n ENDOSSEOUS, blade (plate) form:
- • Adequate bone to support the implant with width and length being the primary
dimensions of concern.
- • Maxillary and mandibular arch locations.
- • Completely or partially edentulous patients.
n ENDOSSEOUS, ramus frame:
- • Adequate anterior bone to support the implant with width and height being the
primary dimensions of concern.
- • Mandibular arch location.
- • Completely edentulous patients.
n SUBPERIOSTEAL, complete, unilateral, circumferential:
- • Atrophy of bone but with adequate bone to support the implant.
- • Maxillary and mandibular arch locations.
- • Completely and partially edentulous patients.
- • Stable bone for support.
n TRANSOSTEAL, staple, single pin, multiple pin:
- • Adequate anterior bone to support the implant with width and height being the
primary dimensions of concern.
- • Anterior mandibular arch location.
- • Completely and partially edentulous patients.
v
What Are the Requirements for Surgical, Restorative, and Periodontal Management of
Patients With Dental Implants?
Implant treatment is delivered in several ways: (1) by multidisciplinary teams of
dentists in which an oral surgeon or periodontist performs the surgical component of the
implant and a prosthodontist performs the prosthetic component; (2) by individual
implan-tologists with extensive training in both the surgical and prosthetic components
who perform all aspects of the procedure; and (3) by general dentists who may perform
both components or the prosthetic component only and whose training in implant techniques
may vary widely.
Unfortunately, there are no data available to the panel that address the surgical,
restorative, and periodontal requirements for the individuals managing the implant
patient.
Minimal training has not been precisely defined, but the panel recommends that the
individual that assumes the surgical treatment phase be well prepared in accepted
surgical methodologies. In as much as the restorative procedures employed in implantology
differ from those in traditional restorative dentistry procedures, the panel recommends
instruction in the restorative phase of implantology. These programs also should include
expertise in short- and long-term tissue maintenance addressing gingival status as well
as radiographic evaluation of tissue support.
Patient selection should be restricted to those patients who show a need and
motivation for the implant procedures. The evaluation of the recipient should include a
survey of adequate bone structure, medical history, and, where indicated, medical
laboratory studies and consultation with the patient's physician. The use of computerized
tomography for evaluation of maxillary and mandibular anatomy is suggested when more
accurate information regarding implant placement is needed. The patient's dental
evaluation also should include a psychosocial appraisal of his or her suitability for
implant procedures when psychological symptoms are present.
The panel supports a multidisciplinary approach, and we recommend a preimplant
consultation involving the professional participants with the patient. Postimplant
procedures should include communication, monitoring, and collection of recorded data by
the professional. We recommend that the patient be thoroughly instructed in maintenance
therapy with the understanding that the patient serves as a cotherapist.
There is a lack of data detailing the minimum requirements for an adequate maintenance
program. The proper recall interval, methods of plaque and calculus removal, and use of
antimicrobial agents are critical variables that need further evaluation.
v
What Are the Health Risks of Dental Implants?
There are at least three areas in which the assessment of patient risk should be
considered, including risks associated with the surgery and/or anesthesia, psychological
risks, and medical risks. Risks associated with the surgical procedure may include
inadvertent perforation of the nasal sinus, local and systemic infection, and nerve
injury. Before surgery a medical history should be taken to evaluate the history of the
presenting problem and chief complaints. A review of the current status of the patient's
organ systems should be made.
Children need special consideration, given long-term morbidity concerns, requirements
of growth, manual dexterity, and coping skills.
Psychological stressors and motivational factors have been shown to influence patient
response to surgery and long-term compliance with oral hygiene maintenance. These
stressors include both familial and social environmental factors such as job
satisfaction, financial status, and health concerns. Specific mental conditions may
require psychological intervention to assist with patient cooperation and outcome
satisfaction. Individuals with excessive neurotic concerns, depression, anxiety, and
specific medical fears or previous negative medical or dental experiences should be
appropriately evaluated. Relative contraindications include individuals with psychotic
symptomatology, especially requiring psychotropic medication, and somatization disorders
or chronic pain complaints where medical symptoms are exhibited in the absence of organic
evidence. Tobacco use, alcohol, or drug dependency may interfere with good nutrition or
compliance requirements.
Temporary conditions that may result from implant placement may include pain and
swelling, speech problems, and gingivitis. Long-term problems may include nerve injury,
local bone loss exacerbation, hyperplasias, local or systemic bacterial infection, and
infectious endocarditis in susceptible individuals, including those with body part
replacement. Existing natural dentition may be compromised.
Factors related to prediction of health risks need to be continuously assessed before
the surgical decision, after implantation, during the temporary waiting period, following
the loading period, and at 6-month intervals throughout the followup period. Reliable and
valid standardized measurements sensitive to both psychological and physical factors
should be used in clinical prospective studies to enhance comparison across studies.
v What Are the Future Directions for Research On Materials and Designs of Dental
Implants and On Clinical Management?
Materials and Designs
Dental implants have many compositions and surface textures. Manufacturing processing
techniques affect these surfaces in subtle ways. To better control clinical protocols,
characterization of these surfaces is essential. Ion release from the implant may
influence biocompatibility (bioacceptance). To achieve a more complete understanding of
tissue response to the implant, basic experiments in host-implant physiology and biology
must be continued. Dynamic studies in laboratory animals also should be completed. Other
matters that warrant further study are the influence of surface preparation on
wettability or bonding of tissues to the implant and the effect of galvanic couples
resulting in corrosion. Studies must document the possible release of constituents of
implant materials at the trace and subtrace level into other tissues to determine
their significance with respect to toxicity, mutagenicity, or carcinogenicity.
Basic research should be emphasized to develop materials and methodology to allow for
predictable bone augmentation. The implant- host interface should be studied to
characterize wound repair and tissue adaptation in the peri-implant region.
Among the factors involved in the design of an implant are the force components
produced during loading, the dynamic nature of loading, and the mechanical and structural
properties of the prosthesis of stress transfer to tissues. Unfortunately, accurate data
on such parameters are incomplete. Such information is essential for efficient design of
implants.
Clinical Management
Randomized, controlled, prospective multicenter clinical studies should be initiated.
These studies should investigate the role of several factors on the long-term
effectiveness of dental implants. These factors include, in addition to implant
characteristics, the operator's skills in implant placement, tissue management, various
patient characteristics, including the intraoral location of the implant, and occlusal
and prosthetic considerations.
The panel feels that one important method of accumulating accurate data on implant
performance is to establish a National Dental Implant Registry, which will standardize
reporting forms to collect information on this activity in the United States. A rating
scale based upon function and discomfort should be developed for evaluation of all
implant procedures. In this way, the causative factors involved in success and failure of
implants can be more accurately identified. Consideration also should be given to the
establishment of centers for training, treatment, and research in dental implantology.
To ensure continued safety evaluation of dental implants, long-term prospective
studies should specifically address failures due to medical or psychological
complications that led to premature removal of the implant. When failures occur in either
implants or an existing dentition, a failure analysis should be performed and reported.
All patient data should be recorded, including age, education, socioeconomic level,
number of previous implants, nutritional status, periodontal status, acute or chronic
coexisting diseases, and pharmacologic use.
Patient Considerations
Considering that edentulousness is frequently the result of the patient's high
susceptibil
ity to destructive forms of periodontal disease, the relationship of implant success
rates to the patient's relative susceptibility to periodontitis should be studied. Also,
data are needed on both the acute and chronic or long-term morbidity that may result from
various types of implants.
The public is entitled to educational materials that enable informed participation in
implant treatment decisions, and the panel recommends that these materials be developed.
Conclusion
During the 10 years since the first Consensus Development Conference on Dental
Implants, a great deal of activity in the field has occurred with the development of
better materials and newer techniques that have resulted in improved implant-bone
interface. This conference examined case series studies, and the panel concluded that a
large proportion of endosseous, subperiosteal, and transosteal implants have remained in
place for more than 10 years. The indications and contraindications of various types of
dental implants have been described. The complexity of the surgical, restorative, and
periodontal procedures used to successfully insert and maintain dental implants
demonstrates the need for a multidisciplinary approach in this field.
Long-term studies that concurrently compare various types of implants are needed to
provide information beyond mere survival rates. Functional success of various implants
should include such criteria as the ability to support fixed or removable prostheses in
the absence of discomfort, the presence of satisfactory esthetics, and clinical and
radiographic evidence of tissue health. A suggestion for the establishment of a National
Dental Implant Registry was proposed with the objective of collecting data and
documentation on various procedures being conducted in the United States. Future studies
in materials and techniques were proposed.
Consensus Development Panel
D. Walter Cohen, D.D.S.
Conference and Panel Chairperson
President
The Medical College of Pennsylvania
Philadelphia, Pennsylvania
James D. Beck, Ph.D.
Professor and Chairman
Department of Dental Ecology
University of North Carolina at Chapel Hill
School of Dentistry
Chapel Hill, North Carolina
Chester W. Douglass, D.M.D., Ph.D.
Associate Professor and Chairman
Department of Dental Care Administration
Harvard School of Dental Medicine
Boston, Massachusetts
Manville G. Duncanson, Jr., D.D.S., Ph.D.
Professor and Chairman
Department of Dental Materials
University of Oklahoma College of Dentistry
Oklahoma City, Oklahoma
Lawrence J. Emrich, Ph.D.
Cancer Research Scientist
Department of Biomathematics
Roswell Park Memorial Institute
Buffalo, New York
Max A. Listgarten, D.D.S.
Professor and Chairman
Department of Periodontics
University of Pennsylvania School of
Dental Medicine
Philadelphia, Pennsylvania
Barbara G. Melamed, Ph.D.
Professor of Psychology
Departments of Clinical and Health
Psychology and Community Dentistry and
Psychiatry University of Florida College of Health
Related Professions Health Sciences Center
Gainesville, Florida
Carl E. Misch, D.D.S.
Codirector
Oral Implantology Center
University of Pittsburgh School of Dental Medicine
Director Misch Implant Institute
Dearborn, Michigan
Ralph W. Phillips, D.Sc., M.S.
Research Professor of Dental Materials
Indiana University School of Dentistry
Indianapolis, Indiana
Mary Kaye Richter
Executive Director
National Foundation for Ectodermal Dysplasias
Mascoutah, Illinois
Elaine A. Stuebner, D.D.S., F.A.C.D.
Professor, Oral and Maxillo Facial Surgery
Department of Pediatric Dentistry
College of Dentistry
University of Illinois
Chicago, Illinois
Allan M. Weinstein, Ph.D.
President and Chief Executive Officer IatroMed, Inc.
Phoenix, Arizona
Speakers
Robert E. Baier, Ph.D., P.E.
Director Health-care Instruments and Devices Institute
State University of New York at Buffalo
Buffalo, New York
Burton E. Balkin, D.M.D.
Director Implant Dentistry
University of Pennsylvania
School of Dental Medicine
Narberth, Pennsylvania
Charles L. Bolender, D.D.S., M.S.
Professor and Chairman
Department of Prosthodontics, SM-52
University of Washington
School of Dentistry
Seattle, Washington
Per I. Branemark, M.D.
Professor
Institute for Applied Biotechnology
SWEDEN
John B. Brunski, Ph.D.
Associate Professor
Department of Biomedical Engineering
Rensselaer Polytechnic Institute
Jonsson Engineering Center
Troy, New York
Ulrich M. Gross, M.D.
Professor
Institute of Pathology,
Steglitz Clinic
Free University of Berlin
FEDERAL REPUBLIC OF GERMANY
Jack E. Lemons, Ph.D.
Professor and Chairman
Department of Biomaterials
University of Alabama at Birmingham
School of Dentistry
Birmingham, Alabama
Krishan K. Kapur, D.M.D., M.S.
Professor-in-Residence Removable Prosthodontics
University of California at Los Angeles
Chief Dental Services
Veterans Administration Medical Center
Sepulveda, California
Victor J. Matukas, D.D.S., Ph.D., M.D.
McCallum Professor and Chairman
Department of Oral and Maxillofacial Surgery
University of Alabama at Birmingham
Birmingham, Alabama
Ralph V. McKinney, Jr., D.D.S., Ph.D.
Professor and Chairman
Department of Oral Pathology
Medical College of Georgia
School of Dentistry
Augusta, Georgia
Roland M. Meffert, D.D.S., F.A.C.D., F.I.C.D.
Professor and Chairman
Department of Periodontics
Louisiana State University
School of Dentistry
New Orleans, Louisiana
Anthony H. Melcher, M.D.S., H.D.D., Ph.D., D.Sc.
Professor of Dentistry
Faculty of Dentistry
Associate Dean of Life Sciences
School of Graduate Studies
University of Toronto
Toronto, Ontario CANADA
Lawrence H. Meskin, D.D.S., Ph.D.
Dean of Graduate School
University of Colorado
Health Sciences Center
Denver, Colorado
Joseph R. Natiella, D.D.S.
Professor and Chairman
Department of Stomatology and
Interdisciplinary Sciences
State University of New York at Buffalo
School of Dental Medicine
Buffalo, New York
Michael G. Newman, D.D.S.
Adjunct Professor
University of California at Los Angeles
School of Dentistry
Section of Periodontics
Center for Health Sciences
Los Angeles, California
W. Eugene Roberts, D.D.S., Ph.D.
Professor of Orthodontics
Director
Bone Research Laboratory
University of the Pacific
School of Dentistry
San Francisco, California
Paul A. Schnitman, D.D.S., M.S.
Associate Professor and Head
Department of Implant Dentistry
Harvard School of Dental Medicine
Boston, Massachusetts
Leonard B. Shulman, D.M.D., M.S.
Associate Clinical Professor and Head
Department of Implant Research
Forsyth Dental Center
Boston, Massachusetts
Dennis C. Smith, D.Sc., Ph.D., M.Sc., F.R.S.C.
Professor and Head
Department of Biomaterials
Faculty of Dentistry
University of Toronto
Toronto, Ontario CANADA
Charles M. Weiss, D.D.S., F.I.C.D.
President
Director of Research and Development
Oratronics, Inc.
The Chrysler Building
New York, New York
Philip Worthington, M.D., F.D.S.R.C.S.
Professor of Oral and Maxillofacial Surgery
Department of Oral and Maxillofacial Surgery
University of Washington
Seattle, Washington
Franklin A. Young, Jr., D.Sc., M.S.E.
Professor and Chairman
Department of Materials Science
Medical University of South Carolina
Charleston, South Carolina
George A. Zarb, B.Ch.D., D.D.S., M.S., M.S., F.R.C.D.(c)
Professor and Chairman
Department of Prosthodontics
University of Toronto
Toronto, Ontario CANADA
Planning Committee
D. Walter Cohen, D.D.S.
Conference and Panel Chairperson President
The Medical College of Pennsylvania
Philadelphia, Pennsylvania
Michael J. Bernstein
Director of Communications
Office of Medical Applications of Research
National Institutes of Health
Bethesda, Maryland
Jerry M. Elliott
Program Analyst
Office of Medical Applications of Research
National Institutes of Health
Bethesda, Maryland
Albert D. Guckes, D.D.S., M.S.D.
Chief Commissioned Officer's Dental Clinic
Warren Grant Magnuson Clinical Center
National Institutes of Health
Bethesda, Maryland
H. David Hall, D.M.D., M.D.
Professor and Chairman
Department of Oral Surgery
Vanderbilt University School of Medicine
The Vanderbilt Clinic
Nashville, Tennessee
Jack E. Lemons, Ph.D.
Professor and Chairman
Department of Biomaterials
University of Alabama at Birmingham School of Dentistry
Birmingham, Alabama
Jack L. Lewis, Ph.D.
Professor of Orthopaedic Surgery and Mechanical Engineering
University of Minnesota Medical School
Minneapolis, Minnesota
Marie U. Nylen, D.D.S., Dr. Odont. h.c.
Director Extramural Program
National Institute of Dental Research
National Institutes of Health
Bethesda, Maryland
Anthony Rizzo, D.M.D.
Planning Committee Chairperson
Chief Periodontal and Soft Tissue Diseases Branch
National Institute of Dental Research
National Institutes of Health
Bethesda, Maryland
Patricia Sheridan
Technical Writer/Editor
Office of Planning, Evaluation, and Communication
National Institute of Dental Research
National Institutes of Health
Bethesda, Maryland
D. Gregory Singleton, D.D.S.
Dental Officer Center for Devices and
Radiological Health
Food and Drug Administration
Silver Spring, Maryland
Thomas M. Valega, Ph.D.
Special Assistant for Manpower Development and Training
Extramural Program
National Institute of Dental Research
National Institutes of Health
Bethesda, Maryland
Philip A. Watson, D.D.S., M.S.D.
Professor
Department of Biomaterials
Faculty of Dentistry
University of Toronto
Toronto, Ontario CANADA
Wayne T. Wozniak, Ph.D.
Assistant Secretary
Council on Dental Materials, Instruments, and Equipment
American Dental Association
Chicago, Illinois
Conference Sponsors
National Institute of Dental Research
Harald Loë Director
The Office of Medical Applications of Research
John H. Ferguson Director
The Food and Drug Administration
Frank Young Commissioner
Treatment Planning for Success:
Wise Choices for Maxillary
Single-Tooth Implants
By Belinda L. Gregory-Head, BDS, MS; Alex McDonald PhD, DDS; and Eugene LaBarre DMD,
MS
Abstract: The purpose of this article is to demonstrate to general practitioners
who have no experience with dental implant treatment the esthetic limitations of such
treatment. The criteria for wise case selection will be described so that esthetic
excellence can be predictably achieved in general practice. A checklist of criteria will
be provided as a treatment-planning tool to determine if a patient is likely to have an
esthetically successful outcome.
While the anterior implant patient may come into the office fixed on the notion of
having an implant, further questioning often reveals that his or her chief concern is to
have a missing tooth replaced with something that looks good, feels good, and works like
a real tooth. The challenge of treatment planning is to fulfill these goals. If any of
these criteria cannot be satisfied, then the treatment may be considered a failure.1-3
California dentists may very well face a greater challenge than most in satisfying the
esthetic demands of their patients. Practitioners here must satisfy an extremely
esthetically aware population. Unreasonable demands from patients and unrealistic
promises by practitioners can led to unsatisfactory experiences for all parties. A clear
understanding of the esthetic limitations of dental implants and the practitioner's own
expertise in this area will reduce the risk of unforeseen problems.
Long-term data on the success of implant-supported single-tooth restorations in the
anterior maxilla have been available since 19964 and have been corroborated in
many more recent studies.5-7 Success rates of between 90 percent and 98
percent have been consistently reported. Early papers documented complications as being
mainly mechanical in nature, including screw loosening, component fracture, and loss of
integration. Studies seeking to define success in the anterior region have, until
recently, focused on retention and not on esthetic success.
The push for better function and esthetics has led to a growing appreciation of the
biomechanical limitations of implants. Wider-diameter implants have been introduced.8,9
This addition to the armamentarium along with better engineering of the components and
screw-tightening systems10,11 have brought us to a time when a dental implant
can be a predictable and functional success. Advances in determining the ideal position
of the implant and more accurate surgical techniques have greatly enhanced esthetic
outcomes.12 These have been significant improvements, but they may never be
enough to allow a dental implant to be the treatment of choice for all edentulous spaces
in the anterior region.
v
Functional Success With Esthetic Failure
The purpose of this article is to demonstrate that there are some esthetic limitations
to dental implant treatment. It is aimed at practitioners with no experience with implant
treatment. The criteria for wise case selection will be described so that esthetic
excellence can be predictably achieved in general practice.
The following checklist of nine issues will be discussed. The checklist provides a
treatment-planning tool to determine if a patient is likely to have an esthetically
successful outcome:
- · Assessment of patient expectations;
- · Assessment of gingival display;
- · Gingival thickness;
- · Papilla presence or absence;
- · Morphology of adjacent teeth (crown-to-root ratio);
- · Size and shape of contact areas of adjacent teeth;
- · Available bone height;
- · Available bone width; and
- · Studies appropriate for final decision making.
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants
v
Assessment of Patient Expectations
Patients' desires are often overlooked in guides to treatment planning, yet they may
be the most important criterion assessed by the dentist. An experienced practitioner will
be better able to judge a patient's esthetic demands, but in any case a clear
understanding of the patient's wishes must be established before any treatment
recommendations are made. It is possible to satisfy some demanding patients, but
significant cooperation is required of them. It is critical that the patient be involved
and educated as to the risks, esthetic or otherwise, that may be inherent in the
treatment. The patient will be expected to maintain rigorous dental hygiene and deal with
various provisional restorations as treatment progresses. For this reason, an emphasis on
the team approach is recommended. The patient should become an integral member of the
treatment team along with the laboratory technician, hygienist, and dentists.13,14
Pretreatment intraoral photographs and carefully selected patient-education videos can
help bring the patient's level of understanding up to that required for an esthetic case.15
For a practitioner's first anterior implant case, it is recommended that he or she choose
a cooperative patient with realistic expectations.
v
Assessment of Gingival Display
After initial assessment of patient expectations, the evaluation of the smile line or
gingival display will provide the best indicator as to the esthetic risk of the case.
Excessive gingival display may be due to a number of factors, including vertical
maxillary excess, short clinical crowns, and hypermobility of the upper lip.16
Whatever the underlying etiology, it is important to evaluate the patient's ability to
display gingiva.17,18 Being asked to smile can result in a forced or half
smile and may be misleading. It is recommended that the patient be asked to sneer or lift
his or her upper lip as high as possible so the dentist can assess the situation. If a
"gummy" smile is presented, the patient should be fully informed of the
difficulties ahead. Additional periodontal procedures such as crown lengthening of
remaining maxillary dentition may be considered.19 If the patient is unable to
display gingival tissue, it is still important to discuss the risks, but it is also
possible to reassure the patient that any gingival esthetic compromise will be hidden
from view. The single most important factor for esthetic success in anterior implants is
the smile line. It is highly recommended that the first few patients treated in a
practice have a low lip line.
v
Gingival Form
The morphology of gingival tissue has been discussed extensively in the periodontal
literature. It is relevant to esthetic success with anterior implants since gingival
recession has been identified as a significant complication in these cases.20 The
forms of
periodontium can be broadly divided into two distinct "biotypes," which have
been correlated to specific tooth forms.21 Thin, highly scalloped gingival
tissues are associated with long, narrow, and tapered tooth forms. The second important
biotype is the thick, flat, more fibrous form associated with a shorter, wider, and
squarer tooth shape. The two tissue types are associated with different responses to
inflammatory stimuli. The thin, highly scalloped type tends to respond with marginal
recession and loss of papillary height, while the thick, fibrous type tends to develop a
chronic inflammatory response that may result in periodontal pocketing.22 An
ideal first implant patient would have an abundance of thick, flat, fibrous gingival
tissue and therefore be more resistant to gingival recession around the restoration. This
biotype also allows for the use of metal abutments with less chance of show-through at
the gingival margin. This gingival form is also associated with a favorable square tooth
form.
v
Papilla Presence or Absence
The existence of papillae filling the interdental spaces is a key indicator for future
success. If the remaining dentition exhibits "black triangles" due to lack of
complete fill of the spaces, then the risk of similar incomplete fill around the implant
restoration is high. "Black triangles" may be pre-existing for a number of
reasons, including gingival recession, highly tapered triangular tooth form, and previous
periodontal surgery. The problem is difficult to resolve, and the patient should be
educated as to the esthetic risks involved. Attempts have been made to classify loss of
papillae and provide prognostic indicators.23 Surgical techniques aimed at
regenerating lost papillae have been developed.24,25 Such regeneration remains
challenging, and it may be unwise for a general dentist who is new to implants to
treatment plan a first case anticipating the need for additional periodontal plastic
procedures.
The position of the osseous crest is a critical indicator for potential loss of
papillae after a surgical intervention such as extraction or implant placement.26
The greater the distance from the free gingival margin to the osseous crest, the greater
the esthetic risk. A sounding depth of greater than 3 mm at the midfacial aspect or 4 mm
at the interproximal position would indicate an esthetic risk.27 An ideal
patient would therefore have excellent periodontal health and a high, flat bone profile.
v
Adjacent Tooth Morphology
Complete papillary fill of the interdental space after implant restoration is also
closely related to tooth form, particularly the position and shape of the contact areas.
It has been determined that if the apical limit of the contact area is 5 mm or less
from the osseous crest, then a papilla will be present almost 100 percent of the time in
the
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants
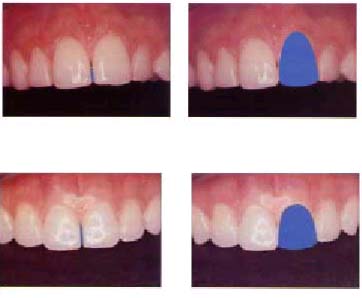
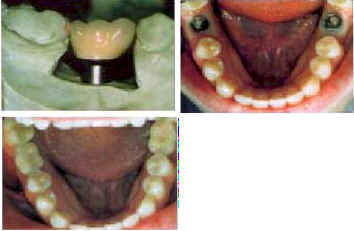
Figure 2. The triangular crown form is associated with thin, highly scalloped gingival
tissues.
Figure 4. The broader, squarer tooth form is associated with thicker, flatter gingival
tissue.
Figure 1. The tapered crown form results in a short, incisally positioned contact area. A
small interdental space is visible in this natural dentition.
Figure 3. Shorter, broader tooth forms have longer contact areas and better prognosis
for fill of the interdental space.

