14. Antiarrhythmic Agents, Beta Adrenergic Receptor Blocking Agents, and Calcium Channel Blocking Agents
ANTIARRHYTHMIC AGENTS
Antiarrhythmic drugs produce the desired effect by altering automaticity, excitability, or conductivity of cardiac cells. Automaticity is the ability of the cells of the myocardium to spontaneously initiate electrical impulses. The response of cardiac cells to stimulation is termed excitability. Conduction velocity is termed conductivity.
Electrophysiologic Mechanism of Antiarrhythmic Agents
On a cellular level, antiarrhythmic agents can be divided into several classes based on their electrophy-siologic properties and effects on the conduction system of cardiac muscle tissue. Electrophysiologic effects are reflected in the agents' interference with one of the phases of the action potential. The rapid sequence of changes that occurs when a cardiac cell's membrane is stimulated is called an action potential. Table 14.1 outlines the phases of an action potential. Action potentials are the result of the movement of ions across the cell membrane. There are two types of action potentials in the heart: slow response and fast response. The type of action potential generated is generally due to the type .of channel that the ion travels. Action potentials correlate with the cardiac cycle (Table 14.2).
| Table 14.1 Phases of an Action Potential |
|
Phase 0 |
| Phase 0 is the almost instantaneous depolarization of the
cell that occurs when an electrical impulse contacts the cell membrane,
reversing the charge of its interior, Phase 0 is the sharp, tall upstroke. |
| Phases 1,2,3 |
| These phases represent the cell recovery period and return
to the original negative state. |
| |
Phase 1 equals overshoot. |
| |
Phase 2 equals plateau. |
| |
Phase 3 equals the rapid repolarization. |
| Phase 4 |
| The cell is repolarized, resting, ready to be fired again,
This is termed the resting membrane potential. |
| The action potential phases correlate with specific ionic
movements through the cell membrane. |
| |
Phase 0 = Na+ in flux |
| |
Phase 1 = K+ efflux Cl- in flux |
| |
Phase 2 = Ca++ in flux, K+ efflux |
| |
Phase 3 = K+ efflux |
| |
Phase 4 = the Na-K+ pump restores normal ion concentrations |
|
|
Classification
The antiarrhythmic drugs have been classified (Vaughn-Williams classification) into four groups based on their electrophysiologic effect on the action potential.50,66
Class I drugs act directly on cardiac cells by depressing sodium (fast channel) inward movement and therefore depressing membrane response, slowing the velocity of Phase 0 of the action potential. The refractory period is then prolonged. This group of drugs is effective in the treatment of arrhythmias if increased automaticity and reentry problems are present. Quinindine is the prototype of this class.
Class I antiarrhythmics have three subgroups based on conduction velocity and repolarization properties. Class IA agents depress Phase 0 and prolong the action potential. Quinidine and procainamide are examples of drugs in Class IA.
Class IB agents slightly depress Phase 0 and the action potential duration. The prototype of Class IB drugs is lidocaine.
Class 1C agents markedly depress Phase 0 but increase the QRS duration. The prototype of Class 1C agents is flecainide.
Class III agents prolong action potential duration and lengthen the effective refractory period. These drugs have little effect on the rapid upstroke of the action potential but prolong repolarization. The example of Class III agents is bretylium.
Class IV drugs are those that depress the calcium (slow) channels during Phase 2 of the action potential; they are called calcium channel blockers. The slow channels predominate in the sinoatrial (SA) and AV nodes. These drugs increase AV nodal refractoriness and conduction time. The prototype of an antiarrhythmic calcium blocking agent is verapamil. Nifedipine and diltiazem, although classed as calcium channel blockers, are less effective in treating arrhythmia.61
Although the newer drugs can be placed in classes on the basis of their cellular actions, this classification system does not have strong clinical significance because one ineffective drug in a class does not preclude the effectiveness of another drug in the same class. Many of the new antiarrhythmic agents have characteristics of more than one class.
| Table 14.2 Correlations of Ventricular Action Potential
with the ECG |
|
QRS complex - corresponds with upstroke of the action potential — Phase 0
and Phase 1 |
| ST segment - corresponds with the plateau — Phase 2 |
| T wave - reflects repolarization — Phase 3 |
| The isoelectric segment - following the T wave, corresponds to
ventricular diastole — Phase 4 |
|
Class I
Class IA. The Class IA agents, in addition to blocking the fast sodium channel, variably lengthen the action potential duration in all cardiac tissues. This property enables the drugs to convert atrial flutter and fibrillation to sinus rhythm. They slow atrial rates in flutter and may accelerate the ventricular response. Because of their activity in decreasing conduction and increasing the effective refractory period of bypass tracts, they are effective in slowing ventricular response in atrial fibrillation and flutter complicating the Wolff-Parkinson-White (W-P-W) syndrome. Although effective in most ventricular arrhythmias, they are contraindicated in torsade de pointes (see quinidine).
The Class IA agents include quinidine (quinidine sulfate and quinidine gluconate) and procainamide (Pronestyl), the two classic antiarrhythmic drugs in use for decades. Quinidine is used in the treatment of both atrial and ventricular arrhythmias. It is used primarily on a long-term basis to prevent recurrence of supraventricular tachyarrythmias and to suppress ventricular premature beats. It is administered orally or by the intravenous route.
Quinidine has many side effects: gastrointestinal problems (intolerable diarrhea is the most severe), skin rashes, and central nervous system problems, ranging from lightheadedness to severe hypotension and confusion. ECG changes, including a widened QRS complex and a widened QT interval, are common adverse reactions.
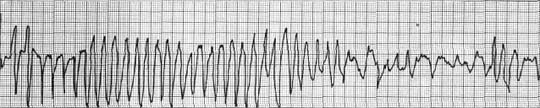
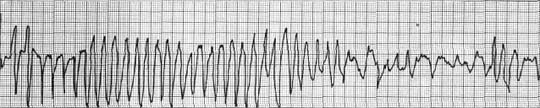
Another adverse effect seen in patients treated with either quinidine or Pronestyl is
torsade de pointes. The term refers to ventricular tachycardia characterized by QRS complexes of changing amplitude that appear to twist around the isoelectric line. The rates are very rapid.
Torsade de pointes frequently occurs in the setting of a long QT interval (Fig. 14.1).
A rarely seen adverse effect to quinidine, and possibly other Class I antiarrhythmics, is Barlow's syndrome, also known as the click-murmur syndrome. This problem is described as an apical systolic murmur with a systolic click and an ECG with inferior ischemic changes in association with a mitral regurgi-tation due to mitral valve prolapse. Pain is also associated with this syndrome, although its mechanism is not understood. Patients with Barlow's syndrome have premature ventricular complexes (PVCs) with prolonged QT interval. Normal doses of quinidine may further prolong the QT interval, resulting in more serious complications.
Procainamide is effective in controlling arrhythmias of atrial and ventricular origin. It is preferentially used in ventricular arrhythmias such as premature ventricular contractions and ventricular tachycardia. Atrial arrhythmias unresponsive to quinidine, such as atrial fibrillation, flutter, and paroxysmal supraventricular tachycardia, may respond to procainamide.
Ajmaline, a new Class IA antiarrhythmic agent, is used (1) as a treatment of arrhythmias resistant to all conventional agents; (2) as a test for AV conduction in patients with possible paroxysmal or latent heart block; and (3) as a treatment of arrhythmias associated with the W-P-W syndrome. Ajmaline prolongs the effective refractory period of the atria and prolongs conduction in the His-Purkinje system. This effect is evident in patients with intraventricular conduction disturbances that can be aggravated by ajmaline. Ajmaline may be administered intravenously to control serious ventricular arrhythmias resistant to lidocaine and procainamide. The oral administration is the drug prajmalium bitartrate, also effective in suppressing and preventing ventricular arrhythmias. Treatment with ajmaline is associated with a high incidence of adverse effects. Complete AV block, intraventricular conduction disturbances, and a negative inotropic effect are encountered during the intravenous administration of the drug. Hepatotoxicity and mild gastrointestinal side effects have also been reported.
