of childhood maladjustment have been found in patients with late-onset schizophrenia and early-onset schizophrenia, for example, suggesting that some liability for the disorder exists early in life. Equivalent degrees of minor physical anomalies in patients with late-onset schizophrenia and early-onset schizophrenia suggest the presence of developmental defects in both groups (Lohr et al., 1997). The presence of a genetic contribution to late-onset and early-onset schizophrenia is evident in increased rates of schizophrenia among first-degree relatives (Rokhlina, 1975; Castle & Howard, 1992; Castle et al., 1997).
If late-onset schizophrenia is neurodevelopmental in origin, an explanation for the delayed onset may be that late-onset schizophrenia is a less severe form of the disorder and, as such, is less likely to manifest early in life. Recent research suggests that in several arenas—for example, neuropsychological impairments in learning, retrieval, abstraction, and semantic memory as well as electroencephalogram abnormalities—the deficits of patients with late-onset schizophrenia are less severe (Heaton et al., 1994; Jeste et al., 1995b; Olichney et al., 1995, 1996; Paulsen et al., 1995, 1996). Also, negative symptoms are less pronounced and neuroleptic doses are lower in patients with late-onset schizophrenia (Jeste et al., 1995b). The etiology and onset of schizophrenia in younger adults often are explained by a diathesis-stress model in which there is a genetic vulnerability in combination with an environmental insult (such as obstetric complications), with onset triggered by maturational changes or life events that stress a developmentally damaged brain (Feinberg, 1983; Weinberger, 1987; Wyatt, 1996). Under this multiple insult model, patients with late-onset schizophrenia may have had fewer insults and thus have a delayed onset. An alternative or complementary explanation for the delayed onset in late-onset schizophrenia is the possibility that these patients possess protective features that cushion the blow of any additional insults. The preponderance of women among patients with late-onset schizophrenia has fueled hypotheses that estrogen plays a protective role.
The view of late-onset schizophrenia as a less severe form of schizophrenia, in which the delayed onset results from fewer detrimental insults or the presence of protective factors, suggests a continuous relationship between age at onset and severity of liability. An alternative view is that late-onset schizophrenia is a distinct neurobiological subtype of schizophrenia. The preponderance of women and of paranoid subtype patients seen in late-onset schizophrenia supports this view. These two etiologic theories of late-onset schizophrenia call for further research.
Pharmacological treatment of schizophrenia in late life presents some unique challenges. Conventional neuroleptic agents, such as haloperidol, have proven effective in managing the “positive symptoms” (such as delusions and hallucinations) of many older patients, but these medications have a high risk of potentially disabling and persistent side effects, such as tardive dyskinesia (Jeste et al., in press). The cumulative annual incidence of tardive dyskinesia among older outpatients (29 percent) treated with relatively low daily doses of conventional antipsychotic medications is higher than that reported in younger adults (Jeste et al., in press).
Recent years have witnessed promising advances in the management of schizophrenia. Studies with mostly younger schizophrenia patients suggest that the newer “atypical” antipsychotics, such as clozapine, risperidone, olanzapine, and quetiapine, may be effective in treating those patients previously unresponsive to traditional neuroleptics. They also are associated with a lower risk of extrapyramidal symptoms and tardive dyskinesia (Jeste et al., in press). Moreover, the newer medications may be more effective in treating negative symptoms and may even yield partial improvement in certain neurocognitive deficits associated with this disorder (Green et al., 1997).
The foremost barriers to the widespread use of atypical antipsychotic medications in older adults are (1) the lack of large-scale studies to demonstrate the effectiveness and safety of these medications in older patients with multiple medical conditions, and (2) the higher cost of these medications relative to traditional neuroleptics (Thomas & Lewis, 1998).
Older people are not immune to the problems associated with improper use of alcohol and drugs, but as a rule, misuse of alcohol and prescription medications appears to be a more common problem among older adults than abuse of illicit drugs. Still, because few studies of the incidence and prevalence of substance abuse have focused on older adults—and because those few were beset by methodological problems—the popular perception may be misleading.
A persistent research problem has been that diagnostic criteria for substance abuse were developed and validated on young and middle-aged adults. For example, DSM-IV criteria include increased tolerance to the effects of the substance, which results in increased consumption over time; yet, changes in pharmacokinetics and physiology may alter drug tolerance in older adults. Decreased tolerance to alcohol among older individuals may lead to decreased consumption of alcohol with no apparent reduction in intoxication. Criteria that relate to the impact of drug use on typical tasks of young and middle adulthood, such as school and work performance or child rearing, may be largely irrelevant to older adults, who often live alone and are retired. Thus, abuse and dependence among older adults may be underestimated (Ellor & Kurz, 1982; Miller et al., 1991; King et al., 1994).
The prevalence of heavy drinking (12 to 21 drinks per week) in older adults is estimated at 3 to 9 percent (Liberto et al., 1992). One-month prevalence estimates of alcohol abuse and dependence in this group are much lower, ranging from 0.9 percent (Regier et al., 1988) to 2.2 percent (Bailey et al., 1965). Alcohol abuse and dependence are approximately four times more common among men than women (1.2 percent vs. 0.3 percent) ages 65 and older (Grant et al., 1994). Although lifetime prevalence rates for alcoholism are higher for white men and women between ages 18 and 29, African American men and women have higher rates among those 65 years and older. For Hispanics, men had rates between those of whites and African Americans. Hispanic females had a much lower rate than that for whites and African Americans (Helzer et al., 1991). Longitudinal studies suggest variously that alcohol consumption decreases with age (Temple & Leino, 1989; Adams et al., 1990), remains stable (Ekerdt et al., 1989), or increases (Gordon & Kannel, 1983), but it is anticipated that alcohol abuse or dependence will increase as the baby boomers age, since that cohort has a greater history of alcohol consumption than current cohorts of older adults (Reid & Anderson, 1997).