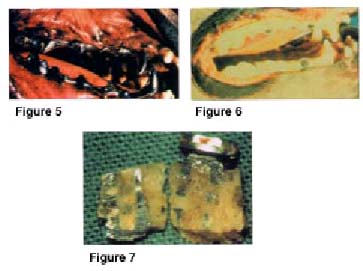
Figure 6. Example of a patient with excellent bone height and favorable tooth form, note
long contact areas.
Figure 5. Ideal vertical placement of implant 3 mm apical to the cement oenamel
junction of adjacent teeth allows for appropriate emergence of crown form (Nobel Biocare
implant with a custom abutment).
natural dentition. An additional 1 mm distance drops the likelihood of a papilla being
present to only 56 percent.28 While the position of the osseous crest may be
difficult to adjust, the position of the contact areas may be changed by the restorative
dentist. A careful evaluation of the patient's natural tooth morphology should be made.
Long, narrow tapered teeth tend to have short incisally positioned contact areas (Figure
1) likely to be further from the osseous crest and therefore likely to have incomplete
fill of the interdental space. The triangular shape (Figure 2) is also associated with
thinner highly scalloped gingival tissue that tends to recede. More predictable anterior
esthetics will be gained with patients who have broader tooth forms and longer, more
cervically positioned contact areas (Figures 3 and 4). Pretreatment photographs are an
essential tool for evaluation of tooth shape and educating the patient as to potential
risks.
Crown shape is related to root form. Ironically, unfavorable clinical crowns with a
triangular morphology taper into a narrow neck and narrow, tapered root form with more
interdental bone. This would be a favorable variable providing for more bone between the
titanium implant and the adjacent natural roots. This makes placement easier and reduces
the risk of root proximity issues. It is generally believed that at least 1.5 mm of
healthy bone should exist between the dental implant and the adjacent root surface.
Recent work on treatment-planning criteria for multiple implant restorations has
suggested that at least 3 mm should separate neighboring implants to reduce interimplant
crestal bone loss and hence preserve vital osseous support for the interimplant papillae.29
Adjacent tooth morphology has an additional effect on treatment planning a single
dental implant. The length of the adjacent clinical crowns will have biomechanical
consequences for the implant restoration regardless of tooth shape. Neighboring long
clinical crowns must be replicated in the final restoration and may result in a long
lever arm acting on the dental implant itself. Unless excellent bone height is available
to facilitate the placement of a long implant, an unfavorable crown-to-implant ratio will
result for most implant systems available.
In relation to adjacent tooth morphology, the ideal implant patient would have short,
wide clinical crowns with long contact areas and existing papillae.
v
Available Bone Height
Occlusal forces act obliquely on anterior teeth. Likewise, an anterior implant
restoration will be loaded nonaxially. Longer implants resist nonaxial loading better and
have been associated with higher success rates. Implants of 11 mm or longer have proven
to be successful in the anterior maxilla.30 If the replacement being proposed
is for a single tooth only, there is often adequate remaining bone height to facilitate
fixture placement.
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants
However, the osseous crest may be positioned apical to ideal. Ideal placement of a
dental implant will result in the top of the fixture being placed 2-4 mm apical to the
cemento-enamel junction of the adjacent teeth (Figure 5). The exact ideal distance will
be modified by the diameter of the chosen implant, the desired emergence profile of the
final crown, and the tissue biotype. If the top of the implant closely replicates the
diameter of the missing tooth, the placement will be more coronal. If the top of the
implant is narrower, then placement will be deeper to facilitate harmonious broadening of
the crown form as it emerges from the tissue. Implant placement in a patient with thin,
highly scalloped tissue would also be deeper to accommodate the tendency to recede and to
reduce the risk of metal show-through.
Available bone height can be evaluated with periapical radiographs and clinical
examination. The ideal patient would have adequate height to house a long implant (13 mm
or more) with the crest of the residual ridge 2 mm below the cementoenamel junction of
the adjacent teeth (Figure 6).
v
Available Bone Width
Successful placement of dental implants depends on adequate osseous housing in all
dimensions. At least 1.5 mm of healthy bone is required between the implant and
neighboring root surfaces and the "standard" implant from most manufacturers
approximates 4 mm in diameter. Therefore the minimum mesiodistal space that can
accommodate an implant between two teeth is 7 mm. Replacement of a central incisor or
cuspid would not usually present a problem in this dimension, but loss of a small lateral
incisor could present risk. In such a case, a narrower implant may be considered or
orthodontic correction carried out.
The implant must also be fully encased in bone in the labiolingual dimension. Again, a
minimum of 7 mm is required for a standard diameter implant. It is this requirement that
presents the most common complication of treatment planning for the anterior maxilla. The
labial plate of cortical bone is often missing and remodeled before implant treatment
planning begins. This may be due to previous periodontal or periapical infection,
traumatic loss, or loss during extraction. Even if an atraumatic extraction technique is
employed, the labial plate will inevitably remodel and become positioned lingually within
three to six months. A distinct labial concavity will be evident when the site is viewed
from the occlusal aspect (Figures 7 and 8).
A significant labial defect that would result in the facial aspect of the implant
being located entirely outside the osseous structures should be considered for hard
tissue augmentation prior to implant placement. A less-significant defect may be
accommodated by slightly deeper and more lingual placement of the fixture to allow for
good osseous contact while maintaining the proper emergence profile (Figure 9).
Dental Implants

Figure 7. Occlusal view of poten-tial implant site showing significant labial
concavity. Hard tissue onlay grafting will idealize the site prior to implant placement.
Figure 8. The same patient as Figure 6. Excellent ridge width in both edentulous
lateral incisor sites.