For studies of the conduction system, 50 mg of ajmaline is given intravenously over a 3-minute period with careful monitoring. Some protocols use an epicardial pacing wire in place temporarily to treat the development of complete AV block.
Imipramine is a tricyclic antidepressant drug that has been used for many years. In recent trials, the antiarrhythmic properties have been identified. Although the site of action against ventricular arrhythmias is not known, it appears to be effective in the suppression of chronic PVCs. Tachycardia and unusual electrical delays on ECG are side effects of high doses.
Pirmenol is also a new Class IA drug. It is used to treat PVCs and ventricular arrhythmias and can be given orally or intravenously. A single oral dose of 150-250 mg is effective.
Cibenzoline is a unique addition to the Class IA drugs in that it does not affect the QT interval, although it does prolong infranodal conduction time and QRS interval.26,55 It is potentially effective in the treatment of supraventricular tachycardia (SVT), atrial fibrillation, and atrial flutter because it can prolong infranodal conduction time. This drug has been shown to reduce the incidence of ventricular ectopics. Cibenzoline is used cautiously in patients with bundle branch blocks or extensive infranodal disease because of its ability to prolong conduction from the His to the Purkinje system in the ventricles.
Class IB. Class IB agents generally decrease the maximal rate of Phase 0 depolarization and shorten the action potential duration in Purkinje fibers. The QT interval tends to be shortened by these drugs, suggesting their use in the treatment of ventricular tachyarrhythmias associated with QT prolongation. Lidocaine, the prototype of these drugs, acts directly on the heart. It is of value in the treatment of ventricular ectopic beats, both ventricular tachycardia and PVCs.10 The drug decreases the action potential duration in the Purkinje system. It is rapidly effective. Lidocaine is known to produce central nervous system effects such as confusion, distorted sensorium, and, in high doses, convulsions. This is particularly true in older patients. Infusion rates as well as the time frame of continued infusion must be closely monitored.
|
 |
|
Figure 14.1 Torsade de pointes. One severe adverse reaction to some of the quinidine—like Class I antiarrhythmics that prolong QT interval—is Torsade de pointes. This arrhythmia is characterized by bursts of VT with undulation of the QRS axis. The symptoms often occur in association with prolonged QT interval and bradycardic heart rates. Diarrhea, the most common symptom of Gl intolerance of quinine or pronestyl, can lead to hypokalemia and, in turn, to a prolonged QT interval. If the syndrome occurs, the medication is discontinued immediately. |
Aprindine (Fibocil), another of the new antiarrhythmic agents, has also been shown to slow or block conduction in accessory pathways of W-P-W syndrome patients. Aprindine controls ventricular and supraventricular tachyarrhythmias. It is effective in treatment of a variety of potentially lethal drug-resistant arrhythmias. It is of value in the treatment of patients with PVCs and recurrent ventricular tachycardia with mitral valve prolapse. The antiarrhythmic effects may not be seen for several days, even following initial loading doses.
The side effects may limit the therapeutic use of aprindine. They include neurologic effects, ranging from tremors to hallucinations to seizures; gastroin-testinal effects of nausea, vomiting, and diarrhea; and cardiovascular effects of hypotension and bradycar-dia. Prolonged administration may produce agranu-locytosis and cholestatic jaundice. The agranulocytosis is potentially life threatening and requires a weekly report of white blood cell count.
Ethmozine is used to treat ventricular arrhythmias, particularly in the treatment of nonlethal PVCs. It slows AV nodal and infranodal conduction without affecting refractory periods. Ethmozine is effective by oral administration. Side effects are mild and rarely reported. They include dizziness, headache, nausea, and epigastric pain. In low-dose long-term therapy, adverse effects are rare. Like other antiarrhythmic agents, ethmozine may occasionally be associated with increased frequency of arrhythmias, which is known as the "proarrhythmia effect."
Mexiletine (mexitil) is a new Class IB antiarrhythmic agent with electrophysiologic properties similar to lidocaine. In the presence of an acute myocardial infarction, intravenous mexiletine may be effective in suppressing premature ventricular beats and ventricular tachycardia. It does not appear to be effective in the treatment of recurrent ventricular tachycardias. It has recently been shown to be effective in life-threatening arrhythmias unresponsive to other agents. The reported adverse effects include some neurologic effects such as tremor, dysarthria, diplopia, and paresthesia. The intravenous infusion may exacerbate hypotension or arrhythmia and may create bradycardia or hypotension. Gastrointestinal adverse effects are reported and may be significant.
Tocainide, another new agent similar to lidocaine in its pharmacologic properties, is an orally effective agent. It is used in the treatment of ventricular arrhythmias and ventricular tachycardia. Tocainide has shown improvement in patients with chronic stable PVCs, but it is less effective in preventing chronic recurrent ventricular tachycardia. Adverse side effects have limited use of this drug. Some of the more common problems are gastrointestinal (nausea, anorexia, vomiting) and central nervous system symptoms. The most frequently reported adverse effect is tremulousness. Others included anxiety, dizziness, disorientation, and paresthesia.
Class 1C. The Class 1C agents are the most recent additions to anitarrhythmic therapy. Generally, drugs in this group are characterized by a potent depressing effect on Phase 0 depolarization of the fast sodium channel. In the ventricles, there is a marked reduction in conduction velocity produced by these drugs, which will prolong the QRS duration even when the ventricular rate is slow in normal sinus rhythm. Class 1C agents are effective in eliminating premature ventricular contractions, but because of their potent depressing activity, these drugs may also facilitate the production of arrhythmias.
Encainide is found useful in the treatment of various ventricular arrhythmias, including those resistant to other drugs. It has also proven effective in some cases of supraventricular arrhythmias such as premature atrial contractions (PACs). Encainide prolongs the P-R and QRS intervals. Adverse effects may appear in patients receiving more than 200 mg daily. Lower doses are usually well tolerated. Encainide may aggravate arrhythmias and create central nervous system effects such as lightheadedness, dizziness, tremor, ataxia, or facial numbness. Blurred vision has also been reported. Doses are individualized, with some patients requiring administration every 4 hours. Careful monitoring is required during initial administration of encainide, which limits treatment to the in-hospital patient.
Flecainide (Tambocor) is considered the prototype of the Class 1C drugs. It is found to be more potent than many of the conventional antiarrhythmic agents. It is effective in the treatment of a variety of ventricular arrhythmias, particularly the life-threatening ventricular arrhythmias and the sustained ventricular tachyarrhythmias. Flecainide prolongs intra-cardiac conduction in all segments of the conduction system. In patients with advanced ventricular dysfunction, the negative inotropic effect and the potential for creating arrhythmias of this drug must be weighed against the advantage of its use. Flecainide slows conduction and produces dose-related increases in PR, QRS, and QT intervals. Side effects of the agent are usually mild to moderate and include dizziness, visual disturbances, paresthesia, headache, nausea, and fatigue. The serious adverse effect reported is the occurrence of worsening ventricular arrhythmias.
Lorcainide is an agent that is effective against a variety of ventricular and supraventricular arrhythmias. Its main use at present is for the treatment of chronic ventricular arrhythmias. Administered either intravenously or orally, the drug will suppress ventricular arrhythmias. Lorcainide is also effective with reentrant tachycardia in patients with W-P-W syndrome. Supraventricular tachycardias not associated with W-P-W syndrome, such as atrial fibrillation, atrial flutter, and PACs, are also reduced.