Older persons use prescription drugs approximately three times as frequently as the general population (Special Committee on Aging, 1987), and the use of over-the-counter medications by this group is even more extensive (Kofoed, 1984). Annual estimated expenditures on prescription drugs by older adults in the United States are $15 billion annually, a fourfold greater per capita expenditure on medications compared with that of younger individuals (Anderson et al., 1993; Jeste & Palmer, 1998). Not surprisingly, substance abuse problems in older adults frequently may result from the misuse—that is, underuse, overuse, or erratic use—of such medications; such patterns of use may be due partly to difficulties older individuals have with following and reading prescriptions (Devor et al., 1994). In its extreme form, such misuse of drugs may become drug abuse (Ellor & Kurz, 1982; DSM-IV).
Research studies that have relied on medical records review show consistently that alcohol abuse and dependence are significantly more common than other forms of substance abuse and dependence (Finlayson & Davis, 1994; Moos et al., 1994). Yet prescription drug dependence is not uncommon and, as Finlayson and Davis (1994) found, the greatest risk factor for abuse of prescription medication was being female. This finding is supported by other studies showing that older women are more likely than men to visit physicians and to be prescribed psychoactive drugs (Cafferata et al., 1983; Baum et al., 1984; Mossey & Shapiro, 1985; Adams et al., 1990). In contrast, an analysis of data from the National Household Survey on Drug Abuse concluded that older men were more likely than women to report use of sedatives, tranquilizers, and stimulants (Robins & Clayton, 1989). Older adults of both sexes are at risk for analgesic abuse, which can culminate in various nephropathies (Elseviers & De Broe, 1998).
Benzodiazepine use represents an area of particular concern for older adults given the frequency with which these medications are prescribed at inappropriately high doses (Shorr et al., 1990) and for excessive periods of time. A national survey of approximately 3,000 community-dwelling persons found that older persons were overrepresented among the 1.6 percent who had taken benzodiazepines daily for 1 year or longer (71 percent > 50 years; 33 percent > 65 years of age) (Mellinger et al., 1984). Benzodiazepine users were more likely to be older, white, female, less educated, separated/divorced, to have experienced increased stressful life events, and to have a psychiatric diagnosis (Swartz et al., 1991).
In contrast to alcohol and licit medications, older adults infrequently use illicit drugs. Less than 0.1 percent of older individuals in the Epidemiologic Catchment Area study met DSM-III (American Psychiatric Association, 1980) criteria for drug abuse/dependence during the previous month (Regier et al., 1988). This compared with a 1-month prevalence rate of 3.5 percent among 18- to 24-year-olds. ECA data further suggest a lifetime prevalence of illegal drug use of 1.6 percent for persons older than 65 years (Anthony & Helzer, 1991).
The development of addiction to illicit drugs after young adulthood is rare, while mortality is high (Atkinson et al., 1992). For example, over 27 percent of heroin addicts died during a 24-year period (Hser et al., 1993), and 5.6 percent of deaths associated with heroin or morphine use were among persons older than 55 (National Institute on Drug Abuse, 1992).
As is projected to occur with trends in alcohol consumption, the low prevalence of older adults’ drug use and abuse in the late 1990s may change as the baby boomers age. Annual “snapshot” data extrapolated from the National Household Survey on Drug Abuse, which has been conducted since 1971, afford a glimpse of trends. Patterson and Jeste (1999) recently compared prevalence estimates of those born during the baby boom with an older (> 35 years) non-baby-boomer cohort. The difference between baby boomers and the previous cohort translated in 1996 into an excess of approximately 1.1 million individuals using drugs. Their excess drug use, combined with their sheer numbers, means that more drug use is expected as this cohort ages, placing greater pressures on treatment programs and other resources.
Projections also suggest that the costs of alcohol and substance abuse are likely to rise in the near future. Across age ranges, drug abuse and alcohol abuse have been estimated to cost over $109.8 billion and $166.5 billion, respectively (Harwood et al., 1998). Although no studies have estimated the annual costs of alcohol and substance abuse among older adults, there is evidence that the presence of drug abuse and dependence greatly increases health care expenditures among individuals with comorbid medical disorders. For example, in a study of over 3 million Medicare patients who were hospitalized and discharged with a diagnosis of cardiovascular disease, average annual hospital charges were $17,979 for older patients with a concomitant diagnosis of drug dependence and $14,253 for those with a concomitant diagnosis of drug abuse, compared with only $11,387 for older patients with no concomitant drug disorder (Ingster & Cartwright, 1995). In addition, increased expenditures due to the presence of a drug disorder were greatest among older patients who also had a mental disorder.
A long-standing assumption holds that substance abuse declines as people age. Winick (1962) proposed one of the most popular theories to explain apparent decreases in substance abuse, particularly narcotics, with aging. His “maturing out” theory posits that factors associated with aging processes and length of abuse contribute to a decline in the number of older narcotic addicts. These factors include changes in developmental stages and morbidity and mortality associated with use of substances. Consistent with these hypotheses, substance abusers have higher mortality rates compared with age-matched nonabusers (Finney & Moos, 1991; Moos et al., 1994). However, some research contradicts the “maturing out” theory. For example, some studies show that persons who have been addicted for more than 5 years do not become abstinent as they age (Haastrup & Jepsen, 1988; Hser et al., 1993). Also, addicts approaching 50 years of age who were followed for more than 20 years remained involved in criminal activities (Hser et al., 1993). These findings emphasize the need to focus more attention on substance abuse in late life, especially in light of demographic trends.
The treatment of substance abuse and dependence in older adults is similar to that for other adults. Treatment involves a combination of pharmacological and psychosocial interventions, supplemented by family support and participation in self-help groups (Blazer, 1996a).