Figure 9. Graphic illustration of placement lingually and apically from ideal due to loss
of labial cortex. This technique can be used to avoid grafting but should be employed
with caution since significant deviation from ideal position can result in unfavorable
cantilevers and maintenance problems (Illustration by Annette Kramer).
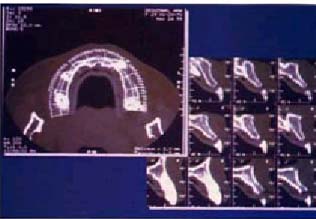
Figure 10. CT scans can significantly increase accuracy in determining available bone for
fixture placement (Image made with GE Lightspeed Plus, Advanced Imaging Center,
Sacramento, Calif.).
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants

Figure 12. Morphology of provisional is accurately duplicated in final restoration.
Figure 11. Ideal placement and provisionalization of implant #5 site results in excellent
emergence profile.
Figure 13. Final restoration in place.
Figure 14. Key anatomic features of an ideal anterior implant patient: low smile line;
abundance of attached keratinized tissue (thick, flat biotype); papillae preserved after
extraction; wide, square-shaped teeth with long contact areas; and excellent bone height
and width (Illustration by Annette Kramer).
v
Determining Available Bone
Assessment of available bone in the mesiodistal and buccolingual dimensions can be
achieved with a thorough clinical examination, or measuring directly from study casts.
Anesthesia and "sounding" of the osseous structures is also a useful technique.
The most accurate diagnostic aid is the CT scan (Figure 10). Unlike Panorex films, where
measurements have to be corrected for varying magnification, the CT film can be measured
directly and is accurate to within 0.1 mm. Dental CT scans have become economic (as low
as $275 to $350 per arch). They should be considered if there is a question as to whether
bone augmentation will be required.
v
Completing the Case
After thorough treatment planning and ideal fixture placement, there is still
opportunity for esthetic excellence or mediocrity in the restoration phase. Several
months of provisionalization allows for maturation of the gingival tissues to an
appropriate (noncylindrical) emergence profile. The tooth form generated through
excellent provisionalization must be carried through to the final restoration so that
crown and papilla form is maintained (Figures 11 through 13).
v
Conclusion
Restoring dental implants in the esthetic zone can be fun if wise choices are made. If
the factors discussed above are carefully considered, patients who present significant
esthetic risks will be screened out and patients with predictably good prognoses will be
taken on. While much emphasis has been placed on the anatomic features of the ideal first
patient (Figure 14) possibly more important is the patient's desire to cooperate with the
team and have realistic expectations. A thorough understanding of the esthetic
limitations of dental implants by all members of the team will result in a rewarding and
satisfying experience.
Authors
Belinda L. Gregory-Head, BDS, MS, is an associate professor and director of dental
implants at the University of the Pacific School of Dentistry.
Alex McDonald, PhD, DDS, is an associate professor and surgical coordinator at the
Implant Clinic at UOP School of Dentistry.
Eugene LaBarre, DMD, MS, is an associate professor and chair of removable
prosthodontics at UOP.
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants
Legends
Figure 1. The tapered crown form results in a short, incisally positioned contact
area. A small interdental space is visible in this natural dentition.
Figure 2. The triangular crown form is associated with thin, highly scalloped gingival
tissues.
Figure 3. Shorter, broader tooth forms have longer contact areas and better prognosis
for fill of the interdental space
Figure 4. The broader, squarer tooth form is associated with thicker, flatter gingival
tissue.
Figure 5. Ideal vertical placement of implant 3 mm apical to the cementoenamel
junction of adjacent teeth allows for appropriate emergence of crown form (Nobel Biocare
implant with a custom abutment).
Figure 6. Example of a patient with excellent bone height and favorable tooth form,
note long contact areas.
Figure 7. Occlusal view of potential implant site showing significant labial
concavity. Hard tissue onlay grafting will idealize the site prior to implant placement.
Figure 8. The same patient as Figure 6. Excellent ridge width in both edentulous
lateral incisor sites.
Figure 9. Graphic illustration of placement lingually and apically from ideal due to
loss of labial cortex. This technique can be used to avoid grafting but should be
employed with caution since significant deviation from ideal position can result in
unfavorable cantilevers and maintenance problems (Illustration by Annette Kramer).
Figure 10. CT scans can significantly increase accuracy in determining available bone
for fixture placement (Image made with GE Lightspeed Plus, Advanced Imaging Center,
Sacramento, Calif.).
Figure 11. Ideal placement and provisionalization of implant #5 site results in
excellent emergence profile.
Figure 12. Morphology of provisional is accurately duplicated in final restoration.
Figure 13. Final restoration in place.
Figure 14. Key anatomic features of an ideal anterior implant patient: low smile line;
abundance of attached keratinized tissue (thick, flat biotype); papillae preserved after
extraction; wide, square-shaped teeth with long contact areas; and excellent bone height
and width (Illustration by Annette Kramer).
References
1. Weisgold AS, Arnoux JP, Lu J, Single-tooth anterior implant: a word of caution.
Part I. J Esthet Dent 9(5):225-33, 1997.
2. Garber D, The esthetic dental implant: letting restoration be the guide. J Am
Dent Assoc 126(3):319-25, 1995.
3. Watson CJ, Tinsley, Sharma S, Implant complications and failures: the single-tooth
restoration. Dent Update 27(1):35-8, 2000.
4. Walther W, Klemke J, et al, Implant-supported single-tooth replacements: risk of
implant and prosthesis failure. J Oral Implantol 22(3-4):236-9, 1996.
5. Henry PJ, Laney WR, et al, Osseointegrated implants for single-tooth replacement: a
prospective 5-year multicenter study. Int J Oral Maxillofac Implants 11(4):450-5,
1996.
6. Naert I, Koutsikakis G, et al, Biologic outcome of single-tooth implant
restorations as tooth replacements: a long-term follow-up study. Clin Implant Dent
Relat Res 2(4):209-18, 2000.
7. Scholander S, A retrospective evaluation of 259 single-tooth replacements by the
use of Brånemark implants. Int J Prosthodont 12(6):483-91, 1999.
8. Boggan RS, Strong JT, et al, Influence of hex geometry and prosthetic table width
on static and fatigue strength of dental implants. J Prosthet Dent 82(4):436-40,
1999.
9. Ivanoff CJ, Sennerby L, et al, Influence of implant diameters on the integration of
screw implants. An experimental study in rabbits. Int J Oral and Maxillofac Surg
26(2):141-8, 1997.
10. Lang LA, May KB, Wang RF, The effect of the use of a counter-torque device on the
abutment-implant interface. J Prosthet Dent 81(4):411-7, 1999.
11. Schulte JK, Coffey J, Comparison of screw retention of nine abutment systems: a
pilot study. Implant Dent 6(1):28-31, 1997.
12. Davarpanah M, Martinez H, Tecucianu JF, Apical-coronal implant position: recent
surgical proposals. Technical note. Int J Oral Maxillofac Implants 15(6):865-72,
2000.
13. Narcisi EM, Culp L, Diagnosis and treatment planning for ceramic restorations. Dent
Clin North Am 45(1):127-42, 2001.
14. Hess D, Buser D, et al, Esthetic single-tooth replacement with implants: a team
approach. Quintessence Int 29(2):77-86, 1998.
15. Dunn JR, Hutson B, Levato CM, Photographic imaging for esthetic restorative
dentistry. Compend Contin Educ Dent 20(8):766-8, 1999.
16. Robbins JW, Differential diagnosis and treatment of excess gingival display. Pract
Periodontics Aesthet Dent 11(2):265-72, 1999.
Treatment Planning for Success: Wise Choices for Maxillary Single-Tooth Implants
17. Morley J, Eubank J, Macroesthetic elements of smile design. J Am Dent Assoc 132(1):39-45,
2001.
18. Paul SJ, Smile analysis and face-bow transfer: enhancing aesthetic restorative
treatment. Pract Proced Aesthet Dent 13(3):217-22, 2001.
19. Levine RA, McGuire M, the diagnosis and treatment of the gummy smile. Compend
Contin Educ Dent 18(8):757-62, 1997.
20. Goodacre CJ, Kan JY, Rungcharassaeng K, Clinical complications of osseointegrated
implants. J Prosthet Dent 81(5):537-52, 1999.
21. Siebert J, Lindhe J, Esthetics and periodontal therapy. In Lindhe J, ed, Textbook
of Clinical Periodontology, 2nd ed. Munksgaard, Copenhagen, 1989, Chap 19.
22. Olsson M, Lindhe J, Periodontal characteristics in individuals with varying forms
of upper central incisors. J Clin Periodontol 18:78-82, 1991.
23. Nordland WP, Tarnow DP, A classification system for loss of papillary height. J
Periodontol 69:1124-26, 1998.
24. Blatz MB, Hurzeler MB, Strub JR, Reconstruction of the lost interproximal
papilla-presentation of surgical and nonsurgical approaches. Int J Periodontics
Restorative Dent 19(4):395-406, 1999.
25. Salama H, Salama M, et al, Developing optimal peri-implant papillae within the
esthetic zone: guided soft tissue augmentation. J Esthet Dent 7(3):125-9, 1995.
26. Kois JC, Predictable single tooth peri-implant esthetics: Five diagnostic keys. Comp
Contin Educ Dent 22(3):199-206, 2001.
27. Kois JC, Altering gingival levels: the restorative connection part 1: biologic
variables. J Esthet Dent 6:3-9, 1994.
28. Tarnow DP, Magner AW, Fletcher P, The effect of the distance from the contact
point to the crest of bone on the presence or absence of the interproximal dental
papilla. J Periodontol 63:995-6, 1992.
29. Tarnow DP, Cho SC, Wallace SS, The effect of inter-implant distance on the height
of inter-implant bone crest. J Periodontol 71:546-9, 2000.
30. Goodacre CJ, Kan JY, Rungcharassaeng K, Clinical complications of osseointegrated
implants. J Prosthet Dent 81(5):537-52, 1999.
Copyright 2001 Journal of the California Dental Association. Vol. 29, No. 11, Nov.
2001
Reprinted with permission.
The Immediate
Dental Implant
By Gordon L. Douglass, DDS, and Robert L. Merin, DDS, MS
Abstract: Numerous clinical studies have shown that dental implants can be placed
immediately in extraction sockets with success when sites are carefully selected. Dental
implants have been placed at the time of extraction with a variety of techniques. All the
techniques report survival rates of 94 percent to 100 percent over a varied healing
period of three months to approximately seven years. This article will review clinical
criteria for determining patient selection for immediate implants and the advantages and
disadvantages of immediate implant placement.
During the past 10 years, numerous clinical studies have shown that dental implants
can be placed immediately in extraction sockets with success when sites are carefully
selected. Dental implants have been placed at the time of extraction with a variety of
techniques including without augmentation, with bone grafting, with bone grafting and a
barrier membrane, and with and without primary closure. The techniques report survival
rates of 94 percent to 100 percent over a varied healing period of three months to
approximately seven years.1-7 Investigators have reported high success rates
with all type of implants, including screw, cylinder, Hydroxylapatite-coated, tapered,
and single-stage.
This article will review the important clinical criteria for determining patient
selection for immediate implants and the advantages and disadvantages of immediate
implant placement. It will also discuss the clinical steps for the placement of dental
implants in extraction sockets. The single-tooth implant restoration has been the most
common immediate implant application, but immediate implants have also been successfully
utilized in full-arch restorations.8 Single-rooted teeth, predominately
incisors and premolars, have been the most frequent sites for immediate implants; but a
study by Schwartz-Arad and colleagues evaluated molar immediate implants and found a
success rate similar to healed molar sites in carefully selected cases.9
v
Patient Evaluation
The first step in determining whether immediate implant placement is a reasonable
clinical choice is evaluation of the potential implant site. Several classification
systems have been proposed by a variety of authors, including Salamma, Gelb, and Becker.10-12
All the systems provide criteria for evaluating the bony morphology for immediate implant
placement. The ideal extraction site for immediate implant placement is one where there
is little or no periodontal bone loss on the tooth that is to be extracted, such as a
tooth with endodontic involvement, root fracture, root resorption, periapical pathology,
root perforation, or unfavorable crown to root ratio (not due to periodontal bone loss).
In all studies, the investigators chose bony three to four walls and sufficient bone to
stabilize the implant. Most researchers report desiring at least 3 to 5 mm of bone beyond
the apex and a bony length of 10 mm or greater for immediate implant placement (Figure
1). There is general consensus that bony defects with two and three walls missing or
severe labial and circumferential defects are not suitable for immediate implant
placement. Wilson showed that the horizontal or circumferential component of the peri-implant
defect was a critical factor relating to the final amount of histologic bone-implant
contact, and that horizontal defects of less than 1.5 mm do not need membranes to obtain
histologic osseointegration13 (Figure 2).
Therefore, immediate implant placement should be limited to those defects that have
three- and four-walled sockets, minimal periodontal bone resorption, sufficient bone to
stabilize the implant, and minimal circumferential defects. Initial implant stability is
the most critical factor in implant osseointegration; therefore, an ideal site is one
with significant alveolar bone around the socket enabling the implant to fill the socket
space (Figure 3). Ivanoff and colleagues have shown that early mobility of implants
greatly reduces their integration and clinical success.14
The Immediate Dental Implant
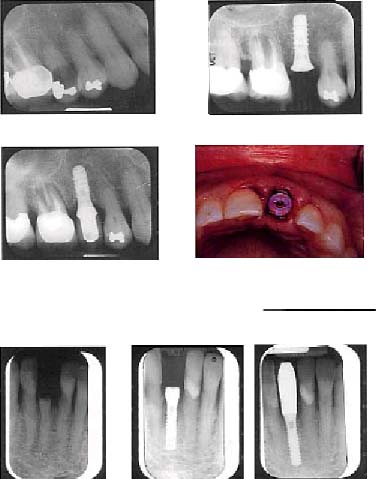
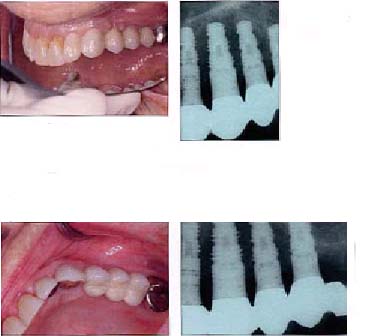
Figure 1a. Preoperative radiograph of tooth #4.
Figure 1b. Immediately after ITI implant placement.
Figure 2. Close adaptation of an implant to the crestal socket wall, within 1.5 mm.
Figure 1c. Two and one-half years after placement. Note that tooth #3 has endodontic
pathology (Implant prosthetics by James M. Herron, DDS, Woodland Hills, Calif.).
Figure 3a. Preoperative view of tooth #25.
Figure 3c. Six months after placement (Implant prosthetics by Gregory W. Holve, DDS,
valley Village, Calif.).
Figure 3b. ITI narrow neck implant immediately after placement.