Because of adverse side effects, which are considerable with lorcainide, it is suggested that the drug be started at low doses and increased at one-week intervals. The most common effect is sleep disturbance encountered in the first month of therapy. The problem centers around frequent awakening during sleep, vivid dreams, hot flashes, and chill sensations. Nausea is the second most common adverse effect. After bolus injection, patients report tremors, blurred vision, and dizziness. Other side effects reported are anxiety, headache, and gastrointestinal disturbances. A few reports of third-degree AV blocks and hypo-tension have been noted.
Propafenone, another of the new antiarrhythmic drugs, is used in the treatment of supraventricular and ventricular premature complexes.7It differs from other Class 1C agents because it exhibits some beta blocking and calcium channel blocking properties, although it does not depress conduction to the same degree as flecainide or encainide. Probably because of its less potent conduction depressing activity, the potential for creating new arrhythmias is reduced. Propafenone produces marked suppression of premature ventricular contractions. The major side effects of this agent are related to central nervous system and gastrointestinal disturbances, but heart failure may be aggravated in patients with severely depressed ventricular function. The oral administration is 150-300 mg every 8-12 hours.
Class II
The beta blocking agents are the Class II antiarrhythmic agents. Their role in the treatment of arrhythmias stems from their ability to block beta receptors. Although primarily investigated for the treatment of hypertension, the relationship between membrane currents and adrenergic receptor excitation and inhibition in the production of ventricular ectopic activity is now being investigated. The membrane-stabilizing activity, or local anestheticlike properties of some beta adrenoreceptor blockers, causes inhibition of Phase 0 of the cardiac action potential.
The beta blockers are not the first choice in the treatment of acute ventricular tachycardias. The Class I agents are preferred. The beta blockers have proven to be of value for prophylaxis against recurrent ventricular tachycardias, particularly if the precipitating cause is sympathetic stimulation. In evaluation studies, the new beta blocking agents have shown a reduction in sudden cardiac death in patients started on beta blocker therapy following a myocardial infarc-tion. It is believed that by effectively blocking the beta receptors—betai in particular—these agents attenuate cardiac stimulation by the sympathetic nervous system and perhaps the potential for reentrant ventricular arrhythmias and sudden death.
The most consistent effect of the beta blockers as antiarrhythmic agents appears to be in tachyarrhy-thmias due to sympathetic excitation. The effect of these drugs on the AV node is to terminate reentrant paroxysmal supraventricular tachycardia and slow the ventricular response in atrial flutter and atrial fibrillation. The beta blockers will rarely convert atrial fibrillation or atrial flutter to normal sinus rhythm (NSR). They are not powerful suppressors of PVCs, nor do they control life-threatening ventricular tachy-arrhythmias. They are effective in ventricular tachy-arrhythmias induced by exercise.
Class III
The concept of lengthening the action potential duration and the refractoriness of cardiac muscle is significant in the control of cardiac arrhythmias. The Class III agents have this property and do not appear to exert a depressant effect on cardiac function. There is a lower incidence of arrhythmogenicity with Class III agents as compared to the Class I agents. Additionally, these drugs possess an antifibrillatory feature. This effect may be particularly important in the control of life-threatening ventricular arrhythmias. The Class III agents prolong repolarization by affecting Phases 1 and 2 of the action potential.
Amiodarone is a drug that was introduced as an antianginal agent and is now considered a Class III antiarrhythmic. It is known to lengthen AV nodal conduction time and refractory periods. It is used in the treatment of ventricular and supraventricular arrhythmias, specifically paroxysmal atrial fibrillation and atrial flutter, supraventricular tachycardias, and recurrent ventricular tachycardia (VT) and ventricular fibrillation (VF).65 The adverse effects of amiodarone are frequently severe. Bradycardia and complete heart block have occurred with IV administration. Hypotension secondary to vasodilatation is also reported. Long-term administration has resulted in dose-related corneal microdeposits, which are reversible and do not disturb vision. The microdeposits are a result of amiodarone being excreted by the lacrimal glands. Pulmonary fibrosis and other pulmonary problems develop and become serious and permanent. Rare cases of erythema nodosum have been reported. Photosensitivity and pigmentation are also side effects. It is suggested that patients on amiodarone therapy avoid sun exposure. Occasionally, a slate-gray or bluish discoloration of the skin may persist for months after the drug is discontinued.
Amiodarone has a long half-life, remaining in the system for weeks or months. Although it is a useful drug for treatment of arrhythmias, it should be used only for patients refractory to other treatment regimens because of its high degree of tissue storage and its unusual side effects. Because of its long half-life, amiodarone becomes effective after days or weeks of administration.
Bretylium tosolate (Bretylol) the prototype for Class III antiarrhythmics, is used when the patient is refractory to other agents. Bretylium acutely suppresses ventricular fibrillation and ventricular arrhythmias.54 The mechanism by which this drug is effective is not clear. When first injected, catechol-amines are released, which tend to increase heart rate, but this effect on both myocardium and peripheral vascular resistance is quickly dissipated. The suppression of ventricular fibrillation is rapid; other ventricular arrhythmias react more slowly—20 minutes to 2 hours for onset of antiarrhythmic effect. The reported adverse effects of bretylium include postural hypotension accompanied by dizziness, vertigo, lightheadedness, and faintness. There is also some degree of hypotension in the supine position. Patients should remain in the supine position until tolerance to the drug occurs. Bretylium is used only for treatment of life-threatening arrhythmias under constant ECG monitoring conditions.
Bethanide is a Class III drug with some properties of both Class I and Class IV antiarrhythmic drugs. It is an oral analog of bretylium. Bethanide is used for patients unresponsive to conventional agents. It has shown promise in hypertensive patients with arrhythmias. It is administered intravenously only with monitoring in the CCU. Adverse effects reported are hypotension following oral administration and marked hypertension with the intravenous administration. Bethanide causes a catecholamine release that may be of benefit in emergency situations dealing with the hypotensive patient in ventricular fibrillation or ventricular tachycardia.
Clofillium is a new Class III drug used for supra-ventricular and ventricular tachycardias. It is an antifi-brillatory agent and has shown ability to interrupt and suppress reentrant arrhythmias. Adverse effects include tinnitus and lightheadedness. The adverse effects are of short duration—5-10 minutes.
Melperone is a neuroleptic drug whose antiarrhythmic properties are now being investigated. It demonstrates features of a Class III antiarrhythmic. Melperone is primarily used in the postmyocardial infarction patient with hypertension. This drug reduces the number of PVCs, multiform PVCs, R on T type PVCs, and runs of ventricular ectopic beats. The reported side effect is sedation.
The new antiarrhythmic N-acecainide (NAPA) (N-Acetylprocainamide) is the principal metabolite of procainamide, but it differs electrophysiologically from procainamide. NAPA produces less prolongation of conduction time and less increase in the AV nodal functional refractory period. It may be more useful than procainamide because (1) it appears to be less likely to cause lupus erythematosus; (2) it lacks negative inotropic effects; and (3) it has a longer elimination period, permitting longer intervals between doses. It is used in treatment of ventricular arrhythmias. The reported adverse effects include mild nausea, diarrhea, and abdominal pain. Pruritic rash is also reported, as are central nervous system symptoms of dizziness and lightheadedness. The toxic to therapeutic levels of this drug are so close that it is not recommended for general use.