Pharmacotherapy for substance abuse and dependence in older adults has been targeted mostly at the acute management of withdrawal. When there is significant physical dependence, withdrawal from alcohol can become a life-threatening medical emergency in older adults. The detoxification of older adult patients ideally should be done in the inpatient setting because of the potential medical complications and because withdrawal symptoms in older adults can be prolonged. Benzodiazepines are often used for treatment of withdrawal symptoms. In older adults, the doses required to treat the signs and symptoms of withdrawal are usually one-half to one-third of those required for a younger adult. Short- or intermediate-acting forms usually are preferred.
Pharmacological agents for treatment of substance dependence rarely have been studied in older adults. Disulfiram use in older adults to promote abstinence is not recommended because of the potential for serious cardiovascular complications. Compounds recently proposed for use in treatment of addiction, such as flagyl, deserve further study. A rare controlled clinical trial of substance abuse treatment in older patients recently revealed naltrexone to be effective at preventing relapse with alcohol dependence (Oslin et al., 1997).
New perspectives are evolving on the nature of mental health services for older adults and the settings in which they are delivered. Far greater emphasis is being placed on community-based care, which entails care provided in homes, in outpatient settings, and through community organizations. The emphasis on community-based care has been triggered by a convergence of demographic, consumer, and public policy imperatives. In terms of demographics, approximately 95 percent of older persons at a given point in time live in the community rather than in institutions, such as nursing homes (U.S. Department of Health and Human Services, Administration on Aging, and American Association of Retired Persons [U.S.DHHS, AoA & AARP], 1995). Of those living in the community, approximately 30 percent, mostly women, live alone (U.S. DHHS, AoA & AARP, 1995). Most older persons prefer to remain in the community and to maintain their independence. Yet living alone makes them even more reliant on community-based services if they have a mental disorder.
Service delivery also is being shaped by public policy and the emergence of managed care. The escalating costs of institutional care, combined with the recognition of past abuses, stimulated policies to limit nursing home admissions and to shift treatment to the community (Maddox et al., 1996). Mental disorders are leading risk factors for institutionalization (Katz & Parmelee, 1997). Therefore, to keep older people in the community, where they prefer to be, more energies are being marshaled to promote mental health and to prevent or treat mental disorders in the community. In other words, treating mental disorders is seen as a means to stave off costly institutionalization—resulting either from a mental disorder or a comorbid somatic disorder. An untreated mental disorder, for example, can turn a minor medical problem into a life-threatening and costly condition. Problems with forgetting to take medication (e.g., with dementia), developing delusions about medication (e.g., with schizophrenia), or lowering motivation to refill prescriptions (e.g., with depression) can increase the likelihood of having more severe illnesses that demand more intensive and expensive institutional care. Therefore, promotion of mental health and treatment of mental disorders are crucial elements of service delivery.
The delivery of community-based mental health services for older adults faces an enormous challenge. Services for older adults are insufficient and fragmented, often divided between systems of health, mental health, and social services (Gatz & Smyer, 1992; Cohen & Cairl, 1996). Under these three systems, services include medical and psychosocial care, rehabilitation, recreation, housing, education, and other supports. Yet although every community has an Administration on Aging to assist with services for older adults generally, there is no administrative body responsible for integrating the daunting array of services needed specifically for individuals with severe mental illnesses. Similar problems are encountered with coordinating services for children, as discussed in Chapter 3. Local mental health authorities and systems of care have been effective in coordinating care for some groups of adults, but no special administrative mental health entities exist for older adults. The fragmentation of service systems for older people in the United States stands in contrast to the United Kingdom and Ireland, where governmental authorities coordinate their care (Reifler, 1997). Older adults eventually may benefit from the local mental health authorities developing in the United States, but thus far these authorities have been focused on services for other adults. Because of ethnic diversity in the United States, systems of care must also deal with the special needs of older Americans who have limited English proficiency and different cultural backgrounds.
The following section describes the nature and settings in which older people receive mental health services. It concentrates on primary care, adult day centers and other community care settings, and nursing homes. A recurrent theme across these settings is the failure to address mental health needs of older people. Selected issues in financing of services for older adults are discussed briefly at the end of this section, but most of the issues related to financing policy (e.g., Medicare, Medicaid) and managed care are discussed in Chapter 6.
Demographic, consumer, and public policy imperatives have propelled tremendous growth in the diversity of settings in which older persons simultaneously reside and receive care (Table 5-2). Care is no longer the strict province of home or nursing home. The diversity of home settings in suburban and urban communities extends from naturally occurring retirement communities to continuing care retirement communities to newer types of alternative living arrangements. These settings include congregate or senior housing, senior hotels, foster care, group homes, day centers (where people reside during the day), and others. The diversity of institutional settings includes nursing homes, general hospitals (with and without psychiatric units), psychiatric hospitals, and state mental hospitals, among others. In fact, the range of settings, and the nature of the services provided within each, has blurred the distinction between home and nursing home (Kane, 1995).
Across the range of settings, the duration of care can be short term or long term, depending on patients’ needs. The phrase, “long-term care,” has come to refer to a range of services for people with chronic or degenerative illness or disabilities who require support over a prolonged period of time. In the past, long-term care was synonymous with nursing home care or other forms of institutional care, but the term has come to apply to a full complement of institutional or community-based settings.
| Table 5-2. Settings for mental health services for older adults* | |
| Communities
Homes |
Institutions
Nursing homes |
| *Two other settings (not included in this table) are board and care homes and assisted living facilities. These are residential facilities that serve as a bridge between community and institutional settings and have elements of each. | |
Within the continuum of services, one new perspective—conceived as the landscape for aging— strives to tailor the environment to the needs of the person through a combined focus on health and residential requirements (Cohen, 1994). Whether at home, in a retirement community, or in a nursing home, this health and home perspective is deemed to be crucial to achieving high quality of life for older adults. Over the past 30 years, improvements in the health side of this perspective have occurred, but the home part has lagged. The challenge is to stimulate an interdisciplinary collaboration between systems of care and consumers.