Figure 4. Microsurgical scalpel (top) and periotome (bottom) can be used to help
extract teeth.
v
Clinical Procedure
Tooth Extraction
The first step in immediate implant placement after case selection is an atraumatic
extraction. Every attempt should be made to minimize trauma to the alveolus during the
extraction. The use of a minisurgical blade to make the initial sulcular incision around
the tooth will facilitate separating the soft tissues from the root and cutting the
periodontal ligament. In many cases, the sulcular incision will be the only incision
needed. The periodontal ligaments can be further separated from the tooth with a
periotome, which will help prevent fracture of the alveolus (Figure 4). Once the tooth
has been loosened with the periotome, if there is adequate tooth structure, the tooth can
be carefully removed with extraction forceps. If there is not adequate tooth structure to
grip with forceps or rongeurs, then the extraction may be attempted with the periotome
alone or by sectioning the root so that the remaining root fragments can be extracted
without placing pressure on the alveolus. The socket is then debrided with curettes or
rotary instruments. The resulting extraction socket is evaluated for osseous defects. If
all four walls are intact and the circumferential defect is less than 1.5 mm, an implant
well may be placed without the need for bone grafting or augmentation. If three or more
walls are present or if the circumferential defect is greater than 1.5 mm, an implant may
be placed; but bone grafting and protection of the socket with a membrane is recommended.
Implant Osteotomy
The next step is the preparation of the extraction area and the apical bone for the
placement of the implant. The first step in the dental implant placement is the beginning
of an osteotomy with a round bur or pilot drill. If the site is a maxillary anterior
tooth, the osteotomy must be kept on the palatal aspect of the alveolus to prevent
perforating the buccal plate. Once the osteotomy is complete to the desired depth with at
least 3 to 5 mm of intimate implant to bone contact, an implant is placed. The implant
must be stable within the osteotomy with no mobility. The implant may touch all of the
bony walls of the extraction site but should not place undue pressure upon thin alveolar
walls (Figure 5). Kohal and colleagues have shown that pressure of the implant on the
bony walls of the alveolus can result in microfractures and early crestal bone loss.15
The ideal situation would be for the implant to be in contact with the socket without
putting undue pressure on the socket walls unless the alveolus is very thick, leaving no
gap between the occlusal part of the implant and surrounding socket walls (Figure 5). In
other words, the postoperative radiographic appearance of an ideal immediate implant
placement would look the same as a standard implant placement (Figure 6).
The Immediate Dental Implant
Figures 5a. Figures 5b.
Figures 5c.
Figure 5g. The implants at uncovering. Figure 5h. The final restorations.
Figure 5d.

Figures 5a through f. Implants are placed in extraction sites and extraction defects.
Note that implants are placed at palatal aspect of the sockets with no pressure on the
buccal place.
Figures 5e.
Figures 5f.

v
The Implant to Socket Wall Space
The space between the implant and socket wall has been an issue of concern and
controversy. Studies have shown that close adaptation of the implant to socket wall
promotes greater osseointegration13,16 (Figure 7). Additionally, in areas
where there is a wide space from the implant to socket wall, better bone healing is
achieved when an occlusive membrane is placed over the socket. In clinical studies,
investigators have utilized a wide variety of techniques -- including the use of a bone
graft to fill the gap and/or the use of an occlusive membrane to prevent epithelial
perforation into the space between the implant and the socket wall_ to aid in the healing
of this space.17-20 Bone healing in an implant osteotomy proceeds apical to
coronal, therefore the coronal aspect becomes the most critical in the healing. An
implant that appears to be clinically stable may have some fibrous tissue attachment at
the coronal margin rather than true osseointegration, and this may not be detectable for
a long time.
Current research favors the use of a barrier if a significant gap exists between the
implant and the socket wall. Numerous occlusive barriers have been used, both resorbable
and nonresorbable, to prevent epithelial migration into the socket area.21,22
In early studies, woven e-PTFE membrane exposure was a significant complication of
membrane placement.23 Newer, more-stable resorbable membranes allow membrane
exposure without complication. Certain barriers _ porcine collagen and freeze-dried
dermas, and laminar freeze dried bone_ can be used in techniques that do not require
primary closure24 (Figure 8).
Historically, most clinical studies have used primary closure of the flaps over
implants placed in extraction sites. Becker and Becker used the inner portion of e-PTFE
membrane as an occlusive barrier over immediate implants in four patients without primary
closure.25 Rosenquist used a synthetic resorbable membrane as an occlusive
barrier in 10 patients and a laminar freeze dried bone membrane as an occlusive barrier
in 25 patients, without primary closure.10 The advantage of not having to
obtain primary closure is the preservation of the gingival tissues (Figure 8f). The
advantage of a resorbable membrane is that it does not have to be removed, and the
collagen membranes and laminar freeze dried bone show excellent tissue compatibility. For
single-stage implants, both resorbable and nonresorbable barriers have been used to cover
the implant-to-socket-wall gap.26-29
Another choice is to use a single-stage implant that extends into the gingival space,
or a healing cap or custom healing component on a two-stage implant, all of which will
now fill the soft tissue portion of the socket completely or partially (Figures 9 and
10). The concern arises when a significant gap exists between the implant and the socket
and the implant structure or healing cap is going to extend through the socket. Research
favors the use of an occlusive barrier or membrane to protect the healing socket area.30
The Immediate Dental Implant
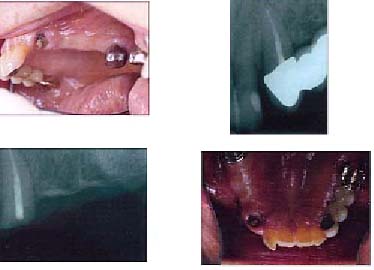
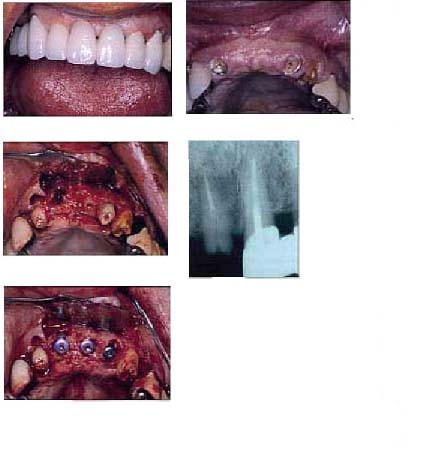
Figure 6a.
Figure 6b.
Figure 6c. Figure 6d.
Figure 6e. Figure 6f. Figure 6g.
Figures 6a through d. No. 11 is fractured, and #10 has irreversible mobility due to
traumatic injury, which prohibits the replacement of the fixed bridge #11-15.

Figures 6e through g. Implants are placed in the extraction sites of #10 and #11 and in
the #12 and #13 healed sites.
Dental Implants
Figures 6i.
Figures 6h through k. The final implant restoration showing excellent preservation of the
gingival form and no difference on the radiographs between the implants in the immediate
and healed sites.
Figures 6j. Figures 6k.


Figure 7a. Preoperative radiograph.
Figure 7b. Immediately after placement of ITI 4.8 mm implant.
Figure 7c. Ten months postoperative radiograph (Implant prosthetics by David M.
Campbell, DDS, Woodland Hills, Calif.).
The Immediate Dental Implant
v
Postoperative Management
A temporary prosthesis, either removable or fixed, can be placed over the implants.
However, a removable prosthesis should not put pressure on the implant or it will result
in premature loading of the implant. Premature loading or vibration of dental implants
has been shown to delay osseointegration and retard bone healing.
Recently, there have been studies evaluating immediate loading of immediate placed
dental implants.31 This has primarily been done where there are four or more
implants extending around a curve that are rigidly splinted together.32 The
authors believe that it is premature to consider loading single implants at this time
since there are significant variables that may retard implant healing. The placement of a
temporary crown, even one that is out of function, transmits load to the implant. New
implant surfaces have been approved by the Food and Drug Administration for loading as
early as eight weeks so that the time from implant placement to the placement of a
temporary crown has shortened significantly, but the greater size of the bone-to-implant
gap around some immediate implants may require longer healing times. The early placement
of a temporary crown on an implant and the experimentation with immediate loading should
not be considered by those who do not have extensive experience in implant placement and
prosthetics.
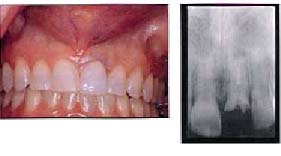
Figure 8b.
Figures 8a and b. Preoperative photo and radiograph showing #9 with a vertical
fracture.

Figure 8c. A wide-diameter root form implant is placed, which reduces the distance
between the socket walls and the implant.
v
Soft Tissue Management
One of the most critical factors in implant restorative esthetics is the gingival
form. The gingival tissues can be shaped and managed by the temporary prosthesis and by
the provisional crown that is placed on the implant prior to placement of the final crown
(Figure 11). In areas where single-stage implants or a healing cap can be used, the
implant itself may help to support the gingival tissues and the interdental papillae,
which are critical for implant esthetics (Figure 10). In the restoration of dental
implants in the esthetic zone of the maxillary anterior teeth, it is recommended that a
temporary crown be considered as part of the restorative treatment plan to help shape and
form the peri-implant tissues prior to placement of the final crown (Figure 8g).
If it is possible to place the dental implant with minimal disruption of the peri-implant
tissues and provide immediate support, the management of the tissues will be facilitated.
The use of anatomic gingival formers or single-stage implants and the placement of
implants without elevating a flap have significantly improved practitioners' ability to
readily achieve excellent peri-implant gingival form.


Figure 8e.
Figures 8d and e. Two resorbable collagen membranes are placed, one on the buccal because
of a narrow buccal late defect and one covering the implant, eliminating the need for
primary closure.


Figure 8g. Temporary restoration helping shape the gingival form.
Figure 8f. Healing at five weeks with preservation of gingival papillae.
The Immediate Dental Implant


Figure 8h. and i. The final restoration one year after completion.
Figure 8i.

Figure 9a. Preoperative view of tooth #21.
Figure 9b. ITI implant immediately after placement.
Figure 9c. Four months after placement. Note bone healing around neck of the implant.


Figure 10b.
Figure 10a and b. No. 7 fractured and nonrestorable.


Figure 10d.
Figure 10c and d. No. 7 fractured an immediate implant is placed.
Dental Implants


Figure 10f.
Figures 10e and f. Final restoration exhibiting the same gingival form as the original
tooth.

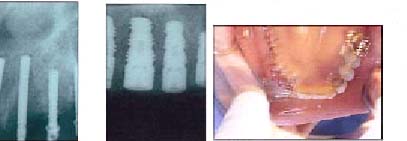
Figure 11a. Preoperative #8 with a fractured root.
Figure 11b. Implant placement #8.


Figure 11d. Radiograph of implant #8.
Figure 11c. Surgical site sutured with minimal displacement of the interdental papillae.


Figures 11e and f. Temporary removable appliance used to shape and support the
gingival papillae.
The Immediate Dental Implant


Figure 11h. Final crown with maintenance of interdental gingival form.
Figure 11g. Healing cap placed.


Figure 12a. Radiograph of #8 shows a large radiolucency associated with a root
fracture that precludes immediate implant placement.
Figure 12b through d. Extraction and augmentation of the socket.


Figure 12c. Figure 12d.


Figures 12e and f. Healing and tissue support from the removable appliance.
Figure 12f.
Dental Implants


Figures 12h.
Figures 12g through i. Implant placement eight months later.


Figures 12i.
Figure 12j. Implant site and uncovering.

Figures 12k and l. Implant restored with temporary crown 12 months from extraction. The
two-stage approach takes considerably more time and more steps than immediate placement.

Figures 12l.
The Immediate Dental Implant
v
Advantages and Disadvantages
The primary advantages of immediate implant placement are the reduction in time of
therapy, the reduction in surgical episodes, and preservation of the bone and gingival
tissues. The greatest rate of bone resorption occurs during the first six months
following tooth extraction unless an implant is placed or a socket augmentation procedure
performed.30 The early maintenance of gingival form will greatly facilitate
the peri-implant gingival tissue esthetics by maintaining support for the interdental
papillae (Figure 11).
The primary disadvantage of immediate implant placement is the fact that the clinician
may not be able to place the implant at the time of extraction even though time has been
scheduled. The patient must always be informed that although an immediate placement will
be attempted, it is not guaranteed since there is always a possibility that factors such
as ankylosis, bone fractures of facial plates, socket expansion during extraction, or
extensive infection might make immediate placement impossible. These areas will require
extraction socket healing and possible augmentation before an implant can be placed
(Figures 12 and 13).


Figure 13a. Preoperative radiograph. Tooth #6 was not a good candidate for an
immediate implant because the root fracture had caused too much vertical and horizontal
bone loss on the facial bone.
Figure 13b. Preoperative photograph.