Sotalol is a beta blocker with Class III antiarrhythmic features. It has broad spectrum activity; it is effective in treatment of supraventricular as well as ventricular arrhythmias, including PVCs occurring singly, in pairs, or in triplets. It has been shown to convert atrial flutter and atrial fibrillation to sinus rhythm. When conversion does not occur, the ventricular response is slowed. It has also been effective in terminating paroxysmal supraventricular tachycardia. Sotalol has been effective for high-risk patients. The most significant adverse effect of this drug is the lengthening of the QT interval with episodes of syncope. Sotalol is viewed as a major advance in new antiarrhythmic agents.
Class IV
The Class IV agents, the calcium antagonists, are newly identified as antiarrhythmia agents. Although verapamil, the prototype of this class, has been in use for atrial arrhythmias for some time, the newer agents appear to have a wider range of antiarrhythmic activity. Successful use of these drugs in the treatment of angina pectoris has led to the discovery of several new agents. The antiarrhythmic activity is now being investigated.
Class V
A possible fifth class of antiarrhythmic agents has now been identified. At this time, only one agent, alinidine, is included. This drug reduces heart rate in an as yet unidentified mechanism. It is believed that alinidine restricts flow of current through anion selective channels not yet identified. Investigation has shown that alinidine (1) does NOT increase potassium permeability and (2) does NOT decrease sodium or calcium permeability. The activity appears to be in delay and restriction of SA nodal cells. At this time, alinidine is used to treat supraventricular tachycardias. It has been shown to improve perfusion and function of ischemic myocardium by reducing heart rate.
Nursing Management
Priorities when administering an antiarrhythmic agent are:
- Observe for signs or symptoms of cardiac and extracardiac toxicity, such as heart-block, prolonged PR interval, depressed conduction in the ventricles, widened QRS complexes, and bradycardia.
- Record rate and character of apical and radial pulses.
- Monitor blood pressure frequently.
- Keep available the drugs for treating cardiac toxicity and the equipment for emergency problems.
- Assess for signs of congestive heart failure or edema, such as fatigue or dyspnea.
- Discuss medication regimens and prior medications with the patient.
- Assess and evaluate response to the medical regimen. Collect frequent rhythm strips to document response to medications.
- Monitor patients on Holier monitoring before and after administration of medication.
- Determine if medication should be given with food.
- Monitor electrolytes; report changes.
- For IV infusions, monitor site, rate of infusion, and dosage mixture.
- Assess patients' sensorium frequently.
- Assess for gastric disturbances; prevent aspiration.
- Instruct patient about possible side effects from agents.
|
|
BETA ADRENERGIC RECEPTOR BLOCKING AGENTS
Beta adrenoreceptor blockers are competitive inhibitors of the effect of catecholamines on beta adrenoreceptors in the heart, peripheral circulation, pulmonary airways, central nervous system, and various other body tissues.29 These drugs are alike as beta blockers but have decidedly differing features (Table 14.3). In the Vaughn-Williams drug classification, beta blockers are the Class II antiarrhythmics.
| Table 14.3 Differences between the Beta
Adrenoreceptor Antagonists |
|
The similarity of beta blockers is in the manner by which they induce
blockage. It is a dose-dependent manner—up to a maximal level. |
| The differing features: |
| 1. |
Potency of beta blockage |
| 2. |
Cardioselectivity |
| 3. |
Intrinsic sympathomimetic activity—the partial agonist effect of some of
the drugs |
| 4. |
Membrane-stabilizing activity |
| 5. |
Direct vasodilatory effect |
| 6. |
Class II and III antiarrhythmic properties |
| 7. |
Lipophilicity and hydrophilicity |
| 8. |
Route of elimination |
| 9. |
Duration of action |
|
|
Beta adrenergic blocking agents are used in the treatment of hypertension, angina pectoris, and cardiac arrhythmias46 (Table 14.4). The individual properties of the drugs differ; therefore the choice of agent to use is influenced by its activity. Cardioselectivity is an important feature in choosing a beta blocker. The drugs that affect beta1 (cardiac) and beta2
(peripheral) receptors are nonselective. Those that preferentially block beta1 receptors are called cardioselective. The advantage is that these drugs in controlled dosages may be used without the danger of bronchoconstriction. This is an important point for the patient with obstructive pulmonary disease such as asthma.36
Properties of Beta Adrenoreceptor Antagonists
Selectivity
The use of beta blocking agents is limited for some patients. Impaired pulmonary function, bronchospasm, and peripheral vascular disorders are some of the adverse reactions in the use of these
| Table 14.4 Therapeutic Effects of the Beta
Blockers in Selected Cardiovascular Problems |
| 1. |
Angina Pectoris |
| |
a. |
Antianginal effect is related to reduction of heart rate,
systolic blood pressure, and velocity and extent of myocardial contraction,
the determinates of myocardial dial oxygen consumption |
| |
b. |
Reduces the coronary blood flow due to the reduced
myocardial oxygen demand |
| 2. |
Hypertension |
| |
a. |
Although the mechanism of antihypertensive effect has not
yet been established, the effect is probably due to |
| |
|
(1) |
reduction in cardiac output due to a decrease in heart rate and
contractility; |
| |
|
(2) |
inhibition of renin release by the kidneys; |
| |
|
(3) |
an effect on central nervous system; |
| |
|
(2) |
suppression of the adrenergic-vasoconstrictor stimulation; and |
| |
|
(5) |
reset of baroreceptors |
| |
b. |
Lowers systolic and diastolic pressure in both supine and
standing positions |
| |
c. |
Effective at rest and during exercise |
| |
d. |
Combinations of these |
| 3. |
Arrhythmias (Class II Antiarrhythmic) |
| |
a. |
Slows spontaneous sinus node rate and ectopic refractory
period of atrioventricular node; slows reentry pathways |
| |
b. |
Alleviates ischemic-induced arrhythmias by the effect on
oxygen demand-supply ratio |
| 4. |
Cardiac Protection/Prevention of Myocardial Damage Extension |
| |
a. |
Adrenergic stimulation of the heart increases during acute
myocardial ischemia and infarction, aggravating myocardial damage |
| |
b. |
Beta blockers shown to limit myocardial damage by reducing
myocardial oxygen demand and exerting an antiarrhythmic effect |
|
|
|
|
drugs. Beta1 receptors affect cardiac stimulation, and beta2 receptors affect smooth muscle relaxation in the pulmonary airways and blood vessels. It is believed that beta1 selective blockers cause fewer adverse reactions related to the peripheral circulation than do nonselective blockers. The incidence of cold extremities and Raynaud's phenomenon is less with beta1selective blockers than with nonselective blockers.
Intrinsic Sympathomimetic Activity
The clinical effect of beta blockers results from action on myocardial contractility and heart rate. At rest, the beta blocker without intrinsic sympathomi-metic activity will decrease heart rate; those with this property may increase heart rate and protect against prolonged atrioventricular conduction time. Pindolol, however, with intrinsic sympathomimetic activity, may worsen AV block.
Membrane Stabilizing Activity
Membrane stabilizing activity refers to the local anestheticlike properties of some beta adrenoreceptor blockers that cause inhibition of Phase 0 of the cardiac action potential. It describes the inhibition of sodium current across the cell membranes. It is defined elec-trophysiologically as the reduction in the rate of rise of the action potential, occurring without altering the duration of the action potential or the resting potential. Most of these agents have a depressant effect on cardiac cells. Membrane stabilization is a small therapeutic role for the beta blockers.
Direct Vasodilatory Effect
This effect is limited in the beta blocking agents. Labetolol has the effect, resulting from blockade of peripheral alpha adrenergic mediated vasoconstric-tion. Blood pressure is lowered acutely.