One important area for an interdisciplinary approach is the extent to which a given setting fosters independent functioning versus dependent functioning, an issue influencing mental health and quality of life. Though certainly not a goal, some settings inadvertently foster dependency rather than independence. Nursing homes and hospitals, for example, are understandably more focused on what individuals cannot do, as opposed to what they can do. Yet their major focus on incapacity (the nursing and health focus) runs the risk of overshadowing function and independence (the home and humanities focus). In other settings, the balance between dependence and independence shifts in the other direction, with the risk of nursing and health needs being inadequately addressed. In recent years, the emphasis has been on “aging in place,” either at home or in the community, rather than in alternate settings.
The landscape for aging is a construct within which to examine the depth and breadth of human experience in later life (Cohen, 1998b). A health and humanities focus across this landscape offers a design for dealing with mental health problems as well as with health promotion to harness human potential. The landscape for aging, with its health and humanities orientation, is a construct designed to stir new thinking in research, practice, and policy. It also defines a clear need for new mental health services’ development and delivery, training, research, and policies to address the range of sites, each with its own unique characteristics and growing populations. The service systems, however, have yet to embrace a broader view.
Primary care6 represents a pivotal setting for the identification and treatment of mental disorders in older people. Many older people prefer to receive mental health treatment in primary care (Unutzer et al., 1997a), a preference bolstered by public financing policies that encourage their increasing reliance on primary, rather than specialty, mental health care (Mechanic, 1998). Primary care offers the potential advantages of proximity, affordability, convenience, and coordination of care for mental and somatic disorders, given that comorbidity is typical.
The potential advantages of primary care, however, have yet to be realized. Diagnosis and treatment of older people’s mental disorders in the primary care setting are inadequate. The efficacious treatments described in the depression section of this chapter are not being practiced, particularly not in primary care and other general medical settings. As documented earlier, a significant percentage of older patients with depression are underdiagnosed and undertreated. The concern about inadequate treatment of late-life depression in primary care is magnified by growing enrollment in managed care.
Primary care is generally not well equipped to treat chronic mental disorders such as depression or dementia. It has limited capacity to identify patients with common mental disorders and to provide the proactive followup that is required to retain patients in treatment. To ensure better treatment of late-life depression in primary care, there is heightening awareness of the need for new models for mental health service delivery (Unutzer et al., 1997a). New models of service delivery in primary care include mental health teams, consultation-liaison models,7 and integration of mental health professionals into primary care (Katon & Gonzales, 1994; Schulberg et al., 1995; Katon et al., 1996, 1997; Stolee et al., 1996; Gask et al., 1997). For example, the intervention developed by Katon and colleagues introduced a structured depression treatment program into the primary care setting. The program included behavioral treatment to inculcate more adaptive coping strategies and counseling to enhance compliance with antidepressant medications. Patients were randomized in a controlled trial comparing this structured depression program with usual care by primary care physicians. The investigators found patients participating in the program to have displayed better medication adherence, better satisfaction with care, and a greater decrease in severity of major depression (Katon et al., 1996).
Models that integrate mental health treatment into primary care, while thus far designed largely for depression, also may have utility for other mental disorders seen in primary care. Nevertheless, primary care is not appropriate for all patients with mental disorders. Primary care providers can be guided by a set of recommendations for appropriate referrals to specialty mental health care (American Association for Geriatric Psychiatry, 1997).
Over the past few decades, adult day centers have developed as an important service delivery approach to providing community-based long-term care. Adult day centers, although heterogeneous in orientation, provide a range of services (usually during standard “9 to 5” business hours), including assessment, social, and recreation services, for adults with chronic and serious disabilities. They represent a form of respite care designed to give caregivers a break from the responsibility of providing care and to enable them to pursue employment. Over the past 30 years, adult day centers have grown in number from fewer than 100 to over 4,000, under the sponsorship of community organizations or residential facilities. A large national demonstration program on adult day centers showed that they can care for a wide spectrum of patients with Alzheimer’s disease and related dementias and can achieve financial viability (Reifler et al., 1997; Reifler et al., in press). There also is evidence that adult day centers are cost-effective in terms of delaying institutionalization, and participants show improvement in some measures of functioning and mood (Wimo et al., 1993, 1994).
There are several approaches to delivering services in adult day centers. There is no research evidence that any one model of service delivery is superior to another. For example, a social model has been developed by Little Havana Activities & Nutrition Centers of Dade County (Florida). The Little Havana “Senior Center” provides mental health, health, social, nutritional, transportation, and recreational services, emphasizing both remedial and preventive services. The center focuses on the predominantly Cuban population of South Florida. Yet much more research is needed to demonstrate the relative effectiveness of different models of adult day services (Reifler et al., 1997).
Beyond adult day centers, other innovative models of community-based long-term care strive to incorporate mental health services. Few have been evaluated and none implemented on a wide scale. These models include the social/health maintenance organization (S/HMO) (Greenberg et al., 1988), On Lok Senior Services Program, and life care communities or continuing care retirement communities (Robinson, 1990b). These new features of the landscape of aging show promise, but there is insufficient evidence of cost-effectiveness and generalizability of these models, particularly the mental health component. Perhaps the lack of a research base and limited market account for the slow pace of their proliferation in the United States.
Most older adults live in the community and only a minority of them live in nursing homes; of the latter, about two-thirds have some kind of mental disorder (Burns, 1991). The majority have some type of dementia, while others have disabling depression or schizophrenia (Burns, 1991). Despite the high prevalence of people with mental disorders in nursing homes, these settings generally are ill equipped to meet their needs (Lombardo, 1994).