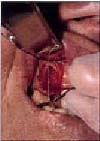
Figure 13c. Surgical view of missing facial bone.
Figure 13d. Photograph of extracted tooth.
v
Conclusion
Dental implants that are immediately placed into carefully selected extraction sockets
have high survival rates comparable to implants placed in healed sites. The
immediate-placement implants provide significant advantages of less surgical procedures,
shorter treatment time, and the facilitation of improved esthetics. There are significant
areas of information that need to be clarified regarding the use of bone grafts and
membranes around immediately placed implants and the size of the space between the
implant and socket wall. Until these are clarified with evidence-based clinical studies,
clinical judgment behooves dentists to use prudence in their case selection for immediate
implants. There must be adequate bone to give implant stability, and the bony walls
around implants should be intact on at least three of the four sides. However, with these
caveats, the immediate implant has now become a significant part of implant therapy and
provides for timely esthetic implant restorations.
Authors
Gordon L. Douglass, DDS, maintains a private practice in Sacramento, Calif. Robert L.
Merin, DDS, MS, is the immediate past president of the California Society of
Periodontists. He is also a lecturer at the University of California at Los Angeles
School of Dentistry and a consultant for the West Los Angeles Veterans Administration. He
maintains a private practice in Woodland Hills, Calif. Dr. Merin is a diplomate of the
American Board of Periodontology and a staff member of West Hills Hospital and Northridge
Hospital.
The Immediate Dental Implant
References
1. Lazzara RJ, Immediate implant placement into extraction sites: Surgical and
restorative advantages. Int J Periodont Restorative Dent 9:333-43, 1989.
2. Ashman A, An immediate tooth root replacement: An implant cylinder and synthetic
bone combination. J Oral Implantol 16:28-38, 1990.
3. Parel SM, Triplett RG, Immediate fixture placement: A treatment planning
alternative. Int J Oral Maxillofac Implants 5:337-45, 1990.
4. Barizilay I, Grasser GN, et al, Immediate implantation of a pure titanium implant
into an extraction socket: Report of a pilot procedure. Int J Oral Maxillofac Implants
6:277-84, 1991.
5. Tolman DE, Keller EE, Endosseous implant placement immediately following dental
extraction and alveoplasty: Preliminary report with 6 year follow-up. Int J Oral
Maxillofac Implants 6:24-8, 1991.
6. Becker W, Becker BE, et al, Guided tissue regeneration for implants placed into
extraction sockets: A study in dogs. J Periodontal 62:703-9, 1991.
7. Yukna RA, Clinical comparison of hydroxylapatite-coated titanium dental implants
placed in fresh extraction sockets and healed extraction sites. J Periodontol
62:468-72, 1991.
8. Schwartz-Arad D, Chaushu G, Full-arch restoration of the jaw with fixed ceramometal
prosthesis. Int J Oral Maxillofac Implants 13:819-25, 1998.
9. Schwartz-Arad D, Gorssman Y, Chaushu G, The clinical effectiveness of implants
placed immediately into fresh extraction sites of molar teeth. J Periodontal
71:839-44, 2000.
10. Salama H, Salama M, The role of orthodontic extrusive remodeling in the
enhancement of soft and hard tissue profiles prior to implant placement: A systematic
approach to the management of extraction site defects. Int J Periodont Restorative
Dent 13:313-33, 1993.
11. Gelb DA, Immediate implants surgery: Three-year retrospective evaluation of 50
consecutive cases. Int J Oral Maxillofac Implants 8:388-99, 1993.
12. Becker W, Dahlin C, et al, The use of ePTFE barrier membranes for bone promotion
around titanium implants placed into extraction sockets: A prospective multicenter study.
Int J Oral Maxillofac Implants 9:31-40, 1994.
13. Wilson TG, Schenk R, et al, Implants placed in immediate extraction sites: A
report of histologic and histometric analyses of human biopsies. Int J Oral Maxillofac
Implants 13:333-41, 1998.
14. Ivanoff C-J, Sennerby L, Lekholm U, Influence of initial implant integration of
titanium implants. An experimental study in rabbits. Clin Oral Impl Res 7:120-7,
1996.
15. Kohal RJ, Hurzeler MB, et al, Custom-made root analogue titanium implants placed
into extraction sockets. An experimental study in monkeys. Clin Oral Impl Res
8:386-92, 1997.
16. Lundgren D, Rylander H, et al, Healing-in of root analogue titanium implants
placed in extraction sockets: An experimental study in the beagle dogs. Clin Oral
Implants Res 3:136-44, 1992.
17. Todescan R, Pilliar RM, Melcher AH, A small animal model for investigating
endosseous dental implants: Effect of graft materials on healing endosseous,
porous-surfaced implants placed in a fresh extraction socket. Int J Oral Maxillofac
Implants 2:217-23, 1987.
18. Becker W, Lynch SE, et al, A comparison of ePTFE membranes alone or in combination
with platelet-derived growth factors and insulin-like growth factor-1 or demineralized
freeze-dried bone in promoting bone formation around immediate extraction socket
implants. J Periodontal 63:929-40, 1992..
19. Wilson TG, Guided tissue regeneration around dental implants in immediate and
recent extraction sites: Initial observations. Int J Periodont Restorative Dent
12:184-93, 1992.
20. Lang NP, Bragger U, et al, Immediate transmucosal implants using the principle of
guided tissue regeneration (I). Rationale, clinical procedures and 30 month results. Clin
Oral Implants Res 5:154-63, 1994.
21. Gher ME, Quintero G, et al, Bone grafting and guided bone regeneration for
immediate implants in humans. J Periodontal 65:881-91, 1994.
22. Sevor JJ, Meffert RM, Placement of implants into fresh extraction sites using a
resorbable collagen membrane. Case reports. Practical Periodontology and Aesthetic
Dentistry 4:35-41.
23. Celletti R, Davarpanah M, et al, Guided tissue regeneration around dental implants
in immediate extraction sockets: Comparison of e-PTFE and a new titanium membrane. Int
J Periodont Restorative Dent 14:243-53, 1994.
24. Becker W, Becker B, et al, Autogenous bone grafting of bone defects adjacent to
implants placed into immediate extraction sockets in patients: A prospective study.
Internat J Oral Maxillofac Implants 389-96, 1994.
25. Rosenquist B, A bioresorbable GTR membrane as occlusive barrier after placement of
implants into fresh extraction sockets. A preliminary study. Submitted for publication,
1999.
26. Rosenquist B, Ahmed M, The immediate replacement of teeth by dental implants using
homologous bone membranes to seal the sockets: Clinical and radiographic findings. Clin
Oral Impl Res 11:572-82, 2000.
27. Cochran DL, Douglas HB, Augmentation of osseous tissue around nonsubmerged
endosseous dental implants. Int J Periodontics Restorative Dent 13:506-19, 1993.
The Immediate Dental Implant
28. Bragger U, Hammerle CHF, Lang NP, Immediate transmucosal implants using the
principle of guided tissue regeneration (II). A cross-sectional study comparing the
clinical outcome 1 year after immediate and standard implant placement. Clin Oral
Implants Res 7:268-76, 1996.
29. Cornelini R, Immediate Transmucosal Implant Placement: A Report of 2 Cases. Int
J Periodontics Restorative Dent 20:199-206, 2000.
30. Schwartz-Arad D, Chaushu G, The Ways and Wherefores of Immediate Placement of
Implants Into Fresh Extraction Sites: A Literature Review. J. Periodontol 10:915-23,
1997.
31. Chaushu G, Chaushu S, et al, Immediate loading of single-tooth implants: immediate
versus non immediate implantation. A clinical report. Int J Oral Maxillofac Implants 16(2):267-72,
2001.
32. Jaffin RA, Kumar A, Berman C, Immediate loading of implants in partially and fully
edentulous jaws: A series of 27 case reports. J Periodontol 71:833-8, 2000.
Legends
1. Figure 1a. Preoperative radiograph of tooth #4.
2. Figure 1b. Immediately after ITI implant placement.
3. Figure 1c. Two and one-half years after placement. Note that tooth #3 has
endodontic pathology (Implant prosthetics by James M. Herron, DDS, Woodland Hills,
Calif.).
4. Figure 2. Close adaptation of an implant to the crestal socket wall, within 1.5 mm.
5. Figure 3a. Preoperative view of tooth #25.
6. Figure 3b. ITI narrow neck implant immediately after placement.
7. Figure 3c. Six months after placement (Implant prosthetics by Gregory W. Holve,
DDS, valley Village, Calif.).
8. Figure 4. Microsurgical scalpel (top) and periotome (bottom) can be used to help
extract teeth.
9. Figures 5a through e. Implants are placed in extraction sites and extraction
defects. Note that implants are placed at palatal aspect of the sockets with no pressure
on the buccal place.
10. Figure 5g. The implants at uncovering.
11. Figure 5h. The final restorations.
12. Figures 6a through d. No. 11 is fractured, and #10 has irreversible mobility due
to traumatic injury, which prohibits the replacement of the fixed bridge #11-15.
13. Figures 6e through g. Implants are placed in the extraction sites of #10 and #11
and in the #12 and #13 healed sites.
14. Figures 6h through k. The final implant restoration showing excellent preservation
of the gingival form and no difference on the radiographs between the implants in the
immediate and healed sites.
15. Figure 7a. Preoperative radiograph.
16. Figure 7b. Immediately after placement of ITI 4.8 mm implant.
17. Figure 7c. Ten months postoperative radiograph (Implant prosthetics by David M.
Campbell, DDS, Woodland Hills, Calif.).
18. Figures 8a and b. Preoperative photo and radiograph showing #9 with a vertical
fracture.
The Immediate Dental Implant
19. Figure 8c. A wide-diameter root form implant is placed, which reduces the distance
between the socket walls and the implant.
20. Figures 8d and e. Two resorbable collagen membranes are placed, one on the buccal
because of a narrow buccal late defect and one covering the implant, eliminating the need
for primary closure.
21. Figure 8f. Healing at five weeks with preservation of gingival papillae.
22. Figure 8g. Temporary restoration helping shape the gingival form.
23. Figures 8h through j. The final restoration one year after completion.
24. Figure 9a. Preoperative view of tooth #21.
25. Figure 9b. ITI implant immediately after placement.
26. Figure 9c. Four months after placement. Note bone healing around neck of the
implant.
27. Figure 10a and b. No. 7 fractured and nonrestorable.
28. Figures 10c and d. No. 7 an immediate implant is placed.
29. Figures 10e and f. Final restoration exhibiting the same gingival form as the
original tooth.
30. Figure 11a. Preoperative #8 with a fractured root.
31. Figure 11b. Implant placement #8.
32. Figure 11c. Surgical site sutured with minimal displacement of the interdental
papillae.
33. Figure 11d. Radiograph of implant #8.
34. Figures 11e and f. Temporary removable appliance used to shape and support the
gingival papillae.
35. Figure 11g. Healing cap placed.
36. Figure 11h. Final crown with maintenance of interdental gingival form.
37. Figure 12a. Radiograph #8 shows a large radiolucency associated with a root
fracture that precludes immediate implant placement.
38. Figure 12b through d. Extraction and augmentation of the socket.
39. Figures 12e and f. Healing and tissue support from the removable appliance.
40. Figures 12g through i. Implant placement eight months later.
41. Figure 12j. Implant site and uncovering.
42. Figures 12k and l. Implant restored with temporary crown 12 months from
extraction. The two-stage approach takes considerably more time and more steps than
immediate placement.
43. Figure 13a. Preoperative radiograph. Tooth #6 was not a good candidate for an
immediate implant because the root fracture had caused too much vertical and horizontal
bone loss on the facial bone.
44. Figure 13b. Preoperative photograph.
45. Figure 13c. Surgical view of missing facial bone.
46. Figure 13d. Photograph of extracted tooth.
Copyright Journal of the California Dental Association. Vol. 30, No. 5, May 2002.
Reprinted with permission.
Implant-Borne
Single Tooth Replacement_
An Illustration and Rationale
By Richard K. Rounsavelle, DDS
Abstract: This article demonstrates a method for the replacement of a single
missing tooth with a dental implant system that can simply and easily be incorporated
into a general practice. Recent innovations in implant abutment design and impression
procedures have resulted in a technique that is very similar to traditional crown and
bridge procedures. This article describes a step-by-step protocol for the restoration of
a single missing tooth with an implant-borne, cemented crown.
The replacement of diseased natural tooth substance with an optimal material is the
essence of restorative dentistry. The restoration should be durable, be reasonably
esthetic, and require minimally invasive procedures. Dental schools have taught the art
and science of partial coverage cast gold restorations (Figures 1a and b) with the
ultimate intent of conserving healthy tooth structure. The implant-borne single tooth
replacement, like the partial gold casting, embodies the principle of tooth conservation
which all dentists should espouse in serving their patients.
With an implant, the adjacent teeth, when healthy, need no longer be prepared solely
for the purpose of providing support for a fixed bridge. On occasion, every dentist has
seen a formerly healthy tooth progress through a series of destructive events following
restoration for crown retainers. This scenario is now avoidable.
The ITI Solid Abutment System, described herein, heralded a breakthrough in
simplifying the restorative process. Dental implants, formerly the province of a few
specialists, now may be routinely accomplished by all general dentists.
v
Treatment Planning
A team approach is best for treating implant patients. The general practitioner should
refer his or her patients to a qualified specialist for surgical placement of implant
fixtures, along with bone grafting and soft-tissue manipulation where indicated. In
consultation with a surgeon, the G.P. will share the responsibility for evaluating such
factors as medical history, availability of supporting bone, soft tissue contours,
occlusion, and cosmetics. The use of mounted study casts with a diagnostic wax-up of the
replacement tooth greatly facilitates the shared evaluation of a given case. In addition
to the wax-up, the G.P. may also provide guidance as to implant location by using a
surgical stent or template for surgical implant positioning. This appliance may take many
forms, but for single tooth replacement, a tooth-borne device is usually most
appropriate. This device may transfer from the diagnostic wax-up the facial or lingual
anatomy of the proposed final restoration, depending on the surgeon's preference. This
transfer conveys to the surgeon the G.P.'s intent for the final restoration at the time
of implant placement (Figure 2).
v
Standard Abutment-Final Impressions
After the implant has "osseointegrated," or united to the surrounding bone,
the patient is ready for restoration. The technique described involves a solid abutment,
which is analogous to a tooth preparation (Figure 3); an impression cap and cylinder; and
a laboratory replica of the abutment.
First, one places the white impression cap over the implant collar (Figure 4). This
impression coping eliminates the need for tissue retraction and, therefore, local
anesthesia. To be certain that complete seating has occurred, one should rotate the cap
while viewing it from an occlusal direction. If the cap rotates without dislodging and
the abutment appears to be centered, it is seated properly. Seating requires firm
pressure and, when achieved, will result in a palpable "click" (Figure 5).
Next, the positioning cylinder (Figure 6) is placed into the impression cap. The trick
here is to view the abutment again from an occlusal perspective to orient the flat
section of the abutment and match it to the corresponding flat area of the positioning
cylinder. It, too, will seat with firm pressure and must go completely into place (Figure
7).
One is then ready to take the impression. The best impression material to use is the
most rigid: vinyl polysiloxane. Polyether and polysulfide also work well. Nonrigid
materials, such as hydrocolloid, are contraindicated. One should be sure to block out any
large undercuts created by teeth within the arch. Syringe hydrocolloid works well for
blocking.
Implant-Borne Single Tooth Replacement_An Illustration and Rationale
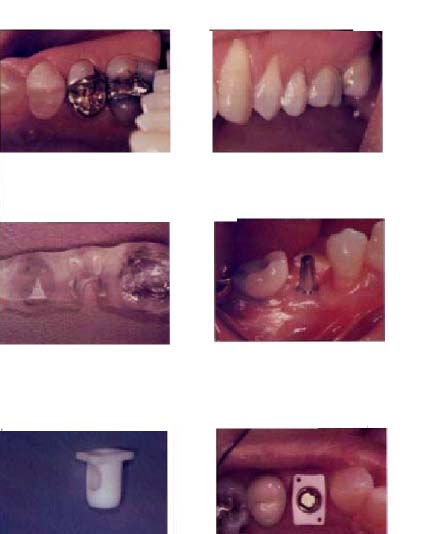
Figure 1a. Figure 1b.
Figures 1a and b. Partial gold coverage can be both conservative and esthetic.
Figure 2. Implant positioning guide for single tooth with lingual acrylic of replacement
tooth removed.
Figure 3. Standard solid abutment
torqued into ITI implant fixture.
Figure 4. Standard abutment
impression cap.
Figure 5. Impression cap in place over abutment.
Dental Implants
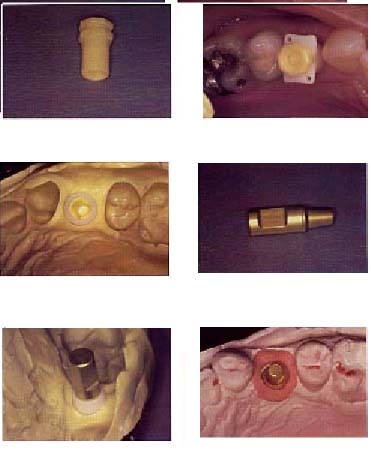
Figure 6. Positioning cylinder for 5.5 mm solid abutment.
Figure 7. Positioning cylinder seated into impression cap.
Figure 8. Impression cap/positioning cylinder imbedded within final impression.
Figure 9. Analog of a 5.5 mm solid abutment.
Figure 10. Analog seated into place in the impression cap/positioning cylinder
assembly.
Figure 11. Final laboratory cast for crown fabrication.
Implant-Borne Single Tooth Replacement_An Illustration and Rationale

Figure 12. Plastic coping for laboratory procedures (seated on analog).
Figure 13. Protective cap for temporization.
Figure 14. Plastic coping shortened and air abraded for inclusion in an acrylic
provisional crown.
Figure 15. Modified copings seated on solid abutment.
Figure 16a. Acrylic filled shell seated over modified copings.
Figure 16b. Shell with acrylic and copings incorporated.
One should inject and place the tray as for any other crown impression. The cap and
cylinder assembly should lift off the abutment and be embedded within the impression
(Figure 8).
The actual "prep" or abutment that the lab will use is called an analog or
abutment replica (Figure 9). This is a small metal component that one must next mate to
the impression component assembly. Again, one carefully matches the flat side of the
analog with the flat side of the positioning cylinder and firmly pushes it into place. If
the analog does not snap into the impression cap, it is not seated completely (Figures 10
and 11).
The impression is now ready for the lab. The lab will use a prefabricated plastic
coping (Figure 12) to act as a base onto which wax is added to create the appropriate
contour from which the crown is completed via conventional procedures.
v
Temporary Crowns
The options for placing a temporary crown depend upon the patient and the situation. A
very simple approach is to use temporary cement to place a temporary protective cap
available from the manufacturer (Figure 13). If the patient requires a more esthetic
temporary crown, one may modify a plastic coping (the same one used in the laboratory
phase) and incorporate the coping with acrylic resin into a crown form or clear plastic
shell. This latter technique requires more chair time but is greatly appreciated by a
patient who needs a tooth and has been without a fixed replacement. The procedure for
this is as follows:
First, one shortens, scores, and air abrades the coping in the lab. Then one seats the
coping until it snaps into place over the abutment (Figure 15). The crown form or clear
matrix filled with acrylic is allowed to set completely on the coping (Figures 16a and
b). It is very important to remove all acrylic from any undercuts prior to the final set.
The coping "over-crown" is then taken to the lab; and, very carefully, using
the salt and pepper technique, one fills in the spaces between the acrylic and the margin
of the coping (Figure 17). Once this is achieved, one may finish and polish to create the
final crown contour and emergence profile. The final provisional must snap into place on
the abutment to prevent soft tissue encroachment over the implant collar. To achieve this
fit, one must remove a small amount of acrylic from the occlusal aspect of the
provisional internally with a straight fissure lab bur. One then cements with temporary
cement and thoroughly removes any gingival excess, as it commonly lodges just below the
implant collar.
Implant-Borne Single Tooth Replacement_An Illustration and Rationale
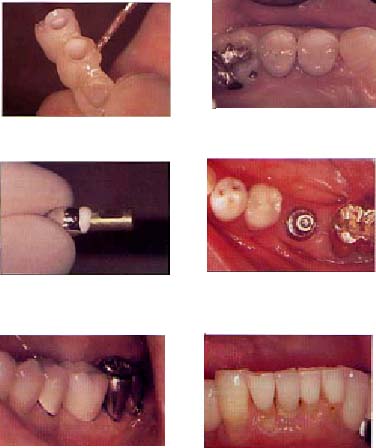
Figure 17. Addition of acrylic to establish contour and marginal adaptation.
Figure 18. Final first premolar restoration cemented to place.
Figure 20. ITI Wide Neck abutment.
Figure 19. Partial displacement of excess cement using laboratory analog prior to
cementation.
Figure 21. Final restoration showing a more favorable emergence contour achievable
with wider implant (tooth #31 was periodontally compromised).
Figure 22.