Lipophilicity and Hydrophilicity
Lipophilicity refers to the lipid solubility, and hy-drophilicity refers to the water solubility of the agents. Hydrophilicity and limited access to certain tissues may be the reason for cardioselectivity. Most cardioselective beta blockers are hydrophilic, but this property is not essential for cardioselectivity. Li-pophilic beta blockers are absorbed via the gastroin-testinal tract more quickly than the hydrophilic beta blockers.
Route of Elimination
Beta blockers are eliminated by hepatic metabolism, urinary excretion, and other poorly defined mechanisms.
Duration of Action
The duration of action is related to half-life and varies markedly in these drugs. The variation in plasma half-life results from the variation in elimination rates and routes. This in turn is related to lipid solubility. Several of the short half-life drugs have been developed in slow-release formulations to allow once-daily administration with better compliance for long-term medication regimen. The patient with an acute myocardial infarction with a rapidly changing hemodynamic status requires an ultra-short-term half-life beta blocker. Several of these are also on the market (Esmolol).
Hemodynamic Effects
The hemodynamic effect of treatment with a beta blocker is dependent on the agent used, the mode of administration, and the patient's cardiovascular status. Generally, the beta blocking agents create a negative chronotropic and inotropic effect. Acute administration results in a slowed heart rate, a reduced cardiac output, an insignificant change in stroke volume, and a transient increase in systemic vascular resistance. In patients who are normotensive, the systemic arterial blood pressure is usually unchanged. This acute response is similar in both the cardioselective and the nonselective agents. The acute increase in systemic vascular resistance probably results from a compensatory mechanism secondary to the reduced cardiac output. With continued beta blocker therapy, the reduction in cardiac output and heart rate is sustained, but the increased systemic vascular resistance readjusts to pretreatment level or below, resulting in a decreased arterial pressure. This occurs in days to weeks after treatment is originated.
The sympathetic nervous system affects renin release. Beta blockers inhibit the sympathetic effect on renin release and decrease the plasma renin activity. This effect is particularly noticeable within minutes of intravenous administration. All of the beta blockers reduce plasma renin activity.
Electrophysiologic Activity
Beta blockers depress normal and ectopic pace-maker activity and slow conduction in the atrioventricular node and in accessory pathways. They also increase the threshold for ventricular fibrillation in ischemic and nonischemic myocardium.
Beta blockers are among the most widely used classes of drugs. The more serious adverse effects result directly from the beta blockade. For some of these drugs, the sympathomimetic activity modifies the side effects.
Adverse Effects
- Congestive heart failure, bradycardia, hypoten-sion, and atrioventricular block are side effects resulting directly from cardiac beta blockade.
- Pulmonary side effects such as bronchospasm may occur. This adverse effect is often present in patients with asthma or obstructive pulmonary diseases. Nonselective beta blockers and high doses of cardioselective beta blockers are contra-indicated in asthmatic patients.
- Fatigue is a side effect of beta blockade that may result from the hemodynamic effects of the drugs. Another theory suggests that fatigue results from peripheral metabolic effects such as a fall in blood glucose levels and inhibition of lactic acid release from skeletal muscles.
- Peripheral vascular impairment may be aggravated or precipitated by beta blockers. In hypertensive patients, cold extremities and absent pulses were a problem. The incidence of this adverse effect was found to be less in patients treated with a cardioselective beta blocker or one with intrinsic sympathomimetic properties. The beta blocking agent decreased blood flow in muscle in patients with peripheral vascular disease and intermittent claudication.
- Beta blockers may aggravate or precipitate coronary artery spasm by blocking beta2 adrenorecep-tor-mediated coronary vasodilatation and leaving the alpha adrenergic-mediated coronary vasocon-striction unopposed.
- Central nervous system adverse effects are usually dose-related and frequently disappear with a prolonged medical regimen. Included are vivid dreams, insomnia, hallucinations, depression, dizziness, lightheadedness, time distortion, and short memory loss.
- Insulin dependent diabetics as well as non-diabetic patients have experienced hypoglycemia resulting from the effect of a nonselective beta blocking agent on glucose metabolism.
- Tremors and muscle cramps have been described.
- A variety of gastrointestinal effects are reported: nausea, diarrhea, anorexia, constipation, vomiting.
- Beta blockers tend to elevate plasma levels of triglycerides and low density lipoproteins and to lower plasma levels of the high density lipoproteins. This effect is more pronounced when non-selective agents are used. It is believed to result from unopposed peripheral alpha adrenergic stimulation.
Withdrawal Syndrome
Abrupt withdrawal of beta blockers results in rebound phenomena, including tachycardia, hypertension, and myocardial ischemia. The withdrawal symptoms are not consistent, however, and vary with the drug in use.
Beta Adrenoreceptor Blocking Agents Propranolol (Inderol)
Propranolol's use as an antihypertensive medication probably results from the drug's ability to reduce cardiac output, force of contraction, renin secretion, and central sympathetic tone. Propranolol is not cardioselective; it blocks both beta1 and beta2 receptors. Blocking the beta1 receptors reduces heart rate and myocardial contractility, leading to a lowered blood pressure. The antiarrhythmic effect (this drug is the prototype for Class II antiarrhythmic drugs) stems from the drug's action to reduce the sinus rate, decrease the spontaneous rate of depolarization of ectopic pacemakers, and slow conduction both in the atria and the AV node. The drug's action to reduce heart rate and contractility aids in the reduction of anginal pain by reducing total coronary blood flow and myocardial oxygen demand. Propranolol must not be abruptly withdrawn. Beta blockers create problems of susceptibility to circulating catecholamines. The patient may experience an increase in anginal pain and myocardial infarction. Hypertensive patients may have life-threatening rebound elevated blood pressure. Problems may arise immediately or within a few days after abrupt withdrawal.
Nonselective beta blockers are contraindicated in asthmatic patients because of the possibility of increased airway resistance.
Acebutolol (Sectral)
Acebutolol is a cardioselective blocker with intrinsic sympathomimetic activity. It is used in the treatment of angina pectoris, hypertension, and ventricular arrhythmias. In recent testing, it has been shown to improve the hemodynamic status of patients with congestive cardiomyopathy. This drug reduces heart rate and blood pressure at rest and during exercise. It sometimes suppresses or does not affect the renin-angiotensin system. The antiarrhythmic effect occurs by blockage of adrenergic stimulation on cardiac impulse generation and conduction. The prolongation of His-Purkinje conduction helps in the suppression of ventricular arrhythmias. The arrhythmic use is primarily for ventricular arrhythmias. This drug has reduced adverse effects common to the other beta blockers because of its intrinsic sympathomimetic activity.
Atenolol (Jenormin)
Atenolol is probably used as an antihypertensive agent because of its ability to decrease sympathetic activity in peripheral vasculature, antagonize catecholamines, and decrease renin secretion.30 The exact mechanism is not known. Atenolol is a cardioselective agent with the beta1 blocking traits of propranolol. Antiarrhythmic activity includes its use to treat sinus tachycardia and persistent atrial extrasystolic and tachycardiac rhythms.
Alprenolol
Alprenolol is a cardioselective beta blocker drug that is used to treat rapid heart rates. It slows heart rate with its chronotropic effect. This is a long-action beta blocker administered one time daily. The incidence of adverse effects is reduced. This drug slows atrial ectopic and sinus automaticity and prolongs junctional conduction activity.
Carteolol
The beta blocker carteolol is a partial agonist; it has some beta simulating action. It seems to enhance SA nodal automaticity in some instances. However, with catecholamine-enhanced activity, the beta blockage alone comes into play, and carteolol is more effective than propranolol in depressing SA node automaticity. The antihypertensive activity of the drug is in reduction of both systolic and diastolic blood pressure. Carteolol is titrated by response. There are limited adverse effects because a low dose is effective. This drug is still being researched.