Deinstitutionalization of state mental hospitals beginning in the 1960s encouraged the expanded use of nursing homes for older adults with mental disorders. This trend was enhanced by Medicaid incentives to use nursing homes instead of mental hospitals. But the shift to nursing homes was not accompanied by alterations in care. In 1986, the Institute of Medicine issued a landmark report documenting inappropriate and inadequate care in nursing homes, including the excessive use of physical and chemical restraints (IOM, 1986). This subsequent visibility of problems prompted the passage in 1987 of the Nursing Home Reform Act (also known as the Omnibus Budget Reconciliation Act of 1987). This legislation restricted the inappropriate use of restraints and required preadmission screening for all persons suspected of having serious mental illness. The purpose of the screening was to exclude from nursing homes people with mental disorders who needed either more appropriate acute treatment in hospitals or long-term treatment in community-based settings. Preadmission screening also was designed to improve the quality of psychosocial assessments and care for nursing home residents with mental disorders. Nursing home placement is appropriate for patients with mental disorders if the disorders have produced such significant dysfunction that patients are unable to perform activities of daily living.
To meet the legislation’s requirements, nursing homes must have the capacity to deliver mental health care. Such capacity depends on trained mental health professionals to deliver appropriate care and treatment. Unfortunately, prior to and even after passage of the Omnibus Budget Reconciliation Act of 1987, Medicaid policies discouraged nursing homes from providing specialized mental health services, and Medicaid reimbursements for nursing home patients have been too low to provide a strong incentive for participation by highly trained mental health providers (Taube et al., 1990). The emphasis on community-based care, combined with inadequate nursing home reimbursement policies, has limited the development of innovative mental health services in nursing homes. Major barriers persist in the delivery of appropriate care to mentally ill residents of nursing homes.
Older adults with severe and persistent mental disorders (SPMD) are the most frequent users of long-term care either in community or institutional settings. SPMD in older adults includes lifelong and late-onset schizophrenia, delusional disorder, bipolar disorder, and recurrent major depression. It also includes Alzheimer’s disease and other dementias (and related behavioral symptoms, including psychosis), severe treatment-refractory depression, or severe behavioral problems requiring intensive and prolonged psychiatric intervention. Although these groups of disorders have different courses of illness and outcomes, they have many overlapping clinical features, share the common need for mental health long-term care services, and are frequently treated together in long-term care settings (Burns, 1991; Gottesman et al., 1991; American Psychiatric Association, 1993). It is estimated that 0.8 percent of persons older than 55 years in the United States have SPMD (Kessler et al., 1996).
As a result of the dramatic downsizing and closure of state hospitals in past decades, 89 percent of institutionalized older persons with SPMD now live in nursing homes (Burns, 1991). However, institutions are expected to play a substantially smaller role than community-based settings in future systems of mental health long-term care (Bartels et al., in press). First, the majority of older adults with SPMD presently live in the community (Meeks & Murrell, 1997; Meeks et al., 1997) and prefer to remain there. Second, experience with the Preadmission Screening and Resident Review mandated by the Omnibus Budget Reconciliation Act of 1987 has been mixed. It may have slowed inappropriate admissions to nursing homes, restricted inappropriate use of restraints, and reduced overuse of psychotropic medications, but it did not otherwise improve the quality of mental health services (Lombardo, 1994). Furthermore, states’ opposition to what they perceived to be Federal government interference in local health care policy and a general trend toward deregulation subsequently curtailed Federal nursing home reform. Finally, the growing costs of nursing home care are stimulating dramatic reforms in reimbursement and policy, including state mandates to limit Medicaid expenditures by decreasing nursing home beds and Federal reform by Medicare to implement prospective payment for nursing home services (Bartels & Levine, 1998). To accommodate the mounting number of individuals who have disorders requiring chronic care, future projections suggest the greatest growth in services will be in home and community-based settings (Institute for Health and Aging, 1996), increasingly financed through capitated and managed care arrangements.
Older adults with SPMD are high users of services (Cuffel et al., 1996; Semke & Jensen, 1997) and require mental health long-term care that is comprehensive, integrated, and multidisciplinary (Moak, 1996; Small et al., 1997; Bartels & Colenda, 1998). The mental health care needs of this population include specialized geropsychiatric services (Moak, 1996); integrated medical care (Moak & Fisher, 1991; Small et al., 1997); dementia care (Small et al., 1997; Bartels & Colenda, 1998); home and community-based long-term care; and residential and family support services, intensive case management, and psychosocial rehabilitation services (Aiken, 1990; Robinson, 1990a; Schaftt & Randolph, 1994; Lipsman, 1996). With adequate supports, older persons with SPMD can be maintained in the community, sometimes at lower cost, and with equal or improved quality of life in comparison with institutions (Bernstein & Hensley, 1988; Mosher-Ashley, 1989; Leff, 1993; Trieman et al., 1996).
However, current mental health policies have left many older persons with SPMD with decreased access to mental health care in both community and institutional settings (Knight et al., 1998). Community-based mental health services for older people are largely provided through the general medical sector, partly due to poor responsiveness to the needs of older people by community mental health organizations (Light et al., 1986). Yet reliance on the general medical sector also has not met their needs because of its focus on acute care (George, 1992). In addition, most home health agencies provide only limited short-term mental health care. The long-term care programs that exist primarily aid older adults with chronic physical disabilities or cognitive impairment but fail to address impairments in mood and behavior (Robinson, 1990a). An additional barrier is that the majority of community-residing older adults do not seek mental health services, except for medication (Meeks & Murrell, 1997), despite continued need (Meeks et al., 1997). Those without family support generally live in nursing homes, assisted living facilities, and board and care homes. These three are forms of residential care that offer some combination of housing, supportive services, and, in some cases, medical care. In short, more resources must be devoted to programs that integrate mental health rehabilitative services into long-term care in both community and institutional settings.