Figures 22, 23. Very narrow restorations on the ITI Narrow Neck abutments.
v
Delivery of Final Restoration
The beauty of this implant system is its simplicity and similarity to conventional
crown and bridge procedures: One tries the crown in place, adjusts contacts and
occlusion, and cements. The following are helpful hints on adjusting these crowns:
- n One should be very careful in adjusting contacts because there is no periodontal
ligament "cushion" on the implant to absorb small discrepancies. If the
contact is excessive, the crown will not seat completely.
- n One should relieve all eccentric occlusal contacts _especially those that occupy
the extreme periphery of the occlusal table.
- n One should make certain that the centric contacts are as close to the long axis
of the implant fixture as possible and are light. One should have the patient firmly
clench to register contact with a mylar shim stock.
- n If temporary cement is to be used, one should be aware that implant-borne crowns
tend to dislodge very abruptly and unpredictably when luted with temporary cement
(Figure 18).
- n It is always a good practice to place an impression cap onto the abutment
whenever one is working with the final crown away from the chair. This procedure will
prevent the soft tissues from collapsing over the implant collar and from blocking
complete seating of the final crown.
If the implant collar extends more than 2 mm subgingivally, one may minimize excess
cement by displacing it with an analog prior to final cementing of the crown (Figure 19).
When a large volume of cement is removed extraorally, the clean-up of set cement from the
subgingival area is greatly facilitated.
Implant-Borne Single Tooth Replacement_An Illustration and Rationale
v
Other Abutments
There are several abutments available to deal with other restorative situations and
locations. For example, when the missing tooth has sufficient bone and mesiodistal
dimensions, as in the molar region, a larger diameter implant with a wider platform is
indicated (Figure 20). This increased diameter affords significantly greater implant
surface area for osseointegration and a more-ideal emergence profile for the final
restoration (Figure 21). A larger bearing area better distributes the load of posterior
occlusion. The components and procedures are identical to those used with the standard
abutment. Due to the posterior location of most wide-body implants, one would usually
temporize with a simple protection cap. Cementation considerations are similar to the
standard abutment; however, because these abutments are often shorter than the standard
due to reduced interocclusal distance, the additional retention afforded by stronger
cement may be needed. Retention may also be enhanced by a lateral set screw.
A narrow implant and abutment can be used for mandibular incisors, maxillary lateral
incisors, and some small premolar areas (Figures 22, 23).
v
Custom Abutments
There will be situations in which the implant collar (the finish line of the
restoration) is intentionally located deeply subgingivally to help the restorative
dentist develop the optimum esthetics of the final restoration. This usually occurs in
the anterior region and the mesial aspect of the maxillary first premolar. If the final
crown margin extends to this deep margin location, a significant complication may occur
during cementation. Excess cement can be driven over, around, and under the implant
collar during crown placement. This subgingival cement can be very difficult, if not
impossible, to remove completely; and these retained cement fragments may cause
considerable soft tissue inflammation and infection.
The best way to avoid "deep" finish lines affecting implant-borne anterior
crowns is to use the custom abutment (Figure 24). The clinician may then elevate the
margin to a more coronal location. With the finish line, and thus the excess cement, made
more accessible, the complication of excess cement removal is greatly reduced. There are
other advantages of using the custom abutment in the anterior teeth. The long axis of the
implant may be in a different inclination than that of the final crown. The custom
abutment can correct this discrepancy in both labiolingual and mesiodistal directions.
The resulting contour enhances tissue health and architecture for an optimum esthetic
result (Figure 25).
Dental Implants
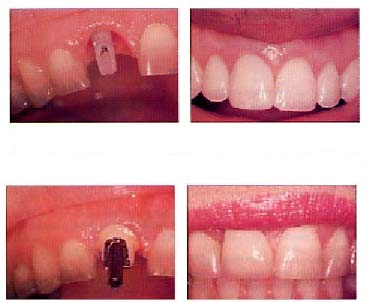
Figure 24. Soft tissue that has been
sculpted by a properly contoured provisional crown.
Figure 25. Provisional restoration veneered with microfill composite resin.
Figure 26. Ceramo-metal custom abutment on tooth #8.
Figure 27. Final ceramo-metal crown cemented on the custom abutment shown in Figure
24.
To maximize the esthetic result, one should sculpt the surrounding tissues with a
carefully made provisional crown prior to the final impressions (Figure 26). The
technique that uses a plastic coping and stock crown or prefabricated clear shell works
well. For the cosmetically demanding patient, one may modify the shade of the provisional
crown by removing approximately 1 mm of labial acrylic and directly bonding microfill
composite resin to the acrylic surface (Figure 27).
One may fabricate the custom abutment by casting metal to a stock screw-retained
abutment. This custom abutment is secured to the implant with the appropriate screw, and
the crown is cemented onto it.
Implant-Borne Single Tooth Replacement_An Illustration and Rationale
v
Conclusion
This article has described a technique that will greatly facilitate the incorporation
of osseointegrated dental implant restorative treatment into the general practitioner's
routine procedures. This technique is just a beginning. The principle and procedures
discussed can be expanded to apply to a wide variety of more-involved restorative
situations that may be more complicated. As one's experience and skill increases, the way
one thinks about cases with missing teeth will change considerably. The care one provides
to patients will progress to a higher level, a level that fully respects the ideals of
mentors who encouraged their students to preserve tooth structure with conservative gold
restorations.
Author
Richard K. Rounsavelle, DDS, is a general dentist in Torrance, Calif. He is also a
member of CDA's Council on Scientific Sessions.
Copyright California Dental Association Journal. Vol. 29, No. 11, Nov. 2001.
Reprinted with permission.
Legends
1. Figures 1a and b. Partial gold coverage can be both conservative and esthetic.
2. Figure 2. Implant positioning guide for single tooth with lingual acrylic of
replacement tooth removed.
3. Figure 3. Standard solid abutment torqued into ITI implant fixture.
4. Figure 4. Standard abutment impression cap.
5. Figure 5. Impression cap in place over abutment.
6. Figure 6. Positioning cylinder for 5.5 mm solid abutment.
7. Figure 7. Positioning cylinder seated into impression cap.
8. Figure 8. Impression cap/positioning cylinder imbedded within final impression.
9. Figure 9. Analog of a 5.5 mm solid abutment.
10. Figure 10. Analog seated into place in the impression cap/positioning cylinder
assembly.
11. Figure 11. Final laboratory cast for crown fabrication.
12. Figure 12. Plastic coping for laboratory procedures (seated on analog).
13. Figure 13. Protective cap for temporization.
14. Figure 14. Plastic coping shortened and air abraded for inclusion in an acrylic
provisional crown.
15. Figure 15. Modified copings seated on solid abutment.
16. Figure 16a. Acrylic filled shell seated over modified copings.
17. Figure 16b. Shell with acrylic and copings incorporated.
18. Figure 17. Addition of acrylic to establish contour and marginal adaptation.
19. Figure 18. Final first premolar restoration cemented to place.
20. Figure 19. Partial displacement of excess cement using laboratory analog prior to
cementation.
21. Figure 20. ITI Wide Neck abutment.
22. Figure 21. Final restoration showing a more favorable emergence contour achievable
with widerimplant (Tooth #31 was periodontally compromised).
23. Figures 22, 23. Very narrow restorations on the ITI Narrow Neck abutments.
24. Figure 24. Soft tissue that has been sculpted by a properly contoured provisional
crown.
25. Figure 25. Provisional restoration veneered with microfill composite resin.
26. Figure 26. Ceramo-metal custom abutment on tooth #8.
27. Figure 27. Final ceramo-metal crown cemented on the custom abutment shown in
Figure 24.
Ten Years of Patients'
Experiences With
Fixed ImplantSupported Prostheses
By Gun Sandberg, RDH, MSci; Torsten Stenberg, DDS, PhD; and Karin Wikblad, PhD
Abstract
Purpose. This study investigated patients' perceptions of fixed implantsupported
prostheses (ISP) in totally edentulous jaws in order to obtain a broader base for patient
information.
Methods. A total of 135 patients who had received prosthetic rehabilitation
treatment responded to a questionnaire on oral functions, speech, oral selfcare,
esthetics, lifestyle changes and selfconfidence, oral comfort, and overall satisfaction
with ISP. The patients also listed positive and negative experiences with the ISP.
Results. Most patients (97%) reported overall satisfaction. Chewing ability was
rated as good or very good by all but one (99.3%). Twentysix patients (19.6%) identified
bruxing and clenching habits; these were significantly younger than those free from
problems. Phonetic problems were reported by 32.8% after insertion, with 18.6% (eight
patients) having remaining problems after seven to 10 years. Most of the patients (87.2%)
found it easy to clean the prosthesis. Improved lifestyle after ISP insertion was
reported by 75% and increased selfconfidence by 82% of the patients. Improvements were
especially perceptible in social situations that involved conversation or eating. None of
the measured variables was related to duration of having ISP.
Conclusions. The patients' experiences in this study lasted over a period of 10
years, thus their positive and negative aspects can serve as information support for
dentistry to enable future ISP patients to make appropriate choices. The
information could be made available to patients by including in a patienttargeted
booklet.
Keywords. Implantsupported prosthesis, patient satisfaction, oral function,
oral self care, esthetics, lifestyle, selfconfidence, patient information.
v Introduction
Today edentulous patients can choose among several types of tooth replacement
treatment. However, to make the right choice, they must have adequate information.
Technical information is easy to provide but is not sufficient for decision making. There
is a need for complementary information on patients' satisfaction and experiences in
wearing a certain type of prosthesis.
The aim of the current study was therefore, to document patient experiences and
perceptions of wearing implantsupported prostheses (ISP) over a period of 10 years in
order to obtain an extended knowledge base for patient information.
v
Review of the Literature
Earlier, the only treatment of toothlessness was a removable denture. A new era in
tooth replacement treatment began when Brånemark published the results of 10 years'
treatment with titanium implantsupported dental prostheses in more than 200 patients.1
Since its introduction in 1965, the Brånemark implant system has shown a high rate of
success for ISP in totally edentulous jaws.7
Successful ISP treatment is dependent on biological, psychosocial, functional,
technical, and constructional factors.5 Jemt followed, in a retrospective
study, 391 edentulous patients consecutively treated with ISP from the time of prostheses
placement to the first annual checkup.6 The overall success rate was 98.1% and
99.5% for the implants.
Oral Functions
Over a threeyear period, oral functioning in patients rehabilitated by maxillary ISPs
was evaluated in a longitudinal investigation.7 Additionally, a questionnaire
solicited patients' subjective evaluation of the effect of the therapy. All patients were
pleased with the oral rehabilitation, and the ISP treatment led to increased oral
functions. e.g., chewing comfort.
In a retrospective study, patient satisfaction and maintenance issues for 156 patients
were evaluated.7 Patients were asked to rate oral functions and overall
satisfaction by use of visual analogue scales. Information on maintenance was collected
from dental records. Despite a number of repairs needed within the first year, patients
indicated a high level of overall satisfaction with their oral functions.
In a threeyear followup study patients participated in a survey.9 Patients'
opinions were obtained by questionnaires using sixgrade scales ranking from negative to
positive or
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
never to always. The patients were given the questionnaire at the first recall
interval within four months, and again after three years to elucidate the long-term
effects of the reconstructions. The patients were very satisfied with the oral functions,
and chewing ability improved significantly during the three years after treatment. Nearly
all patients said that they would undergo the treatment again or recommend it to others.
Speech and Phonetics
Haraldsson investigated 19 randomly selected patients and found that about half of the
edentulous patients experienced speech difficulties immediately after having had ISP, but
mainly during the first weeks or months after treatment.'° Twentyone individuals treated
with fixed ISP in the maxilla were evaluated in two studies.2 In one study,
registrations were made when the patients wore complete removable dentures in the upper
jaw, and three to six months after they had been treated with ISPs in the maxilla. These
patients were reexamined after three years.12 The results indicated that,
after initial problems, 94% of the individuals considered themselves to be free from
speech problems at a three-year followup, while 6% did not.
Jemt reported clinical problems encountered during a fiveyear period for a group of 76
patients treated with fixed ISPs.3 Speech problems was the most frequent
complaint during the first year. When Jemt studied 391 edentulous patients treated with
ISP during one year from the time of prostheses placement, he stated that problems
involving speech were obviously related to time.6 Onethird of the patients had
phonetic problems immediately after treatment, but only 13% had remaining problems after
one year. The patients' adaptation by increasing lip pressure to prevent air leakage
reduced the speech problems.
Oral SelfCare
Difficulties in cleaning the prosthesis also seem to be a problem, and patients have
reported less satisfaction with the oral selfcare associated with the prostheses.
Walton's retrospective study on patient satisfaction and maintenance found a high level
of overall satisfaction with the ISPs. The only exception was limited satisfaction with
the cleansibility of the fixed ISPs.
Psychological and Social Factors
Improved psychological and social functions, quality of life, self-confidence, and
satisfaction of patients after insertion of ISP have been reported. Twentysix patients
were examined pre and postoperatively after three months, and again after two years, in
two controlled studies.14, 15 The majority of these stated that their lives
had improved significantly; that they had regained selfconfidence; and that in contrast
to patients having
worn a conventional removable denture, they accepted the ISP as a part of themselves.
These results have been supported by others who have stated that qualityoflife factors
associated with ISP may be important for understanding the success of implantology.15,
16 A survey study that compared status before and after ISP therapy suggested that
patients' attitudes toward their dental health improved significantly after treatment
with ISPs.17 Harle studied 46 female patients in a survey to assess the impact
of ISP and conventional removable dentures on relative health status.18 The
data demonstrated that, for some patients, there were clinically important advantages of
ISP in terms of improved physical, psychological, and social functioning.
Very little is known, however, about patients' longterm experiences, and some of the
studies mentioned above included few subjects. Thus, a larger study was needed to measure
patients' experiences over a longer period of time to be able to give impartial
information to patients choosing a treatment from among options.
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
v
Materials and Methods
A crosssectional design was used and data were collected from dental records and by
use of questionnaires mailed to patients who had received fixed ISP during a 10-year
period.
Sample
To control for constructional and technical factors, only patients treated by one
specific prosthodontist at a prosthodontic clinic in Sweden during a 10year period were
selected. A total of 148 patients had received prosthetic rehabilitation treatment with
fixed ISP during the 10year period from this prosthodontist. The group consisted of 60
males and 88 females ranging in age from 36 to 90 years (mean age 66.9 years, SD 10.2).
Measurements
A modified version of questionnaires shown to have good validity and reliability in
earlier epidemiological studies was used in the data collection.7, 19 The
modified questionnaire also was tested in a pilot study among a group of adult and
elderly people. It consisted of 29 items in the following areas.
- • Oral functions were measured, including chewing ability and
parafunctional phenomena such as bruxing, clenching, and fatigue/stiffness in the
temporomandibular joint.
- • Speech and phonetics were assessed by questions on speech and
conversation in general, and on specific difficulties in expressing different sounds.
A timeaspect on perceived speech problems also was included to assess how long it
took for patients to adjust to any difficulties experienced after insertion of ISP.
- • Oral selfcare was assessed with questions about the information the
patient received on how to care for the ISP, and difficulties experienced in cleaning
them.
- • Esthetics was measured as satisfaction with the esthetics of ISP and
overall patient appearance compared to appearance prior to ISP insertion.
- • Lifestyle changes and selfconfidence were assessed with questions on
habits; e.g., covering of the mouth during social interaction, level of
self-confidence compared to the time prior to ISP insertion, and lifestyle changes in
general.
- • Oral comfort levels before and after insertion of ISP were compared with
the use of a 10point visual analogue scale (VAS) and openended questions on different
aspects of oral comfort.
- • Overall satisfaction was rated on a scale ranging from very satisfied to
very dissatisfied and by means of an open ended question.
- • An additional question on most positive and most negative experiences with
ISP also was included.
Besides data from the questionnaire, the following data were collected from the dental
records:
- - location and reasons for ISP selection
- - number of implants
- - year of treatment
Procedure
Data were collected by a dental hygienist. Names and addresses of the 148 patients
were obtained from the prosthodontic clinic. The prosthodontist who had treated the
patients did not participate in the data collection. Questionnaires were mailed to the
148 patients, along with a letter informing them about the purpose of the study and its
voluntary nature. After one reminder, 135 (91.2%) of the patients responded.
Dropout analysis was undertaken to ascertain the reason for lack of response by 13 of
the subjects. Of them, six had died, two had been admitted to hospital, two felt
themselves too old and too tired to fill in the questionnaire, one had forgotten to fill
in the questionnaire, and two could not be reached.
Data Analysis
The computer program Statview 4.5 was used for all data analyses. To isolate time
related differences, the sample was divided into four subgroups: one to two, three to
four, five to six, and seven to 10 years after ISP insertion. Depending on data type,
results are presented as median values with range or mean values with standard
deviations. Answers to openended questions were categorized with reference to
similarities and differences in the answers. Group comparisons were made by use of ANOVA
for continuous data and c2 tests for discontinuous: p< 0.05 was regarded as
statistically significant.
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
v
Result
Demographic and Clinical Characteristics
Responses were received from 135 patients, 53 males and 82 females, ranging in age
from 44 to 90, with an average of 67 years (SD 9.7). A total of 768 implants had been
inserted, 38.9% in the maxilla and 61.1% in the mandible. Reasons for ISP selection over
removable dentures were patient preference in 34% and functional problems (e.g.,
prosthesis fits loosely, chewing and speech difficulties) in 63.3% of the patients. In
the remaining 2.7%, the reason was unknown. Seventyone (52.7%) of the patients were
totally edentulous in both jaws and wore conventional removable prostheses; 23.3% wore
removable prostheses in one jaw and retained their own teeth in the other. Twentyfour
percent had caries and periodontitis without any earlier experiences of wearing
prostheses. The patients had ISP for 4.8 years as a mean (SD 2.5 years, range one to 10
years). To be able to detect problems that may be timerelated, the patients were divided
into four groups according to length of time wearing ISP. Demographic and clinical
characteristics in the four groups are shown in Table I.
Oral Functions
The questions in this area included the ability to masticate food and types of food
that were difficult for the patient to masticate. Chewing ability was rated as good or
very good by all patients but one (99.3%). Most (86.4%) reported that they ate all types
of food. Some food, however, was so difficult to chew that 13.6% avoided it. Food that
was avoided included hard bread, stringy meat, raw vegetables, apples, and nuts. There
were no differences in chewing ability among the four subgroups (Table II). Neither were
age (F=0.25, DF=2/130, p= 0.8) or gender differences (c2=0.87, DF=2, p=0.65)
found in this respect.
Bruxing and clenching habits were identified by 26 patients (19.6%), and 10 (7.6%)
experienced a sense of fatigue or stiffness in the temporomandibular joint. The patients
who reported bruxing and clenching habits were significantly younger (61.5 years. SD 9.5)
than those free from such problems (68.7 years, SD 9.5; F=5.75, df=2/130,p= 0.004), but
no significant differences were found that could be related to time wearing ISP (Table
II.). Twentyfive patients were not aware of whether they had bruxing and clenching
habits.
Table I. Demographic and Clinical Characteristics of 135 Patients in Relation to
Length of Time Wearing ISP
Length of time wearing ISP
Characteristics 12 years 3-4 years 5- 6 years 710 years
Age (years±SD) 66.3±8.6 67.6±9.0 66.4±11.6 67.1.±9.9
Male/Female (number) 8/15 24/25 12/20 9/22
ISP location:
maxillary (number) 6 15 8 5
mandibular (number) 15 28 20 19
both jaws (number) 2 6 4 7
Length of time
wearing ISP (years±SD) 1.6±0.5 3.47±0.5 5.41±.05 8.58±0.92
Speech and Phonetics
Fortythree (32.8%) patients encountered phonetic problems after implant insertion,
with eight (18.6%) having remaining problems after seven to 10 years. Differences were
found between maxillary and mandibular prostheses, in that those with maxillary
prostheses reported significantly more speech problems (c2= l 9.36, DF=27
p=0.000 1). Speech problems did not significantly decrease with time lapsed since
treatment (Table II). The most common problem was pronouncing the esound and variations
such as sj, sch, ski, st, and str. Other difficult sounds were b, d, f, j, and r.
Respondents commented in the following way regarding their difficulties.
- - I sound like a frog.
- - I lisped in the beginning.
- - I still have a whistling sound.
- - I can no longer whistle, but it doesn't matter.
When asked about their conversation with other people, 69.4% reported that
conversation was easier to manage after ISP, 28.2% found no difference compared to the
time prior to insertion of ISP, and 2.4% found it more difficult than before to speak
with others. This did not seem to be related to time lapsed since ISP insertion (Table
II). No age (F=0.2, DF=2/121, p=0.82) or gender differences (c2=0.16, DF=2,
p=0.69) were found.

Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
Oral SelfCare
One hundred thirty patients (97.7%) stated that they had received adequate information
on taking care of the prostheses. Most of the patients (87.2%) found it easy to clean the
prostheses; difficulties were reported by 12.8%. Cleaning problems did not decrease
significantly with length of time with ISP (Table II). Age (F=0.78, DF=2/130, p=0.46) or
gender differences (c2=0.36, DF=2, p=0.84) were not found.
Esthetics
Most patients (94.3%) indicated satisfaction with the esthetics of their ISP, 5.2%
were neither satisfied nor dissatisfied, and 0.5% reported dissatisfaction. Significant
differences were not found among the four groups (Table III).
Examples of patient's comments are
- _ The teeth could have been longer and bigger.
- _ The color of my teeth was yellowed before.
- _ My upper jaw has shrunk.
- _ When I look into the mirror, I can't believe that my teeth are so beautiful.
- _ I admire my teeth.
When asked about their overall appearance, 49.2% of the patients reported an
improvement, 44.6% answered that the overall appearance was neither better nor worse than
before the insertion, and eight individuals (6.2%) were of the opinion that their overall
appearance had worsened compared to the time prior to ISP insertion. Satisfaction or
dissatisfaction with esthetics did not correlate with the length of time they had ISP
(Table III). No age (F=0.91, DF=3/128,p=0.44) or gender differences (c2=2.73.
DF=3, p=0.44) were found.
Table II. Percentage of Patients Reporting Absence of Problems With Oral Functions,
Speech, and Oral Self-Care (n=135)
Length of time wearing ISP

Measured 1-2 years 3-4 years 5-6 years 7-10 years
variables % of n=23 % of n=49 % of n=32 % of n=31 Statistics
Oral functions
Good chewing ability 100.0 100.0 96.8 100.0 c2(3)=3.32 p=0.3
Can eat all kinds of food 86.4 87.5 87.1 83.9 c2(3)=.23 p=0.9
Absence of bruxing/clenching* 81.0 75.0 71.4 79.0 c2(3)=0.71 p=0.9
Absence of fatigue/stiffness 86.4 95.9 86.7 96.8 c2(3)=4.27 p=0.2
Speech
Absence of phonetic problems 56.5 68.1 67.7 73.3 c2(3)1.72 p=0.6
Conversation easier 76.2 66.0 69.0 70.4 c2(3)=0.73 p=0.9
Oral self-care
Absence of cleaning problems 82.6. 87.5 87.1 93.6 c2(3)=1.57 p=0.7
*Twenty-five patients were not aware of whether they had bruxing and clenching habits.
Life-Style Changes and Self-Confidence
Improvement in lifestyle related to the ISP was reported by 74.2% of the patients
while 25% did not experience any such changes and one individual experienced
deterioration. In a further question, patients were asked if they tended to cover the
mouth during social interactions. One hundred nineteen patients (90.8%) reported that
they never did this, whereas eight (6.1%) said that they sometimes did, and four (3.1% )
answered that they
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
often did. When asked about the level of self-confidence they felt since the insertion
of the ISP, 82.4% identified an improvement compared with the time prior to ISP
insertion. Twenty-three (17.6%) did not experience any changes in self-confidence and no
correlation was found with length of time wearing ISP (Table III). No age or gender
differences were found.
Patients commented that they had stronger self-confidence and a renewed enthusiasm for
life. Comments included
- _ Now I can go traveling.
- _ I can be social together with others again.
- _ I can speak in front of a group of people.
- _ I dare to laugh.
- _ I can kiss.
Table III. Percentage of patients reporting positive influence of ISP on esthetics,
improvement in life-style and self-confidence (n= 135)
Length of time wearing lSP