Esmolol
Esmolol is a new ultra-short-action cardioselective beta blocker. Its elimination half-life is just over 9 minutes. It is administered intravenously, and the beta blockage is gone within 15 minutes after termination of the infusion. Recent research in the use of esmolol has shown that it decreases infarct size and heart rate. It is thought that this drug may be useful in reducing myocardial oxygen consumption in patients with acute myocardial infarction. Its special short-term features also make it potentially useful during the preoperative period for the patient experiencing coronary artery bypass surgery. In other in-vestigational studies, atrial fibrillation has been converted to sinus rhythm and ventricular rates have been reduced, particularly in the postoperative period for cardiovascular surgery patients.
Bucindolol
Bucindolol is a new, recently introduced agent that combines beta adrenoreceptor blocking properties with a direct vasodilatory effect. Recent studies have found the drug to be an effective antihypertensive medication. The drug is relatively cardioselective and seems to be about 30 times as potent as propranolol in blocking beta1 receptors. It also shows a mild intrinsic sympathomimetic activity. Bucindolol was shown to lower elevated blood pressure in several studies, reducing systolic and mean arterial pressure.
Bucindolol's very rapid onset of action makes it different from other beta blockers. This effect is thought to be a result of its direct vasodilator activity. One side effect, differing from other beta blocker agents, is the increase in plasma renin activity. Bucindolol is absorbed from the gastrointestinal tract after oral administration. Intravenous administration of the drug as well as oral dosage is now in the investi-gational stage. Side effects are reported to be mild and infrequent. Significant bradycardia is not found. The main adverse effects were dizziness, tiredness, and muscle weakness during exercise.
Labetalol (Trandate, Normodyne]
Labetalol is a recently developed agent with al-phai and beta adrenergic blocking properties as well as direct vasodilating activity. It is a noncardioselec-tive beta blocker. Labetalol is a potent antihypertensive agent effective in treating all levels of elevated blood pressure, including hypertensive crises and hypertension resistant to other drug regimens. It is also effective with the hypertension related to pheochro-mocytoma and renovascular hypertension. In patients with stable angina, Labetalol functions as a beta blocker, reducing myocardial oxygen demand, and as an alpha adrenergic blocker, decreasing neurogenic coronary tone and preventing coronary vasoconstric-tion. Labetalol's alpha1adrenoreceptor inhibitor activity is very similar in action to prazosin. The alpha
1 adrenoreceptor is the receptor of vascular smooth muscle; its blockade by Labetalol produces a decrease in peripheral vascular resistance. This drug has no effect on platelets, indicating that it does not affect the alpha2 receptors, which are the alpha receptors found in platelets. At this time its antiarrhythmic properties are being investigated. There are no adverse reactions after withdrawal of Labetalol. The rebound phenomenon noted with other beta blockers is not reported.
The incidence of side effects of Labetalol is similar to other beta blockers, but heart failure, postural hy-potension, bronchospasm, and vivid dreams are less often reported. Postural hypotension occurs in 58% of patients following the IV administration if the patient is allowed to assume a vertical position. This occurs with doses over 1,gm daily. Although uncommon, Raynaud's phenomenon can occur.
Metoprolol (Lopressor)
Metoprolol is a cardioselective beta blocker. This drug resembles propranolol in other aspects, such as in the indications for use, action, and adverse effects. The effectiveness of the drug is probably related to decreased sympathetic peripheral activity, decreased renin activity, and negative inotropic and chronotropic activity. It is used to treat mild to moderate hypertension.
Nadolol (Corgard)
Nadolol is used in the treatment of hypertension. This beta antagonist is nonselective. It is a negative inotropic and chronotropic drug. Its antihypertensive effect is probably due to its ability to decrease sympathetic flow in the periphery, reduce heart rate and contractility, and decrease renin secretion.
Oxprenolol (Jrasicor)
Oxprenolol is a nonselective beta blocker with intrinsic sympathomimetic activity.52 The agent is used in the treatment of angina pectoris, hypertension, and arrhythmias. Oxprenolol produces a decrease in resting heart rate, but the decrease is not as profound as that produced by propranolol. Oxprenolol is safer for older patients with bradycardia. Although it has a negative inotropic effect, it is not as deleterious as other beta blockers, possibly because of the sympathomimetic activity. Oxprenolol has been shown to affect right ventricular performance to the same extent as propranolol in the hypertensive patient. Like other beta blockers, Oxprenolol suppresses the renin-angiotensin system.
Used as a treatment for angina, the mechanism of action is the reduction of myocardial oxygen demand, the result of a decrease in the heart rate, and of myocardial contractility. The antiarrhythmic effect of the agent occurs by preventing excessive sympathomimetic activity and prolonging AV conduction. Oxprenolol can convert supra ventricular arrhythmias to sinus rhythm, and it controls the ventricular rate. It is effective against multifocal ventricular ectopic beats or brief runs of ventricular tachycardia (VT) in patients with CAD or MIs.
Pindolol (Visken)
Pindolol is a potent nonselective beta adrenergic blocking agent used for the treatment of hypertension. As do other beta blockers, this drug possesses potent intrinsic sympathomimetic activity. It is effective in the treatment of hypertension. Because pindolol has intrinsic sympathomimetic activity (partial agonist), it is preferred sometimes to other beta blockers.
Pindolol slows heart rate and lowers systolic and diastolic blood pressure at rest and during exercise. The activity of pindolol on blood pressure probably results from its effect on heart rate, cardiac output, and peripheral resistance. It slows heart rate and depresses myocardial contractility, but because of the partial agonist effect, the slowing of the heart rate is less than that caused by other beta blockers. It is used alone or in combination with a diuretic in the treatment of hypertension. Pindolol is not currently approved by the FDA for antianginal treatment.
Its use as an antianginal medication is related to the hemodynamic mechanisms involved in the reduction of myocardial oxygen demand. Additionally, the vasodilator properties of pindolol may play a role in its antianginal effect by inducing afterload reduction or coronary vasodilatation.
The intravenous and oral use of pindolol to treat arrhythmias has shown the drug to be effective in converting paroxysmal supraventricular tachycardia, atrial fibrillation, and atrial flutter to sinus rhythm. It has also been shown to control the ventricular rate in patients with atrial fibrillation who did not convert sinus rhythm. Pindolol should not be abruptly withdrawn because it may, as in the cases of other beta blockers, produce withdrawal symptoms. However, its intrinsic sympathomimetic activity results in some adrenergic stimulation during treatment with the drug. This may prevent the adrenergic supersensitiv-ity that is a mechanism of beta blocker withdrawal syndrome.
Sotalol (Sofacor)
Sotalol is a nonselective beta adrenergic receptor blocking agent without intrinsic sympathomimetic properties. It is unique among beta blocker drugs in its ability to prolong repolarization. Sotalol is a Class III (see antiarrhythmic drugs) antiarrhythmic drug in addition to having beta blockage properties. It is used for treatment of hypertension, angina pectoris, and arrhythmias. In patients with coronary artery disease or arrhythmias, Sotalol increases the spontaneous sinus node cycle length and slows the sinus rate. It is also shown to prolong conduction time in the AV node.
The side effects of Sotalol are similar to those of the other beta blockers. Additionally, the antiarrhythmic effect is associated with QT prolongation and myocardial depression.
Contraindications for the use of Sotalol include the usual ones for beta blockers—heart failure, brady rhythm, hypotension, and obstructive lung disease. Also, it is not recommended in patients who have a prolonged QT interval.