Financing policies furnish incentives that favor utilization of some services over others (e.g., nursing homes rather than state mental hospitals) or preclude the provision of needed services (e.g., mental health services in nursing homes). Details on financing and organizing mental health services, with a special focus on access, are presented in Chapter 6. Selected issues germane to older adults are addressed here.
Historically, Federal financing policy has imposed special limits on reimbursement for mental health services. Medicaid precluded payment for care in so-called “institutions for mental diseases,” Medicaid’s term for mental hospitals and the small percentage of nursing homes with specialized mental health services. This Medicaid policy provided a disincentive for the majority of nursing homes to specialize in delivering mental health services for fear of losing Medicaid payments (Taube et al., 1990). Under Medicare, the most salient limits were higher copayments for outpatient mental health services and a limited number of days for hospital care. Medicare’s special limits on outpatient mental health services were changed over the past decade, resulting in significantly increased access to and utilization of such services (Goldman et al., 1985; Rosenbach & Ammering, 1997). The concern, however, is that the gains made as a result of policy changes easily could be eroded by the shift to managed care (Rosenbach & Ammering, 1997).
Projections are that 35 percent of all Medicare beneficiaries will be in managed care plans by the year 2007, amounting to approximately 15.3 million people (Komisar et al., 1997). Although the managed care industry has the potential to provide a range of integrated services for people with long-term care needs, managed care’s awareness of and response to chronic care are rudimentary (Institute for Health and Aging, 1996). Despite the potential of systems of managed health care, such as HMOs, to provide comprehensive preventive, acute, and chronic care services, their current specialized geriatric programs and clinical case management for older persons tend to be inadequate or poorly implemented (Friedman & Kane, 1993; Pacala et al., 1995; Kane et al., 1997). In addition, older patients are likely to be poorly served in primary care settings (including primary care HMOs) because of minimal use of specialty providers and suboptimal pharmacological management (Bartels et al., 1997). Further, current systems lack the array of community support, residential, and rehabilitative services necessary to meet the needs of older persons with more severe mental disorders (Knight et al., 1995). These shortcomings are unlikely to be remedied until more research becomes available demonstrating cost-effective models for treating older people with mental illness.
The types of mental health services available within managed care organizations vary greatly with respect to how services are provided. In some organizations, mental health care is directly integrated into the package of general health care services (“carved-in” mental health services), while it is provided in others through a contract with a separate specialty mental health organization that provides only these services and accepts the financial risk (“carved-out” mental health services).
Proponents of carved-in mental health services argue that this model better integrates physical and mental health care, decreases barriers to mental health care due to stigma, and is more likely to produce cost-offsets and overall savings in general health care expenditures. These features are particularly relevant to older persons, as they commonly have comorbid somatic disorders for which they take multiple medications that may affect mental disorders, often avoid specialty mental health settings, and incur significant health care expenses related to psychiatric symptoms (George, 1992; Paveza & Cohen, 1996; Moak, 1996; Riley et al., 1997). Unfortunately, mental health specialty services for older persons tend to be a low priority in managed health care organizations, by comparison with medical or surgical specialty services (Bartels et al., 1997). More importantly, carved-in mental health care may have superior potential for individuals with diagnoses such as minor depression and anxiety disorders but tends to shortchange older patients with SPMD who require intensive and long-term mental health care (Mechanic, 1998). The range of outreach, rehabilitative, residential, and intensive services needed for patients with SPMD is likely to exceed the capacity, expertise, and investment of most general health care providers.
Economic factors also may limit the usefulness of mental health carve-ins in serving the needs of older individuals with SPMD. First, evidence from private sector health plans suggests that without mandated parity, insurers offer inferior coverage of mental health care (Frank et al., 1997b, 1997c). Furthermore, if providers or payers compete for enrollees, there is strong incentive to avoid enrollees expected to have higher costs from mental health problems (e.g., older persons with SPMD). To avoid such discrimination, equal coverage of mental health care would have to be mandated through legislation on mental health parity or through specialized contract requirements with managed care organizations.
Proponents of mental health service carve-outs for older persons argue that separate systems of financing and services are likely to be superior for individuals needing specialty mental health services, especially those with SPMD. In particular, advocates suggest that carved-out mental health organizations have superior technical knowledge, specialized skills, a broader array of services, greater numbers and varieties of mental health providers with experience treating severe mental disorders, and a willingness and commitment to service high-risk populations (Riley et al., 1997). From an economic perspective, since competition is largely over the carve-out contract with the payer (generally a public organization or an employer), there is less incentive to compete on risk selection, and risk adjustment becomes unnecessary. In addition, mental health carve-out organizations may be better equipped to provide rehabilitative and community support mental health services necessary to care for older persons with SPMD. Finally, growth of innovative outpatient alternatives could be stimulated by reinvestment of savings by the payer from any decrease in inpatient service use.
Unfortunately, research is lacking on outcomes and costs for older persons with SPMD in mental health carve-outs. A carve-out arrangement could lead to adverse clinical outcomes in older patients due to fragmentation of medical and mental health care services in a population with high risk of complications of comorbidity and polypharmacy. Also, from a financial perspective, the combination of physical and mental comorbidities seen in older adults, especially those with SPMD, may reduce the economic advantages of carved-out services (Bazemore, 1996; Felker et al., 1996; Tsuang & Woolson, 1997). If the provider cannot appropriately manage services and costs associated with the combination of somatic and mental health disorders, anticipated savings may not materialize. Furthermore, fragmentation of reimbursement streams would likely complicate the assessment of cost-effectiveness or cost-offsets. For example, apparent savings of mental health carve-outs under Medicare actually may be due to shifting costs when an individual is also covered under Medicaid. In this situation, Medicaid may cover prescription drugs, long-term care, and other services that are not paid for by Medicare. In order to offer true efficiencies, Medicare mental health carve-outs need to find a way to bridge the fragmentation of financing care for older persons.
