| Contents | Previous | Post Test |
Sleep is a basic human need, as important for good health as diet and exercise. When we sleep, our bodies rest but our brains are active. Sleep lays the groundwork for a productive day ahead. Although most people need eight hours of sleep each night, the National Sleep Foundation (NSF) 1998 Women and Sleep Poll found that the average woman aged 30-60 sleeps only six hours and forty-one minutes during the workweek. Research has shown that a lack of enough restful sleep results in daytime sleepiness, increased accidents, problems concentrating, poor performance on the job and in school, and possibly, increased sickness and weight gain.
Getting the right amount of sleep is vital, but just as important is the quality of your sleep. Conditions unique to women, like the menstrual cycle, pregnancy and menopause, can affect how well a woman sleeps. This is because the changing levels of hormones that a woman experiences throughout the month, like estrogen and progesterone, have an impact on sleep. Understanding the effects of these hormones, environmental factors and lifestyle habits can help women enjoy a good night’s sleep.
Changes in women’s bodies occur at different times in the menstrual cycle and may affect sleep. For example, the NSF poll found that 50% of menstruating women reported bloating that disturbed their sleep.
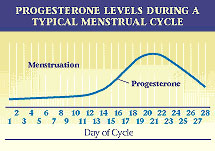
On average, these women reported disrupted sleep for two to three days each menstrual cycle. These changes can be linked to the rise and fall of hormone levels in the body. The hormone progesterone, which rises after ovulation (when an ovary releases an egg), may cause some women to feel more sleepy or fatigued. However, poor quality sleep is more likely at the beginning of the menstrual cycle when bleeding starts.
Hormones, of course, are not the only factors that influence sleep. Stress, illness, diet, lifestyle and the sleep environment all play a part. Women’s sleep experiences vary greatly during the menstrual cycle and certain types of sleep problems are associated with each phase of the cycle:
Before Ovulation (days 1-12): Typically, the period (bleeding or menstruation) occurs for about five days. After the period ends, an egg ripens in the ovary.
Ovulation (days 13-14): An egg is released. If the egg is fertilized, pregnancy occurs. Otherwise the cycle continues and a menstrual period results in about 14 days.
After Ovulation (days 15-28): If pregnancy doesn’t occur, the lining of the uterine wall begins to break down; it is shed during the menstrual period.
A healthy sleeper spends about 15-20% of his or her sleep time in deep sleep. Research suggests that women with PMS experience less deep sleep (about 5% of their total sleep) all month long.
Pregnancy is an exciting and physically demanding time. Physical symptoms (body aches, nausea, leg cramps, fetus movements and heartburn), as well as emotional changes (depression, anxiety, worry) can interfere with sleep. In the NSF poll, 78% of women reported more disturbed sleep during pregnancy than at other times. Sleep related problems also become more prevalent as the pregnancy progresses.
Pregnant women who have never snored before may begin doing so. About 30% of pregnant women snore because of increased swelling in their nasal passages. This may partially block the airways. Snoring can also lead to high blood pressure, which can put both the mother and fetus at risk. If the blockage is severe, sleep apnea may result, characterized by loud snoring and periods of stopped breathing during sleep. The lack of oxygen disrupts sleep and may affect the unborn fetus. If loud snoring and severe daytime sleepiness (another symptom of sleep apnea and other sleep disorders) occur, consult your physician.
More women (28%) than men (21%) report restless legs syndrome (RLS) symptoms in the NSF’s 1998 Omnibus Sleep in America Poll and up to 15 percent of pregnant women develop RLS during the third trimester. RLS symptoms - crawling or moving feelings in the foot, calf or upper leg - momentarily disrupt sleep. Moving the legs can stop these symptoms temporarily, but the irritation returns when the limb is still. Fortunately, RLS symptoms usually end after delivery of the baby. However, women who are not pregnant can also suffer from RLS. Medications used to treat RLS may cause harm to the fetus and should be discussed with a doctor.
Once her baby is born, a mother’s sleep is frequently interrupted, particularly if she is nursing. Mothers who nurse and those with babies that wake frequently during the night should try to nap when their babies do. Sharing baby care to the extent possible, especially during the night, is important for the mother’s health, safety, performance and vitality. After-birth blues (post-partum depression) may also be related to sleep problems. This is usually a temporary condition treatable with professional help.
Menopausal symptoms vary from woman to woman. However, women report the most sleeping problems during menopause. Snoring, for example, has been found to be more common and severe in post-menopausal women.
When a woman approaches natural menopause, her ovaries gradually (over several years) decrease production of estrogen and progesterone. If a woman has her ovaries surgically removed (oophorectomy), periods end immediately, and menopausal symptoms become more severe.
Changing and decreasing levels of estrogen cause many menopausal symptoms including hot flashes, which are unexpected feelings of heat all over the body.
They are usually accompanied by sweating. In the NSF poll, 36% of menopausal and post-menopausal women reported hot flashes during sleep. On average, they occurred three days per week and interfered with sleep five days per month. Hot flashes persist for an average of five years. While total sleep time may not suffer, sleep quality does. Hot flashes may interrupt sleep; frequent awakenings cause next-day fatigue.
Treatment with estrogen (Estrogen Replacement Therapy, ERT) or with estrogen and progesterone (Hormone Replacement Therapy, HRT) may relieve menopausal symptoms. The effects of HRT and ERT vary among women depending on the form taken (pill, patch, gel, cream or injection) and the number of years used.