Timolol (Biocadren)
Timolol is a nonselective beta blocking agent used in the treatment of hypertension, angina pectoris, supraventricular arrhythmias, and tachyarrhy-thmias.30 Timolol probably has many of the antihypertensive properties of other beta blockers, decreasing renin secretion and sympathetic flow in the periphery and antagonizing catecholamines.
Nursing Management
Priorities when administering a beta adrenergic receptor blocking agent are:
- Take pulse before each administration and record.
- Determine cardioselectivity of drug to recognize signs of bronchospasm.
- Identify patients at risk for beta2 blockage respiratory problems.
- Withhold and verify instructions for dosage in patients with advanced degrees of heart block, cardiogenic shock, and right ventricular failure resulting from pulmonary hypertension.
- Monitor blood pressure and apical pulse before initial dose.
- Monitor blood pressure, heart rate, and rhythm every hour with IV administration of beta blockers.
- Assess lung sounds; assess for dyspnea with IV administration.
- Monitor orthostatic blood pressures if beta blockers are given concurrently with other antihypertensives.
- Assess lungs every 4 hours for rales and heart sounds for development of extra heart sounds—an S3 or S4.
- Monitor the slow withdrawal of beta blockers for rebound effect.
- Provide patient education for side effects of beta blockers; stress the need to remain on the medication with no abrupt stops and the need to adhere to an on-time schedule of medication.
- Monitor intake and output and daily weights.
- Give food with some of the beta blockers (for example, with propanolol).
|
|
CALCIUM CHANNEL BLOCKING AGENTS
Calcium channel blocking agents have several uses in the treatment of cardiovascular problems.43, 79 In recent years, the number of these agents has grown rapidly.56 They have been found to be effective in treatment of angina pectoris and hypertension, and they are effective as antiarrhythmia agents.85 The slow calcium channel is responsible for the Phase 2 plateau of the cardiac cell action potential. Primarily, the effect is seen in SA and AV nodal tissue activity. The main calcium antagonists in clinical use in the last decade are verapamil, nifedipine, and diltiazem. Many derivatives of these drugs have been evaluated in recent studies. There are marked differences in the various calcium antagonists in regard to chemical structure, type of effect, and site of effect.59
The calcium channel blocking agents can be arbitrarily divided into classes on the basis of chemical configuration. This gives us five main types.
Type 1
Type 1 calcium antagonists are the papaverine derivatives with myocardial and vascular effects. This group includes three agents: verapamil, gallopamil (D-600) and tiapamil. Verapamil is the prototype. All of these agents are moderately potent peripheral and coronary vasodilators. Their predominant action is to lengthen conduction time and prolong refractoriness in the AV node. These are the properties that account for their antiarrhythmic effects in treating supraven-tricular tachycardias.
Verapamil
Verapamil is the drug of choice to terminate acute episodes of supraventricular tachycardia (SVT). It is also effective in the treatment of coronary artery spasm. The IV bolus for SVT is 5-10 mg over 2-3 minutes, and dosage ranges from 80-160 mg every 6-8 hours. Adverse effects include hypotension, edema, headache, and flushing with IV administration. Heart block is also reported. Concurrent administration of propranolol and IV verapamil is contrain-dicated.
Gallopamil
Gallopamil is used to treat angina. It is under investigation as an antiarrhythmic. It is shown to dilate arteries and veins, producing reduced peripheral artery resistance. Administered orally, the dosage is 50-100 mg TID, with side effects similar to verapamil.
Tiapamil
Tiapamil, an antihypertensive, antianginal, and antiarrhythmic agent, is a calcium blocker that reduces systolic and diastolic blood pressure and angina symptoms, evidenced by the disappearance of ST segment depression. It has shown a propensity to enhance peripheral vasodilatation, with a marked reduction in afterload. The protocol calls for oral administration of 600 mg/d in divided doses.
Type 2
The Type 2 calcium antagonists, the dihydropyri-dine derivatives, with vascular effects are the agents similar to nifedipine, the prototype. As a group they are potent vasodilators rather than agents that affect the myocardium. Therapeutic considerations for the use of these agents is in the treatment of hypertensive emergencies, the long-term treatment of essential hypertension, and the therapeutic regimen for angina.
Nifedipine
Nifedipine is used to treat variant angina, classical angina, coronary artery spasms,3 and systemic hypertension.32 The overall effect achieved by this drug in the treatment for angina is the improvement of the oxygen supply-demand ratio, which occurs as an increase in oxygen supply and a decrease in demand with a possible improvement of oxygen use. Nifedipine increases oxygen supply by (1) inhibiting coronary artery spasm; (2) dilating epicardial coronary arteries with increased coronary blood flow; (3) increasing collateral coronary circulation by affecting the dilatation of the epicardial coronary arteries; and (4) reducing coronary resistance by dilating coronary arterioles.40 Nifedipine reduces oxygen demand by (1) afterload reduction due to a decreased peripheral resistance; (2) reduction of preload and cardiac volumes in some cases; (3) a direct negative inotropic effect; and (4) a direct effect on metabolism, resulting in reduced ischemia and improved performance even without increased coronary blood flow. Oxygen use in the mitochondria may be improved with this effect.
One of the most therapeutic properties of nifedipine is coronary artery vasodilatation. The drug is effective in relieving and protecting against ischemic episodes during coronary artery spasm. Nifedipine is a relatively selective dilator of resistance vessels, with little effect on capacitance vessels. It is useful in treatment of systemic arterial hypertension. One advantage is that it does not exaggerate cardiac function and has very slight effect on acceleration of heart rate. Reported side effects of nifedipine are as follows: (1) It may exacerbate angina in patients with coronary artery disease, possibly because of the slight increase in heart rate and the decrease in arterial pressure and coronary perfusion pressure caused by the drug. This reaction is usually seen at the time of dosage changes or at the start of therapy. (2) Congestive heart failure may result from the decrease in perfusion; particularly susceptible are patients treated with beta blockers or patients with severe aortic stenosis who have fixed impedance to flow across the aortic valve. (3) Peripheral edema may occur in the lower extremities. This effect is dose-related; it is not related to congestive heart failure or sodium retention. It probably results from selective dilatation of renal arterioles and precapillary sphincters, causing elevation of capillary filtration pressure. The addition of a diuretic will alleviate this effect. (4) Dizziness, lightheadedness, headache, and fatigue resulting from the vasodilatation may occur. (5) Flushing and heat sensation, probably due to nifedipine-induced vasodilatation, may occur. (6) Hypotension, excessive decrease in blood pressure, is rare and dose-related, occurring with increased dose or at initial titration. (7) Muscle cramps and tremors may occur. (8) Dose-related syn-copal episodes have been reported in a small number of patients. (9) Marked gingival hyperplasia similar to the hyperplasia caused by dilantin may occur, but with only minimal inflammation.
Nisoldipine
This new calcium channel antagonist is structurally similar to nifedipine. In its high vascular selectivity, nisoldipine differs from most clinically used calcium antagonists.49 Nisoldipine is beneficial in the treatment of patients with CAD and hypertension. This agent is possibly the most potent calcium antagonist available for treatment of coronary artery spasm.82 It is 4 to 10 times more potent than nifedipine in relaxing smooth muscle. It has also been shown to relieve coronary artery spasm induced by K+ and to increase coronary blood flow in arteries with spastic segments. Lower doses of nisoldipine produced better results as compared with larger doses of nifedipine or nitroglycerin. This agent is also effective in reducing blood pressure. The antihyper-tensive effect of nisoldipine probably results from peripheral arteriolar vasodilatation. The average dose is 10 mg BID orally. This agent is relatively free of adverse effects, although one reported effect is short-term tachycardia.