Measured 1-2 years 3-4 years 5-6 years 7-10 years Statistics variables % of n=23 % of
n=49 % of n=32 % of n=31
Satisfied with
esthetics of ISP 95.7 97.9 90.3 90.3 c2(3)=2.97 p=0.4
Improved overall 50.0 51.0 44.8 50.0 c2(3)=0.3
appearance p=0.96
Improved lifestyle 77.3 70.2 79.3 73.3 c2(3)=0.91 p=0.8
Never covering the mouth 87.0 93.6 93.3 87.1 c2(3)=1.6
during social interactions p=0.7
Improved self-confidence 91.3 77.1 83.3 83.3 c2(3)=2.23 p=0.5
Oral Comfort
Patients demonstrated high level of oral comfort on the 10-point VAS scale (=9.2; SD
1.3). Both females (53. l %) and males (67.3%) rated their oral comfort after ISP
insertion higher compared to the time prior to insertion. Comments like "lt has been
good all the time" and "there is no difference"' were frequent in the
open-ended questions related to oral comfort.
Overall Satisfaction
One hundred twenty-nine patients (97.7%) reported that they were generally satisfied,
two that they were neither satisfied nor dissatisfied, and one patient felt dissatisfied
with ISP. No significant relation was found between satisfaction and length of time
wearing ISPs (c2=9, p=0.5). Examples of patient comments in this area:
- _ This technique is a miracle, a wonder.
- _ This is the best thing that has happened to me.
- _ I should have done this 10-15 years ago.
Positive and Negative Experiences of the ISP
The responses to the open-ended questions regarding the most positive and the most
negative experiences with the ISP were categorized as follows (the categories are
exemplified by patient quotations).
Positive aspects:
a. Self-confidence/Safety
- - My self-confidence is really increased.
- - To be able to eat, shout, and laugh without flopping dentures makes me feel
very safe.
b. Function
- No problems with chewing.
- I don't have sores or pain in my mouth anymore.
c. Appearance
- Wonderful to have teeth in my mouth.
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
- My teeth are so beautiful.
d. Psychosocial
- I'm not afraid of having dinner at a restaurant.
- I'm able to live a normal life again.
- To lose one's teeth is a tragedy—now the joy of living has returned.
The most frequent positive comments included increased self-confidence and that the
connection of the prosthesis to implants gave increased safety.
Negative aspects:
a. The treatment
- The treatment was hard and l was terrified that it could turn out to be a
failure.
- It was a hard and tedious procedure.
b. Cleaning
- It's hard work to keep them clean.
- The cleaning is time consuming.
c. Speech
- I cannot pronounce certain words.
d. Appearance
- _ My ISP looks so clumsy/ my teeth have become too conspicuous.
- _ My face has changed/l have an odd look since I got the ISP.
e. Economy
_ It is too expensive.
f. Technical problems
- - The screws get loose.
g. Miscellaneous problems
- _ Frequent inflammations in the gingiva.
- _ The teeth are soon worn down.
- _ The teeth become discolored.
- _ All food that gets stuck between the screws is really a problem.
Thirtytwo patients reported that they were not able to identify any negative aspects
of ISP. Most negative comments related to the surgery in itself and particularly the
periods between the different stages in the treatment. Ten patients felt that the ISP had
a negative impact on their appearance, e.g., because of wrong length and wrong color of
the teeth.
To the question "If you get the opportunity to choose the type of prosthesis
today, would you make the same choice?" 94.6% of the patients answered
"yes."
v Discussion
In order to obtain an extended knowledge base for patient information, the present
study focused on the importance of evaluating patients' longterm experiences and
perceptions about their implant-supported prostheses (ISP). Responses were received from
135 patients (91.2%) who had been treated with implant therapy in totally edentulous jaws
during a 10year period. These patients' own opinions—their positive and negative
findings—may serve as support for impartial information to others when they have to
choose a type of treatment.
Most of the patients stated that prior to the ISP insertion they had had oral problems
often and for a long time, and the main reason for ISP selection was to alleviate the
functional problems experienced.
The patients' chewing ability improved after insertion of ISP and remained good
throughout the 10 years. Other studies also have found similar improvement of oral
function after insertion.79 All patients but one (99.3%) rated chewing ability
as good or very good, and most of them (86.4%) could chew all types of food. A sense of
fatigue was reported in 7.6%, and bruxing and clenching habits were present in onefifth
of the patients, and were significantly more frequent in younger patients than in the
elderly.
Phonetic problems were encountered by onethird of the patients but decreased over
time, and one-fourth had remaining problems. After seven to 10 years, 73. 3% of the
patients in this study reported absence of phonetic problems. The problems were
significantly more prominent in patients with maxillary prostheses. This is in accordance
with other findings.16, 12 Jemt found that speech problems were the most
frequent ISP
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
complication in maxillary ISP during the first year after insertion.13
Others also have reported speech problems directly after ISP insertion.6, 10, 12
The problems decreased to l3% after one year in the study by Jemt.6 Lundqvist,
et al. on the other hand, found that, after initial problems, 94% considered themselves
free from speech problems after three years with ISP.12 In this study eight of
the patients ( 18.6%) had remaining problems after seven to 10 years. In the subgroups
three to four years and five to six years respectively, 31.9% and 32.3% of the patients
had remaining problems. Those figures are much higher than in other studies.
Lundqvist studied 21 subjects for three years, and Jemt 391 patients during one year.
Thus, the results of those studies cannot be compared directly to this study. The method
of this study, with the clinician not addressing the patients or signing the
questionnaires, probably made the patients more willing to give impartial answers.
Respondents commented on their difficulties in response to the openended questions,
and the most common problem was pronouncing the ssound. This was in accordance with
earlier findings.6, 12 When asked about their conversation with other people,
69.4% reported that it was easier to speak with others after ISP insertion than before.
This did not seem to be related to time lapsed since ISP insertion.
Most patients (97.7%) reported that the information received regarding selfcare
directions was adequate. In addition, 87.2% found it easy to perform selfcare procedures.
This result is not in accordance with data obtained by Walton, who found that cleaning
difficulties were experienced by 44% of subjects.8 All patients in this study
received dental hygiene care prior to and after the ISP insertion; thus, the diverging
results could be due to quality of instructions given. It might be of interest to
investigate this aspect further.
Very high levels of oral comfort after ISP insertion (x=9.2 on a 10-point VAS scale)
were reported. The tendency that oral comfort may increase with length of time wearing
ISP is probably due to adaptation to the fixed ISP over time, and is perhaps also a
matter of memory in that it was probably not possible to remember how the ISP had felt 10
years ago. Most patients reported satisfaction with the esthetics of their ISP, and only
1% was dissatisfied. Regarding general appearance, many of the patients reported positive
opinions, and 94.3% were satisfied with the esthetics of the ISP. The tendency towards
less satisfaction in patients who had received their fixed ISP many years ago can
probably be explained by the need for repair and remaking of the fixed ISP, in some cases
due to worn or discolored constructions. However, when asked about overall appearance
49.2% reported an improvement, and 44.6% indicated that their overall appearance was
neither better nor worse than before ISP. The patients may have been aware of changes but
not felt comfortable commenting on their own overall appearance.
Satisfaction or dissatisfaction with esthetics did not correlate with length of time
wearing ISP.
Lifestyle improvement was reported by approximately 75% of the patients, and increased
self-confidence by 82%. This was especially perceptible in social settings including
conversation or eating. The positive changes in quality-of-life factors and confidence
are supported by other studies.14-18
The overall effect variable indicated that the patients were satisfied (97.7%) with
their ISP and is in accordance with earlier findings.9, 15, 18 The patients'
negative comments in this study, even if they were few, suggest that dentistry still has
some technical and information issues to address when providing individualized patient
care. Kerschbaum suggested that the difficulty in addressing the question about
satisfaction results from its multifactorial nature including biological, psychological,
and technical factors; and the fact that a patient seldom has the opportunity to compare
his or her treatment with relevant alternatives.5 The current study supports
this approach, as a combination of variables was found to have an impact on the patient's
level of satisfaction. Guckes, et al. suggested that future research should include
outcome measures beyond implant prosthesis survival to assess more fully the practical
impact of dental implants on the patient's oral health.20 It is, however,
important to supply patients not only with technical information, but also with
complementary information on what it is like to live with a certain type of ISP. This is
an important area for dental hygienist involvement.
The results of this study about patients' experiences, positive and negative, can
serve as information support for dentistry to enable potential ISP patients to make
appropriate choices. The dental hygienist is, today to a greater extent than earlier,
involved in the ISP treatment_above all before as well as after the technical treatment.
Therefore, the dental hygienist needs to know of many aspects of patients' satisfaction
and experiences in living with a certain type of prosthesis. To make the information
available to patients, it could be included in a patient-targeted booklet. The booklet
could include a list of quotations on positive and negative experiences, together with
data on patients' experiences in wearing ISP.
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
Conclusions
A combination of variables was found to have an impact on the high level of
satisfaction with ISP. This study encompasses 10 years of patient experiences; thus,
their positive and negative experiences can serve as information support to enable future
ISP patients to make appropriate choices. It is important to supply patients not only
with technical information, but also with complementary information on living with a
certain type of ISP. Such information could be made available to patients by the dental
hygienist.
Acknowledgment
Funding was obtained from Dalarna Research Institute, Falun, Sweden. Gun Sandberg, RDH,
MSci, is registered tutor at the dental hygiene program; and Karin Wikblad, PhD, is
associate professor, and senior lecturer; both at Dalarna University College, Falun,
Sweden. Torsten Stenberg, DDS, PhD, is prosthodontist and chief dentist in prosthodontics
at Falun Center of Oral Rehabilitation, Department of Public Dental Health, County of
Dalarna, Sweden.
References
1. Brånemark P-I, et al.: Osseointegrated implants in the treatment of the edentulous
jaw. Experience from a 10 year period. Scand J Plast Reconstr Surg 1977;16:1-132.
2. Brånemark P-I Zarb G, Albrektsson B: Introduction to osseointegration. Osseointegration
in Clinical Dentistry. (Chaps 1). Chicago, Quintessence Publ. Co, 1985.
3. Adeli R, et al.; A long-term follow-up study of osseointegrated implants in the
treatment of totally edentulous jaws. Int J Oral Maxillofac Impl 1990-5:347-58.
4. Albrektsson T, Zarb G, Worthington P, Eriksson P: The long-term efficacy of
currently used dental implants: A review and proposed criteria of success. Int J Oral
Maxillofac Implants 1986;1: 11-25.
5. Kerschbaum T: Long-term prognosis of conventional prosthodontic restorations. In:
Naert. Steenberghe v. Worthington (eds.): Osseointegration in Oral Rehabilitation.
London, Quintessence Publishing Co.1993;3 3-49.
6. Jemt T: Failures and complications in 391 consecutive insert fixed prostheses
supported by Brånemark implants in edentulous jaws. A study of treatment from time of
prosthesis placement. Oral Maxillofac Implants.
7. Lundqvist S, Haraldson T: Oral function in patient's wearing fixed prosthesis on
osseointegrated implants in the maxilla: 3-year follow-up study. Scand J Dent Res 1992;
100(5):279-83.
8. Walton JN, MacEntee Ml: Problems with prostheses on implants: A retrospective study.
J Prosthet Dent 1994;71 :283 288.
9. DeBroyn H, Collaert H. Linden B, Björn, A: Patient's opinion and treatment outcome
of fixed rehabilitation on Brånemark implants. A 3-year follow up study in private
dental practices. Clin Oral Impl Res 1997;8:265-271.
10. Haraldson T, Carlsson GE: Bite force and oral function in patients with
osseointegrated implant bridges. Scand J Dent Res 1977;36:200-208.
11. Lundqvist S, Lohmander-Agerskov A. Haraldson T: Speech before and after treatment
with bridges on osseointegrated implants in the edentulous upper jaw. Clin Oral Impl
Res 1992;3:57-62.
12. Lundqvist S, Haraldson T, Lindblad P: Speech in connection with maxillary fixed
prostheses on osseointegrated implants: A three-year follow-up study. Clin Oral Impl
Res 1992;3(4):176-80.
13. Jemt T: Fixed implant-supported prostheses in the edentulous maxilla. A five-year
follow-up report. Clin Oral Implants Res 1994;5(3): 142-7.
14. Blomberg S, Lindkvist L: Psychological reactions to edentulousness and treatment
with jawbone-anchored bridges. Acta Psychiatr Scand 1983;58:251 -262.
Ten Years of Patients' Experiences With Fixed Implant-Supported Prostheses
15. Blomberg S: Psychological response. In: Brånemark PI, Zarb GA, Albrektsson T
(eds.): Tissue-Integrated Prosthesis. Osseointegration in Clinical Dentistry.
Berlin, Quintessence Publishing Co., 1985:165-174.
16. Karlsson S, Carlsson GE: Oral motor function and phone in patients with
implant-supported prostheses. In: Naert, Steenberghe v, Worthington P (eds.):
Osseointegration in Oral Rehabilitation. London, Quintessence Books, 1993:123-131.
17. Grogono AL, Lancaster DM, Finger IM: Dental implants: a survey of patients'
attitudes. J Prosthet Dent 1989; 62(5):573-6.
18. Harle TJ, Anderson JD: Patient Satisfaction with Implant-Supported Prostheses.
Int J Prosthodont 1993;6:153-162.
19. Karlsson G: Halsoekonomisk analys av dentala implantat (thesis). Department of
Health and Society, Linkoping University Sweden, 1991.
20. Guckes A, Scurria M, Shugars D: A conceptual framework for understanding outcomes
of oral implant therapy. J Prosth. Dent 1996;75(6):633-639.
Copyright The Journal of Dental Hygiene. Volume 74, Issue III, Summer 2000.
Reprinted with permission.
Dental Implants:
Patient Information
Life's simple pleasures can cause problems and pain for the millions of adults who
suffer from permanent tooth loss.
Men and women of all ages are selfconscious about their dentures, bridges or missing
teeth. Some have difficulty speaking because their dentures slip or click.
For others, the irritation and pain caused by dentures are constant reminders of the
limitations they feel. Many are concerned about their appearance and may feel that their
tooth loss has ``aged them" before their time.
Some regularly decline invitations to social events because they are unwilling to face
the uncertainties of eating, speaking and laughing in public. Many can no longer enjoy
their favorite foods, nor the social interaction with family and friends that accompanies
special meals.
v
A Unique Solution to a Troublesome Problem
Now, more and more people are putting an end to these problems by choosing dental
implants, a revolutionary way to replace missing teeth. Dental implants offer an
excellent alternative to the limitations of conventional dentures, bridges and missing
teeth.
Dental implants are changing the way people live. With them, people are rediscovering
the comfort and confidence to eat, speak, laugh and enjoy life.
Why Are People Choosing Dental Implants?
A national survey of oral and maxillofacial surgeons found that patient interest and
demand has grown significantly.
The survey found:
- n Dental implant use has nearly tripled since 1986 and is expected to continue to
rise rapidly.
- n People of all ages are turning to dental implants to replace a single tooth,
several teeth or a full set of dentures.
- n Leading reasons cited for choosing dental implants are:
- • to restore normal eating and speaking abilities.
- • to enhance facial appearance and confidence.
- • to increase denture retention.
According to the survey, the reasons for the increased demand are:
- n Growing public awareness of the significant functional and esthetic advantages of
dental implants over conventional dentures and bridges
- n The availability of data on the longterm success of dental implants
Experts predict that the demand for the procedure will continue to grow as people
become more familiar with the benefits of dental implants.
Dental Implants: Patient Information
v
An Alternative to Natural Teeth
Dental implants are a great option for patients missing natural teeth, because they
act as a secure anchor for artificial replacement teeth and eliminate the instability
associated with surface adhesives and removable bridges.
Your natural teeth absorb biting pressure of up to 540 lbs. per square inch. Longtime
denturewearers can often absorb no more than 50 lbs. per square inch. Dental implants,
when properly placed, can withstand 450 lbs. per square inch of biting pressure.
Dental implants are made of materials that are compatible with human bone and tissue.
The subperiosteal implants are surgically placed directly into the jawbone. Small posts
are then attached to the implants which protrude through the gums. These posts provide
stable anchors for artificial replacement teeth.
Based on patient needs, a single tooth, a partial bridge or a full set of replacement
teeth are fitted to the implants and locked in place over the protruding posts. In
appearance and in function, implants are the closest thing to natural teeth and a good
alternative to conventional dentures.
Implants eliminate the daytoday frustrations and pain of illfitting dentures. They
allow people to enjoy a healthy and varied diet without the restrictions many denture
wearers face. With a sense of renewed selfconfidence, many people rediscover the
excitement of an active lifestyle shared with family and friends and the chance to speak
clearly and comfortably with coworkers.
For all these reasons, people with dental implants often say they feel better . . .
they look better . . . they live better.

partially edentulous
v
What to Expect
An oral and maxillofacial surgeon can determine if you are a candidate for dental
implants. You will be evaluated based upon a number of things including dental health,
lifestyle, jawbone quality and oral hygiene habits. In close consultation with your own
dentist, the oral and maxillofacial surgeon can plan your dental implant treatment
program.
Dental implant surgery is often done in an oral and maxillofacial surgeon's office. In
some cases, the procedure is done in a hospital or ambulatory surgery center. In any
event, an oral and maxillofacial surgeon can determine the most appropriate setting based
on your individual needs.
A TwoPhase Procedure
For most patients, the placement of dental implants involves two surgical procedures.
First, the implants are surgically placed into your jawbone. These small devices make up
the framework needed to securely hold replacement teeth. For the first three to six
months following surgery, the implants are beneath the surface of the gums, gradually
bonding with the jawbone. During this time, you should be able to wear temporary dentures
and eat a soft diet.
Some patients do report minor pain and swelling immediately after the procedure but
most experience no change in their daily routines.
While the implants are bonding with the jawbone, new replacement teeth are fashioned
by your dentist. The replacement teeth must clip onto the implants, fit securely in the
mouth and withstand the daytoday movement and pressure created by chewing and speaking.
So, it is important that they are created by a dentist with proper training in
restorative techniques.
Once the implants have bonded to the jawbone, the second phase of the procedure
begins. At this time, the oral and maxillofacial surgeon uncovers the implants and
attaches small posts which will act as anchors for the artificial teeth. The posts
protrude through the gumline but are not visible when artificial teeth are attached.
The entire process, from evaluation to completion, generally takes six to eight
months. During this time, most patients do not experience any disruption in their normal
business and social activities.

totally edentulous
Dental Implants: Patient Information
Because dental implants are made of materials that are compatible with human bone,
there is little chance for an allergic reaction in the body. However, implants can fail
when proper oral hygiene techniques are not used. Dental implants require special
individual care. Proper brushing, flossing, rinsing and regular checkups are critical to
the longterm success of your implants.
v
A Team Effort
Though dental implants are a relatively simple procedure, they generally warrant the
expertise of two dental professionals_ an oral and maxillofacial surgeon and a
restorative dentist.
Working as a team, the oral and maxillofacial surgeon and restorative dentist can
determine if you are a candidate for implants and design an appropriate treatment plan. A
restorative dentist, with training in dental implants, creates the replacement teeth. The
doctor prepares the necessary molds and works with a dental laboratory to make sure that
the denture or bridge will meet the particular needs of each patient. Additionally,
dental implant patients should see a dentist for routine follow-up care and maintenance.
An oral and maxillofacial surgeon is a dental specialist who surgically treats the
mouth and jaw area. Following dental school, an oral and maxillofacial surgeon completes
several additional years of training in a hospital residency program and is trained to
administer and monitor all types of anesthesia needed for oral and maxillofacial surgery
procedures.
Start a New Way of Living Today
If you are among the millions of Americans who suffer from permanent tooth loss, you
can eliminate the problems and pain caused by dentures, bridges or missing teeth. You can
begin to rediscover the joy of eating healthy, speaking clearly and laughing comfortably.
Source: American Association of Oral and Maxillofacial Surgeons
9700 W. Bryn Mawr Avenue
Rosemont, IL 60018-5701
(847) 678-6200 Fax (847) 678-6286
www.aaoms.org