There do not appear to be any studies of mental health outcomes for older adults under managed care. In general, the available research on mental health outcomes for other adults consistently finds that managed care is successful at reducing mental health care costs (Busch, 1997; Sturm, 1997), yet clinical outcomes (especially for the most severely and chronically ill) are mixed and difficult to interpret due to differences in plans and populations served. Several studies suggest that outcomes under managed care for younger adults are as favorable as, or better than, those under fee-for-service (Lurie et al., 1992; Cole et al., 1994). In contrast, others report that the greater use of nonspecialty services for mental health care under managed care is associated with less cost-effective care (Sturm & Wells, 1995), and that older and poor chronically ill patients may have worse health outcomes or outcomes that vary substantially by site and patient characteristics (Ware et al., 1996). A recent review of health outcomes for both older and younger adults in the managed care literature (Miller & Luft, 1997) concluded that there were no consistent patterns that suggested worse outcomes. However, negative outcomes were more common in patients with chronic conditions, those with diseases requiring more intensive services, low-income enrollees in worse health, impaired or frail elderly, or home health patients with chronic conditions and diseases. These risk factors apply to older adults with SPMD, suggesting that this group is at high risk for poor outcomes under managed care programs that lack specialized long-term mental health and support services. To definitively address the question of mental health outcomes for older persons under managed care, appropriate outcome measures for older adults with mental illness will need to be developed and implemented in the evolving health care delivery systems (Bartels et al., in press).
Older adults and their families depend on a multiplicity of supports that extend beyond the health and mental health care systems. Patients and caregivers need access to education, support networks, support and self-help groups, respite care, and human services, among other supports (Scott-Lennox & George, 1996). These services assume heightened importance for older people who are living alone, who are uncomfortable with formal mental health services, or who are inadequately treated in primary care. Services and supports appear to be instrumental not only for the patient but also for the family caregiver, as this section explains, but research on their efficacy is sparse. The strongest evidence surrounds the efficacy of services for family caregivers. Support for family caregivers is crucial for their own health and mental health, as well as for controlling the high costs of institutionalization of the family member in their care. The longer the patient remains home, the lower the total cost of institutional care for those who eventually need it.
Support groups, which are an adjunct to formal treatment, are designed to provide mutual support, information, and a broader social network. They can be professionally led by counselors or psychologists, but when they are run by consumers8 or family members, they are known as self-help groups. The distinction is somewhat clouded by the fact that mental health professionals and community organizations often aid self-help groups with logistical support, start-up assistance, consultation, referrals, and education (Waters, 1995). For example, self-help support groups sponsored by the Alzheimer’s Association use professionals to provide consultation to groups orchestrated by lay leaders.
Support groups for people with mental disorders and their families have been found helpful for adults (see Chapter 4). Participation in support groups, including self-help groups, reduces feelings of isolation, increases knowledge, and promotes coping efforts. What little research has been conducted on older people is generally positive but has been limited mostly to caregivers (see later section) and widows (see below), rather than to older people with mental disorders.
Despite the scant body of research, there is reason to believe that support and self-help group participation is as beneficial, if not more beneficial, for older people with mental disorders. Older people tend to live alone and to be more socially isolated than are other people. They also are less comfortable with formal mental health services. Therefore, social networks established through support and self-help groups are thought to be especially vital in preventing isolation and promoting health. Support programs also can help reduce the stigma associated with mental illness, to foster early detection of illnesses, and to improve compliance with formal interventions.
Earlier sections of this chapter documented the untoward consequences of prolonged bereavement: severe emotional distress, adjustment disorders, depression, and suicide. Outcomes have been studied for two programs of self-help for bereavement. One program, They Help Each Other Spiritually (THEOS), had robust effects on those who were more active in the program. Those widows and widowers displayed the improvements on health measures such as depression, anxiety, somatic symptoms, and self-esteem (Lieberman & Videka-Sherman, 1986). The other program, Widow to Widow: A Mutual Health Program for the Widowed, was developed by Silverman (1988). The evaluation in a controlled study found program participants experienced fewer depressive symptoms and recovered their activities and developed new relationships more quickly (Vachon, 1979; Vachon et al., 1980, 1982).
There is a need for improved consumer-oriented public information to educate older persons about health promotion and the nature of mental health problems in aging. Understanding that mental health problems are not inevitable and immutable concomitants of the aging process, but problems that can be diagnosed, treated, and prevented, empowers older persons to seek treatment and contributes to more rapid diagnosis and better treatment outcomes.
With respect to health promotion, older persons also need information about strategies that they can follow to maintain their mental health. Avoiding disease and disability, sustaining high cognitive and physical function, and engaging with life appear to be important ways to promote mental and physical health (Rowe & Kahn, 1997). The two are interdependent.
Established programs for health promotion in older people include wellness programs, life review, retirement, and bereavement groups (see review by Waters, 1995). Although controlled evaluations of these programs are infrequent, bereavement and life review appear to be the best studied. Bereavement groups produce beneficial results, as noted above, and life review has been found to produce positive outcomes in terms of stronger life satisfaction, psychological well-being, self-esteem, and less depression (Haight et al., 1998). Life review also was investigated through individualized home visits to homebound older people in the community who were not depressed but suffered chronic health conditions. Life review for these older people was found to improve life satisfaction and psychological well-being (Haight et al., 1998).