NItrendipine
Nitrendipine is another new calcium antagonist related to nifedipine. It acts predominantly on peripheral vasculature and has been shown to be an effective antihypertensive agent. It acts by peripheral vasodilatation.87 It appears to have a beneficial effect on coronary collateral circulation. Nitrendipine is highly selective for smooth muscle, with no significant effect on the SA node. The hemodynamic effect of nitrendipine mainly results from its vasodilatory properties. It has special value in treatment regimens of patients with high systemic resistance and low re-nin level hypertension. Because cardiac performance is not reduced by administration of nitrendipine, it can be given in combination with beta blockers.
Nimodipine
Nimodipine is yet another new calcium antagonist related to nifedipine. It has a relatively selective dilatory effect on cerebral vasculature, with minimal effect on other vascular beds and on systemic arterial pressure. It is perhaps a potentially beneficial drug in the treatment of cerebrovascular disease such as cerebral arterial spasm.
Nicardipine
Nicardipine is a potent Type 2 vasodilator. It has vasodilator and electrophysiologic properties that are also similar to nifedipine. This agent is selective for coronary and cerebral vessels. The effect of nicardi-pine on vascular smooth muscle was found to be more potent than that of nifedipine, verapamil, or diltiazem. It is selectively potent in its action on the blood vessels of the heart and is used to treat angina. Nicardipine decreases the spontaneous rate of the SA node. It also prolongs the refractory period of the AV node. There are little or no antiarrhythmic properties at therapeutic levels.
Felodipine
Felodipine is a new Type 2 calcium antagonist that interferes with intracellular calcium use in vascular smooth muscle. It appears to have a direct and selective relaxing effect on vascular smooth muscle cells, particularly the resistance vessels. The vasodi-lating effect of felodipine decreases systemic vascular resistance and systolic and diastolic blood pressure, increases cardiac output, and induces reflex increases in heart rate. It has also shown to be effective in treatment of angina pectoris and cardiac failure.45 Felodipine does not increase heart rate in the presence of congestive failure, possibly because of higher pre-treatment heart rates in patients with congestive failure. Congestive heart failure is improved with this drug because systemic vascular resistance is reduced, as is left ventricle end diastolic pressure (LVEDP). Improvement occurs at rest or with exercise. Felodipine is used primarily for treatment of hypertension and congestive failure. It produces an acute hemody-namic improvement in patients with congestive failure. Felodipine has a marked diuretic effect, possibly due to increased renal blood flow. It is compatible with beta blockers and diuretics in treating hypertension.
Reported side effects are mild to moderate: (1) Headache is the most common, following the first dose; (2) flushing due to peripheral dilatation may occur; (3) palpitations also may occur after the first dose; and (4) ankle edema is common.
Type 3
Type 3 calcium antagonists, the benzothiazine derivatives, have both myocardial and vascular effects. Type 3 includes only one drug—diltiazem. This agent is used to treat variant angina and classical angina. It has shown some antiarrhythmic properties in treatment of SVT. Diltiazem has negative chrono-tropic and dromatropic features. The adverse effects reported include bradycardia, sinus arrest, and hypo-tension. The vasodilator effects are less frequent, but there have been reports of dependent edema, headache, and dizziness.
Type 4
Type 4 calcium antagonists, the piperazine derivatives, are little known. In addition to their calcium channel blocking effects, they also show signs of his-tamine blockade. This group, with two identified agents, is highly selective for calcium channels in vascular smooth muscle rather than in cardiac muscle.
CInnarizine
Cinnarizine shows some potential for vasodilata-tion; it increases peripheral blood flow and decreases whole blood viscosity. It may be of use in treating occlusive peripheral vascular disease, intermittent claudication specifically. It is still under investigation.
Flunarizine
Flunarizine is a similar derivative of cinnarizine, with similar use in treatment of occlusive peripheral vascular disease.
The reported adverse effect of both cinnarizine and flunarizine is a sedative effect.
Type 5
The Type 5 calcium antagonists, the complex pharmacologic group, are those of varying structures and effects. This group includes those that have a selectivity of action either for vascular tissues (e.g., lidoflazine) or for both cardiac and smooth muscle (e.g., perhexiline and bepridil), while also having the propensity to block the fast sodium channel in the heart. These agents react differently in therapeutic situations, particularly in the control of cardiac arrhythmias. Overall, these drugs act to dilate coronary vessels and peripheral vessels.
Bepridil
Bepridil, a new antianginal, antiarrhythmic agent, acts by inhibiting the inward calcium channel. Bepridil inhibits slow inward current and reduces amplitude and duration of the action potential in the SA node. It has been shown to increase coronary blood flow and decrease myocardial oxygen consumption. The drug also has a lidocaine-like effect on the fast sodium channel. Bepridil is considered to have three pharmacologic properties: It is membrane stabilizing, calcium antagonistic, and has some Class I antiarrhythmic qualities. Its effect on heart rate is to produce a marked bradycardia. The IV injection produces transient hypotension with peripheral vasodil-atation. This effect is short-lived—about 5 minutes. It is NOT accompanied by tachycardia. Bepridil is used to treat angina. It will decrease oxygen consumption and elevate blood flow. In acute myocardial infarc-tion, bepridil improves resolution of the MI when administered in the IV form. Bepridil is incorporated in treatment regimens for control of ventricular arrhythmias and the suppression of atrial and ventricular ectopic beats, as well as to suppress VT. The antianginal effect is found in the vasodilator activity. Reported adverse effects'are (1) excessive tachycardia and (2) hypotension after intravenous administration. Tremors and gastrointestinal problems occur with oral administration.
Lidoflazine
Lidoflazine is another of the calcium channel blocking agents with some fast channel blocking properties. Primarily a vasodilator, it appears to have some antiarrhythmic features also. Lidoflazine is a long-action coronary artery dilator. The antiarrhythmic activity is specifically in treatment of atrial arrhythmias. It is being investigated as a pharmacologic cardib version agent in atrial fibrillation. The reported adverse effects are the occurrence of PVCs and VT in patients with congestive heart failure who have been treated with digoxin. Lidoflazine is still under investigation.
Perhexiline, another calcium antagonist under investigation, is also an antianginal agent. The mechanism for its antianginal effect is not clearly understood. This drug reduces heart rate but delays relief of artery spasm. The reported adverse effects include (1) hepatic dysfunction; (2) peripheral neuropathy; (3) ataxia, dizziness; (4) papilledema; and (5) nausea and weight loss.
Nursing Management
Priorities when administering a calcium channel blocking agent are:
- Monitor blood pressure every V2-1 hour for initial administration of oral or intravenous verapamil and the oral doses of nifedipine and diltiazem.
- Take blood pressure recordings every 10-15 minutes for the first hour if intravenous bolus of verapamil is administered.
- Tell patient about the possibility of increased anginal pain when calcium blockade begins.
- Monitor apical pulse with radial.
- Assess every Vi-\ hour for complications such as initial hypotension, which is usually transient with the calcium blockers.
- Report continued hypotension that becomes symptomatic or signs of AV block.
- Be aware that nifedipine and verapamil can potentiate the action of digitalis, raising serum levels. Assess for any signs of digitalis toxicity,
- Check for interaction if patient is also on beta blacker or other antihypertensive drugs.
- Use cautiously with CVA patients, because of the vase-dilatory effects of the drugs.
- Assess for early signs of heart failure (e.g., edema) at least every 8 hours.
- Provide patient education for drug dosage, schedules, and interaction with other medications used concurrently.
- Regulate activity for relief of the signs of fatigue that accompany nifedipine.
- Provide comfort measures to relieve the flush sensations that occur.
- Give pain medication for the side effect of headache.
- Caution patient about sedative effects of the Type 4 agents.
|
|