Many other products target problems associated with menopause. These include nutritional products and medications such as calcium supplements, vitamin D, and bisphosphonates for the prevention or treatment of osteoporosis (thinning and weakening of the bones); estrogen creams and rings for vaginal dryness; and sleep-promoting drugs for insomnia. All forms of estrogen that enter the blood stream reduce hot flashes.
An alternative treatment for menopausal symptoms may come from soy products (tofu, soybeans, soymilk). They contain phytoestrogen, a plant hormone similar to estrogen. A few small studies indicate that soy can help lessen hot flashes. Phytoestrogens are also available in over-the-counter nutritional supplements (ginseng, extract of red clover). These supplements are not regulated by the Food and Drug Administration (FDA); their proper doses, long-terms effects and risks are not yet known.
Deciding what, if any, product to use and, if so, for how long, are questions a woman should discuss with her doctor. The answer will depend on personal and family medical history.
Nearly 40 million American men and women suffer from sleep disorders. However, sleep problems affect more women than men. New research exploring women’s sleep experiences may lead to specially tailored treatments.
Insomnia is the most common sleep problem. Women are more likely than men to report insomnia. In fact, according to the NSF poll, 53% of women aged 30-60 experience difficulty sleeping often or always: 60% of women aged 30-39, 47% aged 40-49, and 50% aged 50-60. Yet only 41% of all the women surveyed think they’ve had insomnia in the past year. Fortunately, there are a number of approaches to improving sleep, including those you can do yourself such as exercise, establishing regular bedtimes and wake times, dietary changes (less or no caffeine and alcohol) and improving your sleep environment.
If insomnia persists, and lifestyle, behavioral or diet changes do not help, a doctor may prescribe a sleep-promoting medication (hypnotic). In some instances, there may be an underlying and treatable cause, such as depression (women are twice as likely to report depression as men), stress, anxiety or pain. Doctors may prescribe antidepresssants (for depression), anxiolytics (anti-anxiety drugs), pain medications and/or hypnotic medications to improve sleep.
An estimated 12 million plus Americans have sleep apnea including one in four women over 65.While apnea is more common in men, it increases in women after age 50. Sleep apnea is a serious sleep disorder that is characterized by snoring, interrupted breathing during sleep or excessive daytime sleepiness. Recent studies have also found that sleep apnea is associated with increased blood pressure, a risk for cardiovascular disease and stroke. If any of these symptoms appear, it is important to address them with your doctor. A number of effective treatment approaches are available.
Feeling sleepy during the day or at times you expect to be awake may indicate a need for more sleep or the presence of a serious but treatable disorder such as those already mentioned or narcolepsy, a chronic neurological disorder that affects approximately one in 2000 people. Narcolepsy symptoms frequently appear in teen years. In addition to excessive daytime sleepiness, people with narcolepsy have sudden “sleep attacks” (an over-whelming urge to sleep), suddenly lose muscle tone or strength (cataplexy) and may have disturbed nighttime sleep. Recent scientific breakthroughs have led to new under-standing of the cause of this condition and new treatments have given doctors more ways to help manage its symptoms.
Persons with nocturnal sleep-related eating disorder (NS-RED), an uncommon condition, eat food during the night while they appear asleep. Since parts of the brain that control memory are asleep, people with NS-RED cannot remember nighttime eating. One study indicates that over 66 percent of sufferers are women. NS-RED can occur during sleepwalking. It can be caused by medications (e.g., some drugs prescribed for depression or insomnia) or by sleep disorders (sleep apnea, restless legs syndrome) that cause awakenings and trigger sleep-eating.
More women (58%) suffer from nighttime pain than men (48%), according to a 1996 NSF Gallup Poll Pain conditions like migraine, tension headaches, chronic fatigue syndrome and fibromyalgia are all more common among women. Pain may make it harder to fall asleep or lead to nighttime or early morning awakenings. Relaxation techniques, biofeedback, cognitive therapy, and over-the-counter and prescription medications may help. Treatment may target the pain, the sleeping difficulty, or both.
Shift Workers- about one in five Americans - work non-traditional hours (not the typical hours of 9 a.m. to 5 p.m.). Difficulty falling asleep is a common effect. However, female shift workers also suffer irregular menstrual cycles, difficulty getting pregnant, higher rates of miscarriages, premature births and low birth-weight babies more than regular day working women, according to several large studies. Changes in exposure to light and lost sleep caused by shift work may have biological or hormonal effects that are not yet entirely understood. Still, most shift-working women do have normal, healthy babies. Women shift workers should consult their doctors if experiencing menstrual difficulties, infertility or pregnancy.
When traveling to a different time zone, the body takes time to adjust. This causes the physical experience known as jet lag. Helpful tips include avoiding caffeine and alcohol, changing your sleep and wake time before your trip, (to gradually get closer to your new schedule), and exposing yourself to sunlight or bright light upon arrival (in accordance with your new wake up time) may help you overcome jet lag more quickly.
Many sleep problems can be improved by changing your sleep habits, reducing stress, improving your diet or exercising. If sleep problems persist, it is advised to seek professional help. Your doctor will determine the cause of your sleep problem and may refer you to a sleep disorders center. These centers are staffed with sleep specialists who will ask you questions about your sleep problems and may monitor your sleep overnight.
For more information about sleep contact the:
National Sleep Foundation
1522 K Street, NW, Suite 500
Washington, DC 20005
www.sleepfoundation.org