Another approach to promoting mental health is to develop a “social portfolio,” a program of sound activities and interpersonal relationships that usher individuals into old age (Cohen, 1995b). While people in the modern work force are advised to plan for future economic security—to strive for a balanced financial portfolio—too little attention is paid to developing a balanced social portfolio to help to plan for the future. Ideally, such a program will balance individual with group activities and high mobility/energy activities requiring significant physical exertion with low mobility/energy ones. The social portfolio is a mental health promotion strategy for helping people develop new strengths and satisfactions.
Among the many myths about aging is that American families do not care for their older members. Such myths are based on isolated anecdotes as opposed to aggregate data. Approximately 13 million caregivers, most of whom are women, provide unpaid care to older relatives (Biegel et al., 1991). Families are committed to their older members and provide a spectrum of assistance, from hands-on to monetary help (Bengston et al., 1985; Sussman, 1985; Gatz et al., 1990; Cohen, 1995a). Problems occur with older individuals who have no children or spouse, thereby reducing the opportunity to receive family aid. Problems also occur with the “old-old,” those over 85 whose children are themselves old and, therefore, unable to provide the same intensity of hands-on help that younger adult children can provide. These special circumstances highlight the need for careful attention to planning for mental health service delivery to older individuals with less access to family or informal support systems.
Conversely, a large and growing number of older family members care for chronically mentally ill and mentally retarded younger adults (Bengston et al., 1985; Gatz et al., 1990; Eggebeen & Wilhelm, 1995). Too little is known about ways to help the afflicted younger individuals and their caregiving parents. Families are eager to help themselves, and society needs to find ways to better enable them to do so.
There is a great need to better educate families about what they can do to help promote mental health and to prevent and treat mental health problems in their older family members. Families fall prey to negative stereotypes that little can be done for late-life mental health problems. They need to know that mental health problems in later life, like physical health problems, can be treated. They need to understand how to better recognize symptoms or signals of impending mental health problems among older adults so that they can help their loved ones receive early interventions. They need to know what services are available, where they can be found, and how to help their older relatives access such help when necessary.
The plight of family caregivers is pivotal. As noted earlier, the burden of caring for an older family member places caregivers at risk for mental and physical disorders. Virtually all studies find elevated levels of depressive symptomatology among caregivers, and those using diagnostic interviews report high rates of clinical depression and anxiety (Schultz et al., 1995). Ensuring their mental and physical health is not only vital for their well-being but also is vital for the older people in their care. Support groups and services aimed at caregivers can improve their health and quality of life, can improve management of patients in their care, and can delay their institutionalization.
Family support is often supplemented by enduring long-term relationships between older people and their neighbors and community, including religious, civic, and public organizations (Scott-Lennox & George, 1996). Linkages to these organizations instill a sense of belonging and companionship. Such linkages also provide a safety net, enabling some older people to live independently in spite of functional decline.
While the vast majority of frail and homebound older people receive quality care at home, abuse does occur. Estimates vary, but most studies find rates of abuse by caregivers (either family or nonfamily members) to range up to 5 percent (Coyne et al., 1993; Scott-Lennox & George, 1996). Abuse is generally defined in terms of being either physical, psychological, legal, or financial. The abuse is most likely to occur when the patient has dementia or late-life depression, conditions that impart relatively high psychological and physical burdens on caregivers (Coyne et al., 1993). A recent report by the Institute of Medicine describes the range of interventions for protection against abuse of older people, including caregiver participation in support groups and training programs for behavioral management (especially for Alzheimer’s disease) and social services programs (e.g., adult protective services, casework, advocacy services, and out-of-home placements). While there are very few controlled evaluations of these services (IOM, 1998), communities need to ensure that there are programs in place to prevent abuse of older people. Programs can incorporate any of a number of effective psychosocial and support interventions for patients with Alzheimer’s disease and their caregivers—interventions that were presented earlier in this section and the section on Alzheimer’s disease.
Communities need to ensure the availability of adult day care and other forms of respite services to aid caregivers striving to care for family members at home. They also can provide assistance to self-help and other support programs for patients and caregivers. In the process of facilitating or providing services, communities need to consider the diversity of their older residents—racial and ethnic diversity, socioeconomic diversity, diversity in settings where they live, and diversity in levels of general functioning. Such diversity demands comprehensive program planning, information and referral services (including directories of what is available in the community), strong outreach initiatives, and concerted ways to promote accessibility. Moreover, each component of the community-based delivery system targeting older adults should incorporate a clear focus on mental health. Too often, attention to mental health services for older people and their caregivers is negligible or absent, despite the fact, as noted earlier, that mental health problems and caregiver distress are among the leading reasons for institutionalization (Lombardo, 1994). Important life tasks remain for individuals as they age. Older individuals continue to learn and contribute to society, in spite of physiologic changes due to aging and increasing health problems.
1 Hypomania is marked by abnormally elevated mood, but the symptoms are not severe enough for mania (see Chapter 4).
2 Unipolar depression refers to the depression in patients with major depressive disorders but not to the depression in patients with bipolar disorders.
3 Executive functioning refers to the ability to plan, organize, sequence, and abstract.
4 An allele is a variant form of a gene.
5 Alogia refers to poverty of speech, and avolition refers to lack of goal-directed behavior.
6 Primary care includes services provided by general practitioners, family physicians, general internists, certain specialists designated as primary care physicians (such as pediatricians and obstetricians - gynecologists), nurse practitioners, physician assistants, and other health care professionals. General medical settings include all primary care settings plus all non-mental health specialty care.
7 Consultation-liaison models provide a bridge between psychiatry and the rest of medicine. In most models, a mental health specialist is called in as a consultant at the request of a primary care provider or works as a regular member of a team of health care providers.
8 Consumers are people engaged in and served by mental health services.